Colostomy Creation
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is colostomy creation?
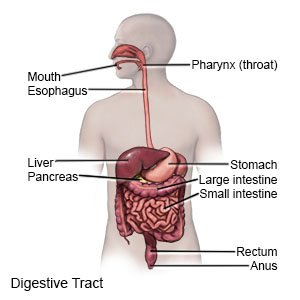
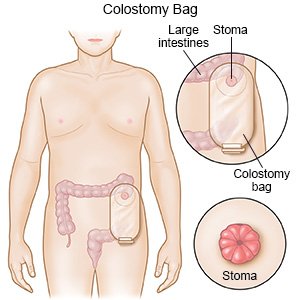
Colostomy creation is surgery that brings part of your colon (bowel) to the surface of your abdomen. This creates a small opening in your abdomen called a stoma. Bowel movements pass through the stoma and into a pouch that is attached to your abdomen.
 |
Why do I need a colostomy?
Colostomy creation is often done to remove parts of your colon that are injured or diseased. You may need a colostomy for conditions such as colorectal cancer, diverticulitis, or inflammatory bowel disease (IBD). Trauma to the abdomen may also require a colostomy.
How long will I need a colostomy?
- A temporary colostomy can last from weeks to years. After your colon heals, another surgery closes the stoma and rejoins the sections of your colon. You will have normal bowel movements after the colostomy is closed. Sometimes a temporary colostomy needs to become permanent.
- A permanent colostomy will last a lifetime. You may need a permanent colostomy if parts of your colon have to be removed. A permanent colostomy is also done when parts of your colon no longer work.
What are the types of colostomy?
Your healthcare provider will choose a colostomy type based on the reasons for the surgery and your general health. Types of colostomies include the following:
- An ascending colostomy has the stoma placed on the right side of your abdomen. Liquid bowel movements pass through the stoma.
- A transverse colostomy has the stoma placed in your upper abdomen on the middle or right side. Bowel movements that pass through the stoma are loose or soft. Sometimes you will have 2 stomas next to each other. This is called a loop colostomy. One stoma will pass bowel movements and the other may pass mucus.
- A descending or sigmoid colostomy has the stoma placed on the lower left side of your abdomen. Firm bowel movements pass through the stoma.
Related medications
What will happen when I meet with an ostomy specialist?
Bring a family member or friend with you to learn how to help you. Write down any questions you may have so you will remember to ask them during your meetings.
- The ostomy specialist will talk with you about lifestyle changes that happen with a colostomy.
- The specialist will explain how to prevent problems such as bowel movement leakage. You will learn stoma care to prevent a rash or infection around the stoma.
- The specialist will talk about the supplies you will need for your colostomy. The specialist will show you how to change the ostomy bag. You will also be shown how to irrigate the colostomy. Irrigation is a procedure to empty your bowel by putting liquid into your stoma.
- The specialist may also talk about your nutrition, bathing, and other activities after surgery.
- You may meet other people who have a colostomy.
How do I prepare for a colostomy creation?
- In the weeks before your surgery you will need to do the following:
- Stop taking blood thinning medicines. This includes NSAIDs, such as ibuprofen and aspirin. Your healthcare provider will tell you other medicines to stop taking.
- Meet with your surgeon or ostomy specialist. Your surgeon or specialist will talk with you about the best place for your stoma. A pen or a small disc is used to mark the stoma site on your abdomen. Your surgeon or specialist will ask you to sit, lie down, stand, and bend. This helps position the stoma to prevent leaks and skin problems. It will also help your stoma better fit your clothes and ostomy bag.
- You may be given an antibiotic to prevent an infection. You may need to begin the antibiotic a few days before your surgery.
- Healthcare providers will tell you to stop eating solid foods for 2 to 3 days before surgery. This helps empty your colon before surgery. Ask which foods and drinks are okay. You may be told not to eat raw vegetables or meats such as beef or pork.
- You may be able to only have clear liquids the day before your surgery. You may need a laxative or enema to completely clean out your colon the night before surgery.
What will happen during my surgery?
- General anesthesia will keep you asleep and pain-free during the surgery. For open surgery, your surgeon will make 1 long incision in the middle of your abdomen. For laparoscopic surgery, 3 to 4 small incisions are made on your abdomen. The laparoscopic tools are placed inside the incisions, and your abdomen is filled with carbon dioxide (a gas). The gas lifts the abdominal muscles away from the colon and other organs during surgery. Your surgeon will cut through the muscles in your abdomen to the colon. Your surgeon will carefully check your colon for disease or injury.
- Your surgeon will cut your colon into 2 or more parts. Diseased or injured parts of your colon may be removed. One end of your colon will be pushed through an opening on your abdomen. The end will be stitched to the skin on your abdomen to create a stoma. The other part of your colon may be stitched closed, or a second stoma will be made. You may have a rod placed under the stoma to keep it above your skin if the colostomy has 2 openings. The other incisions are closed with stitches or staples. Your surgeon will attach a pouch around your stoma to collect fluids and bandage your incisions.
- Your rectum and anus may be removed. This will leave a surgery area called a posterior wound. You will have bandages or pads to collect any drainage from the wound.
What should I expect after my surgery?
You will be monitored until you are fully awake. You will have to stay in the hospital for up to a week. During your stay you will learn how to take care of your stoma and the skin around it. You will also learn how to use the ostomy supplies.
What are the risks of a colostomy creation?
- The condition that led to your colostomy may come back, even with treatment. You may develop an infection or bleed more than expected. Surgery may damage nerves or other organs. You may develop a life-threatening blood clot.
- Your stoma may narrow, become blocked, or move too far outside or inside your abdomen. You may develop a hernia (weakness in the muscles in your abdomen). Sometimes the stoma tissue does not get enough blood and the tissue may die. A colon incision may come apart or leak bowel movement fluid into your abdomen. This can cause a life-threatening infection. More surgery and other treatments are needed right away to correct these problems.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
