Chest Tubes
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about a chest tube:
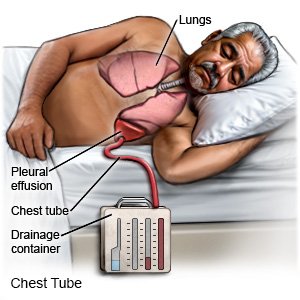
A chest tube is a plastic tube that is put through the side of your chest. A suction device removes air, blood, or fluid from around your heart or lung. This will help you breathe more easily. A chest tube is also known as chest drain or chest drainage tube.
 |
How to prepare for a chest tube to be inserted:
- Your healthcare provider will tell you how to prepare. You may be told not to eat or drink anything for a certain time before your procedure. Your provider may tell you to arrange for someone to drive you home after the procedure.
- Tell your provider about all your current medicines. Your provider will tell you if you need to stop any medicine for the procedure, and when to stop. Your provider will tell you which medicines to take or not take on the day of your procedure.
- Tell your provider if you have any allergies. You may be given antibiotics to prevent a bacterial infection. Tell your healthcare provider if you have ever had an allergic reaction to anesthesia or an antibiotic.
What happens when a chest tube is inserted:
- You may be given general anesthesia to keep you asleep and free from pain during the procedure. You may instead be given local anesthesia or a nerve block. You will be able to feel some pressure during the procedure, but you should not feel any pain.
- Your healthcare provider will make a small incision in your chest. A tool is used to make an opening through the chest muscle. The chest tube is inserted slowly until it reaches the pleural space or chest cavity. Your provider may use an ultrasound to guide the tube into place. When the tube is in place, it will be connected to suction and a drainage system.
- Stitches may be sewn into your chest wall to hold the tube in place. Medical tape may also be used to secure the tube before it is covered with a bandage.
What to expect after a chest tube has been inserted:
- Medicines may be given to relieve pain or prevent a bacterial infection.
- An x-ray or a CT scan may be used to make sure the tube is in the right place. You may also need an x-ray after your chest tube is removed.
What you need to know about chest tube removal:
- Your healthcare provider will tell you when the chest tube can be removed. After heart surgery, your chest tube may be removed within 72 hours. For lungs, the chest tube can be taken out when your lung is working normally again. One sign of this is little or no fluid draining into the chest tube. Another sign is no air leaking for 1 to 2 days. You may need a chest x-ray to make sure your lung is working as it should.
- You may be given medicine to treat pain before the tube is removed. The tape will be removed. The stitches holding the tube in place will be loosened. You may need to breathe a certain way as the tube is taken out. Your provider will remove the tube and may tighten the stitches to close the opening. The area will be covered with a bandage that will stop air from getting into your chest.
Risks of a chest tube:
You may get an infection, or the place where the tube goes in may bleed more than expected. Your organs, blood vessels, or nerves may get damaged. You may have chest pain after the procedure. You may need to have the procedure again if the tube gets pulled out. If your condition comes back after treatment, you may need another chest tube. The chest tube may not decrease your signs and symptoms. The healthcare provider may not be able to insert the tube. If this happens, you may need to have another procedure or surgery.
Related medications
Call your local emergency number (911 in the US) if:
- You suddenly feel lightheaded and have shortness of breath.
- You have chest pain. You may have more pain when you take a deep breath or cough.
- You cough up blood.
Seek care immediately if:
- Blood or fluid soaks through your bandage.
- Your chest tube comes out.
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
Call your doctor if:
- You have a fever.
- You have severe pain and swelling at the insertion site.
- Your insertion site is red, draining pus, or has a bad smell coming from it.
- You have questions or concerns about your condition or care.
Self-care:
- Find a comfortable position. You may have pain or discomfort while the chest tube is in. Lie in a different position to help decrease your pain.
- Cough and breathe deeply as directed. This will decrease your risk for a lung infection. Take deep breaths and cough 10 times each hour. Hold a pillow tightly against your insertion site when you cough. Take a deep breath and hold it for as long as your can. Then let the air out and cough strongly.
Care for your chest tube:
- Check your chest tube for kinks or loops. Keep the tube close to you when you are in bed, but do not lie on it. Do not let loops of tubing hang down the side of your bed. Be sure your tubing is long enough so that you can move and turn in bed without pulling on it. Never clamp the tube yourself.
- Keep the suction device below the level of your chest. This will help fluids drain from your chest to the container below. This will also help prevent fluids from flowing back into your chest.
- Make sure your chest tube is secure. Make sure your chest tube is securely taped to your body. Your chest tube may also be taped to the suction device to help prevent the tubes from coming apart.
- Do not turn knobs or change settings on your device unless a healthcare provider tells you to. If your suction device has water in it, the water should bubble gently, with short periods of no bubbling. A lot of bubbling that does not stop may mean air is leaking.
Insertion site care:
Keep your bandage clean and dry. Ask your healthcare provider when you can bathe.
Follow up with your doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
