Chronic Hypertension
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What is chronic hypertension?
Hypertension is considered chronic when it continues for 3 months or longer. Hypertension that continues causes your heart to work much harder than normal, which may lead to heart damage. Even if you have hypertension for years, lifestyle changes, medicines, or both may help lower your blood pressure.
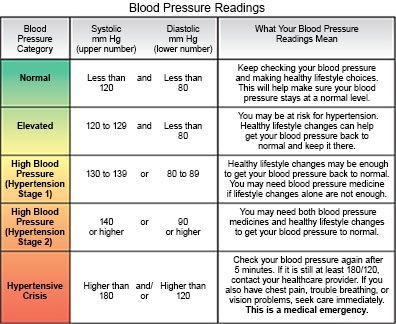
What do I need to know about the stages of hypertension?
Your healthcare provider will give you a blood pressure goal based on your age, health, and risk for cardiovascular disease. The following are general guidelines on the stages of hypertension:
- Normal blood pressure is 119/79 or lower . Your provider may only check your blood pressure each year if it stays at a normal level.
- Elevated blood pressure is 120/79 to 129/79 . This is sometimes called prehypertension. Your provider may suggest lifestyle changes to help lower your blood pressure to a normal level. He or she may then check it again in 3 to 6 months.
- Stage 1 hypertension is 130/80 to 139/89 . Your provider may recommend lifestyle changes, medication, and checks every 3 to 6 months until your blood pressure is controlled.
- Stage 2 hypertension is 140/90 or higher . Your provider will recommend lifestyle changes and have you take 2 kinds of hypertension medicines. You will also need to have your blood pressure checked monthly until it is controlled.
 |
How is chronic hypertension treated?
Your healthcare provider may add, remove, or change any of the following medicines. Do not change or stop taking any of your current medicines without talking to your provider.
- Antihypertensives may be used to help lower your blood pressure. Several kinds of medicines are available. Your provider may change the medicine or medicines you currently take. This may be needed if your blood pressure is often high when you check it at home or you are having other problems with blood pressure control.
- Diuretics help decrease extra fluid that collects in your body. This can help lower your blood pressure. You may urinate more often while you take this medicine.
- Cholesterol medicine helps lower your cholesterol level. A low cholesterol level helps prevent heart disease and makes it easier to control your blood pressure.
Treatment options
The following list of medications are related to or used in the treatment of this condition.
What can I do to manage chronic hypertension?
- Check your blood pressure at home. Do not smoke, have caffeine, or exercise for at least 30 minutes before you check your blood pressure. Sit and rest for 5 minutes before you check your blood pressure. Extend your arm and support it on a flat surface. Your arm should be at the same level as your heart. Follow the directions that came with your blood pressure monitor. Check your blood pressure 2 times, 1 minute apart, before you take your medicine in the morning. Also check your blood pressure before your evening meal. Keep a record of your readings and bring it to your follow-up visits. Your healthcare provider may use the readings to make changes to your treatment plan.

- Manage any other health conditions you have. Health conditions such as diabetes can increase your risk for hypertension. Follow your provider's instructions and take all your medicines as directed. Talk to your provider about any new health conditions you have recently developed.
- Ask about all medicines. Certain medicines can increase your blood pressure. Examples include oral birth control pills, decongestants, herbal supplements, and NSAIDs, such as ibuprofen. Your provider can tell you which medicines are safe for you to take. This includes prescription and over-the-counter medicines.
Related medications
What lifestyle changes can I make to lower my blood pressure?
Your healthcare provider may want you to make more lifestyle changes if you are having trouble controlling your blood pressure. This may feel difficult over time, especially if you think you are making good changes but your pressure is still high. It might help to focus on one new change at a time. For example, try to add 1 more day of exercise, or exercise for an extra 10 minutes on 2 days. Small changes can make a big difference. Your provider can also refer you to specialists such as a dietitian who can help you make small changes. Your family members may be included in helping you learn to create lifestyle changes, such as the following:
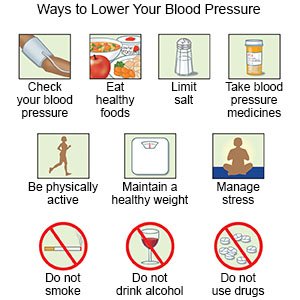 |
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. Some low-sodium foods use potassium salts for flavor. Too much potassium can also cause health problems. Your provider will tell you how much sodium and potassium are safe for you to have in a day. He or she may recommend that you limit sodium to 2,300 mg a day.
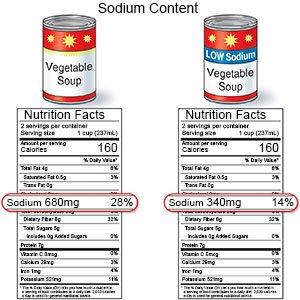
- Follow the meal plan recommended by your provider. A dietitian or your provider can give you more information on low-sodium plans or the DASH (Dietary Approaches to Stop Hypertension) eating plan. The DASH plan is low in sodium, processed sugar, unhealthy fats, and total fat. It is high in potassium, calcium, and fiber. These can be found in vegetables, fruit, and whole-grain foods.

- Be physically active throughout the day. Physical activity, such as exercise, can help control your blood pressure and your weight. Be physically active for at least 30 minutes per day, on most days of the week. Include aerobic activity, such as walking or riding a bicycle. Also include strength training at least 2 times each week. Your provider can help you create a physical activity plan.

- Decrease stress. This may help lower your blood pressure. Learn ways to relax, such as deep breathing or listening to music.
- Limit alcohol as directed. Alcohol can increase your blood pressure. A drink of alcohol is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of liquor. Your provider can help you set daily and weekly drink limits. He or she may recommend no alcohol if your blood pressure stays higher than goal even with medicine or other measures. Ask your provider for information if you need help to quit.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can increase your blood pressure and also cause lung damage. Ask your provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.

Call your local emergency number (911 in the US) or have someone call if:
- You have chest pain.
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
- You become confused or have difficulty speaking.
- You suddenly feel lightheaded or have trouble breathing.
When should I seek immediate care?
- You have a severe headache or vision loss.
- You have weakness in an arm or leg.
When should I call my doctor or cardiologist?
- You feel faint, dizzy, confused, or drowsy.
- You have been taking your blood pressure medicine but your pressure is higher than your provider says it should be.
- You have questions or concerns about your condition or care.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Learn more about Chronic Hypertension
- Do blood pressure drugs interact with alcohol?
- FDA-Approved Weight Loss Drugs: Can They Help You?
- Which Drugs Cause Weight Gain?
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
