Dynacin Side Effects
Generic name: minocycline
Medically reviewed by Drugs.com. Last updated on Mar 18, 2025.
Note: This document provides detailed information about Dynacin Side Effects associated with minocycline. Some dosage forms listed on this page may not apply specifically to the brand name Dynacin.
Applies to minocycline: oral capsule, oral capsule extended release, oral tablet, oral tablet extended release.
Other dosage forms:
Precautions
It is very important that your doctor check the progress of you or your child at regular visits. This will allow your doctor to see if the medicine is working properly and to decide if you should continue to take it. Blood and urine tests may be needed to check for unwanted effects.
If your or your child's symptoms do not improve or if they become worse after 12 weeks of treatment, check with your doctor.
Using this medicine while you are pregnant can harm your unborn baby. The medicine may also cause birth defects if the father is using it when his sexual partner becomes pregnant. If a pregnancy occurs while you are using this medicine, tell your doctor right away.
Birth control pills may not work as well while you are using minocycline (the active ingredient contained in Dynacin). To keep from getting pregnant, use an additional form of birth control with your pills. Other forms include condoms, a diaphragm, or contraceptive foam or jelly.
This medicine may darken the color of your skin, nails, eyes, teeth, gums, or scars. Talk with your doctor if you or your child have any concerns.
Minocycline may cause diarrhea, and in some cases it can be severe. It may occur 2 months or more after you Stop taking minocycline. Do not take any medicine to treat diarrhea without first checking with your doctor. Diarrhea medicines may make the diarrhea worse or make it last longer. If you or your child have any questions about this or if mild diarrhea continues or gets worse, check with your doctor.
Check with your doctor right away if you or your child have pain or tenderness in the upper stomach, pale stools, dark urine, loss of appetite, nausea, vomiting, or yellow eyes or skin. These could be symptoms of a serious liver problem.
This medicine may cause some people to become dizzy or lightheaded. Make sure you know how you react to this combination of medicines before you drive, use machines, or do anything else that could be dangerous until you know how this medicine affects you.
This medicine may cause an increased pressure in your head which can lead to permanent vision loss. Check with your doctor right away if you or your child has severe headache, blurred vision, or any vision changes.
Contact your doctor immediately if fever, rash, joint pain, or tiredness occurs. These could be symptoms of an autoimmune syndrome where the body attacks itself.
Minocycline may cause your skin to be more sensitive to sunlight than it is normally. Exposure to sunlight, even for brief periods of time, may cause a skin rash, itching, redness or other discoloration of the skin, or a severe sunburn. When you begin taking this medicine:
- Stay out of direct sunlight, especially between the hours of 10:00 a.m. and 3:00 p.m., if possible.
- Wear protective clothing, including a hat. Also, wear sunglasses.
- Apply a sunblock product that has a sun protection factor (SPF) number of at least 15. Some patients may require a product with a higher SPF number, especially if they have a fair complexion. If you have any questions about this, check with your doctor.
- Apply a sunblock lipstick that has an SPF of at least 15 to protect your lips.
- Do not use a sun lamp or tanning bed or booth.
If you have a severe reaction from the sun, check with your doctor.
This medicine may cause serious allergic reactions, including anaphylaxis. Anaphylaxis requires immediate medical attention. The most serious signs of this reaction are very fast or irregular breathing, gasping for breath, or fainting. Other signs may include changes in color of the skin of the face, very fast but irregular heartbeat or pulse, hive-like swellings on the skin, and puffiness or swellings of the eyelids or around the eyes. If these side effects occur, get emergency help at once.
Before you have any medical tests, tell the medical doctor in charge that you or your child are taking this medicine. The results of some tests may be affected by this medicine.
If you plan to have children, talk with your doctor before using this medicine. This medicine may affect the process of sperm cell formation in males.
Do not take other medicines unless they have been discussed with your doctor. This includes prescription or nonprescription (over-the-counter [OTC]) medicines and herbal or vitamin supplements.
Common side effects of Dynacin
Some side effects of minocycline may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects.
Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
Less common side effects
- continuing ringing or buzzing or other unexplained noise in the ears
- difficulty with moving
- hearing loss
- hives or welts
- muscle stiffness
- redness of the skin
- sleepiness or unusual drowsiness
Incidence not known
- bloating
- discoloration of the tooth
- increased sensitivity of the skin to sunlight
- indigestion
- severe sunburn
Serious side effects of Dynacin
Along with its needed effects, minocycline may cause some unwanted effects. Although not all of these side effects may occur, if they do occur they may need medical attention.
Check with your doctor immediately if any of the following side effects occur while taking minocycline:
Incidence not known
- black, tarry stools
- blistering, peeling, or loosening of the skin
- blood in the urine or stools
- blurred or double vision
- bulging soft spot on the head of an infant
- chest pain, possibly moving to the left arm, neck, or shoulder
- confusion
- diarrhea
- dizziness or lightheadedness
- eye pain
- fast heartbeat
- general feeling of discomfort or illness
- general tiredness and weakness
- hives, itching, or skin rash
- joint or muscle pain
- large, hive-like swelling on the face, eyelids, lips, tongue, throat, hands, legs, feet, or sex organs
- loss of appetite
- nausea or vomiting
- red skin lesions, often with a purple center
- severe headache
- severe stomach pain
- sores, ulcers, or white spots on the lips or in the mouth
- troubled breathing
- unusual bleeding or bruising
- upper right abdominal or stomach pain
- yellow eyes and skin
See also:
For healthcare professionals
Applies to minocycline: intravenous powder for injection, oral capsule, oral capsule extended release, oral suspension, oral tablet, oral tablet extended release, oral and topical kit.
Nervous system adverse events
- Very common (10% or more): Headache (up to 23%)
- Common (1% to 10%): Dizziness (lightheadedness), somnolence, tinnitus, vertigo
- Rare (0.01% to 0.1%): Hypoesthesia, paresthesia, intracranial hypertension, impaired/decreased hearing
- Very rare (less than 0.01%): Bulging fontanels (in infants)
- Frequency not reported: Convulsions, sedation, ataxia, benign intracranial hypertension (pseudotumor cerebri), vestibular reactions[Ref]
Headache, dizziness, vertigo. and ataxia have been reported. These side effects were reversible within 3 to 48 hours of stopping therapy and occurred less often with low doses.
Pseudotumor cerebri, bulging fontanels (infants), and decreased hearing have also been reported during postmarketing experience.[Ref]
Dermatologic
- Common (1% to 10%): Pruritus, urticaria
- Rare (0.01% to 0.1%): Alopecia, erythema multiforme, erythema nodosum, fixed drug eruptions, hyperpigmentation (brownish or bluish-black pigmentation) of skin, photosensitivity, rash, vasculitis
- Very rare (less than 0.01%): Angioedema, exfoliative dermatitis, hyperpigmentation of nails/nail beds, Stevens-Johnson syndrome, toxic epidermal necrolysis
- Frequency not reported: Hyperpigmentation of various body sites (including bones, mucous membranes, teeth, oral mucosa, tongue, thyroid, eyes [including sclera, conjunctiva], breast milk, lacrimal secretions, structures of inner organs), maculopapular rash, erythematous rash, discolored perspiration, Sweet's syndrome (acute febrile neutrophilic dermatosis)
- Postmarketing reports: Anaphylactoid purpura, pigmentation of skin and mucous membranes, angioneurotic edema, drug rash with eosinophilia and systemic symptoms (DRESS)[Ref]
Hyperpigmentation of various body sites (including the skin, nails, teeth, oral mucosa, bones, thyroid, eyes [including sclera, conjunctiva], breast milk, lacrimal secretions, perspiration) has been reported. This blue/black/grey or muddy-brown discoloration was localized or diffuse. The most common site was the skin. Pigmentation often reversed when the drug was discontinued; however, resolution took several months or persisted in some cases. The generalized muddy-brown skin pigmentation sometimes persisted, especially in areas exposed to sun.
Biopsies of pigmented tissue have shown granules within the cells which stained positive for iron. This pigmentation faded over time after drug discontinuation.
DRESS syndrome (including fatal cases) has been reported. DRESS syndrome with persistent myocarditis has been reported in at least 3 cases.
Fixed drug eruptions, erythema multiforme, Stevens-Johnson syndrome, and photosensitivity have also been reported during postmarketing experience.[Ref]
Gastrointestinal
- Common (1% to 10%): Dry mouth
- Rare (0.01% to 0.1%): Diarrhea, nausea, stomatitis, discoloration of teeth, vomiting
- Very rare (less than 0.01%): Oral and anogenital candidiasis, dyspepsia, dysphagia, enamel hypoplasia, enterocolitis, esophagitis, esophageal ulcerations, glossitis, pancreatitis, pseudomembranous colitis
- Frequency not reported: Antibiotic-associated colitis, oral cavity discoloration (including buccal mucosa, tongue, lip, gum), abdominal cramping, inflammatory lesions (with monilial overgrowth) in the oral and anogenital regions[Ref]
Pancreatitis has rarely been associated with use of this drug. In 2 case reports, cystic fibrosis patients experienced pancreatitis during treatment with this drug for acute bacterial exacerbations of respiratory disease. The authors suggested that cystic fibrosis patients, as a result of the disease process, may be more susceptible to drug-induced pancreatitis. Additionally, in at least 1 case, multiple concomitant medications were taken; therefore, a temporal relationship between this drug and pancreatitis could not be proven conclusively.
Esophagitis and esophageal ulcerations have been reported in patients taking the capsule or tablet formulations of tetracycline-class antibiotics. Most of these patients took the drug immediately before going to bed.
Enterocolitis, pancreatitis, glossitis, dysphagia, and tooth discoloration have also been reported during postmarketing experience.[Ref]
Musculoskeletal
- Common (1% to 10%): Arthralgia, myalgia
- Rare (0.01% to 0.1%): Lupus-like syndrome (consisting of positive antinuclear antibody [ANA], arthralgia, arthritis, joint stiffness/swelling, and at least 1 of the following: fever, myalgia, hepatitis, rash, vasculitis)
- Very rare (less than 0.01%): Arthritis, bone discoloration, systemic lupus erythematosus (SLE), exacerbation of SLE, joint stiffness, joint swelling, joint discoloration, myopathy, hypersensitivity-associated rhabdomyolysis
- Postmarketing reports: Polyarthralgia, exacerbation of systemic lupus, transient lupus-like syndrome[Ref]
Lupus-like reactions induced by this drug have commonly presented with arthralgia or arthritis, myalgia or malaise, and positive ANA titer. Patients with highly positive anti-double stranded DNA (anti-dsDNA) antibodies have rarely been reported. All patients recovered after the drug was discontinued; however, several required short courses of corticosteroids.
Severe acute myopathy associated with this drug (100 mg orally per day) occurred in a 17-year-old male after strenuous exercise. His laboratory values were as follows: ESR 33 mm/hr, CRP 0.84 mg/dL, creatine kinase 87,297 units/L, AST 1307 units/L, ALT 311 units/L, LDH 4935 units/L, aldolase 12.6 units/L, alkaline phosphatase 145 units/L, GGT 66 units/L. Muscle enzyme levels normalized and his symptoms resolved 1 month after this drug was discontinued.
IV minocycline plus quinupristin-dalfopristin were associated with myalgia and arthralgia in 36% of neutropenic cancer patients (n=56).[Ref]
Other
- Common (1% to 10%): Fatigue, malaise
- Uncommon (0.1% to 1%): Fever
- Very rare (less than 0.01%): Discoloration of secretions
Injection:
- Frequency not reported: Magnesium intoxication (including flushing, sweating, hypotension, depressed reflexes, flaccid paralysis, hypothermia, circulatory collapse, cardiac and CNS depression, respiratory paralysis)[Ref]
Psychiatric
- Common (1% to 10%): Mood alteration
Hypersensitivity
- Rare (0.01% to 0.1%): Anaphylaxis/anaphylactoid reaction (including shock, fatalities)
- Frequency not reported: Hypersensitivity, hypersensitivity syndrome (consisting of cutaneous reaction [e.g., rash, exfoliative dermatitis], eosinophilia, and at least 1 of the following: hepatitis, pneumonitis, nephritis, myocarditis, pericarditis; with or without fever, lymphadenopathy), serum sickness-like syndrome (consisting of fever, urticaria/rash, arthralgia, arthritis, joint stiffness/swelling, lymphadenopathy; with or without eosinophilia), autoimmune vasculitis, drug fever, eosinophilic pneumonitis, drug hypersensitivity (e.g., pulmonary infiltrates, night sweats, fever, eosinophilia), serum sickness, serum sickness-like reactions, severe central nervous system (CNS)-pulmonary hypersensitivity syndrome
- Postmarketing reports: Hypersensitivity reactions, anaphylaxis[Ref]
Death has been reported in some cases involving hypersensitivity syndrome, serum sickness-like syndrome, and lupus-like syndrome.
Pulmonary infiltrates, night sweats, fever, and eosinophilia have developed in several patients receiving this drug. These effects were thought to be due to drug hypersensitivity.
Case reports have described a severe CNS -pulmonary hypersensitivity syndrome requiring high-dose corticosteroid therapy. Signs and symptoms have included dry cough, fever, ataxia, muscle weakness, numbness, visual abnormalities, abnormal brain MRI, seizures, pulmonary infiltrates, elevated serum IgE, elevated erythrocyte sedimentation rate (ESR), and eosinophilia.
Eosinophilic pneumonia with relapsing acute respiratory failure requiring mechanical ventilation and corticosteroids has been reported in a 54-year-old woman. Initial symptoms included dry cough, low-grade fever, fatigue, and dyspnea. Eosinophilia, elevated leukocytes, and C-reactive protein (CRP) were noted. At 14 days after being discharged and resuming this drug, the patient developed rapidly progressive respiratory failure again requiring mechanical ventilation.
Late-onset drug fever (associated with fever, sore throat, abdominal pain, weakness, loose bloody stools, fatigue, 40-pound weight loss, ESR 99 mm/hr, CRP 5 mg/dL, and mild increases in liver enzymes) has been reported in a 15-year-old boy after using this drug for 24 months for acne. After 1 year of therapy, at least 1 other case of late-onset drug fever occurred. Other reported cases of drug fever generally occurred after 2 to 4 weeks of drug exposure.[Ref]
Immunologic
- Frequency not reported: Positive antineutrophil cytoplasmic antibody (ANCA) titers, polyarteritis nodosa, ANCA-positive crescentic glomerulonephritis, ANCA-positive vasculitis, autoimmune hepatitis, necrotizing vasculitis and systemic reactions[Ref]
Rare cases of necrotizing vasculitis and systemic reactions have been reported, characterized by lymphadenopathy, eosinophilia, increased liver function enzyme levels, and dermatologic involvement. In each case, this drug was discontinued and in some cases, corticosteroid therapy was necessary to assist in the resolution of symptoms.[Ref]
Hepatic
- Rare (0.01% to 0.1%): Increased liver enzymes, hepatitis, autoimmune hepatitis/hepatotoxicity
- Very rare (less than 0.01%): Hepatic cholestasis, hepatic failure (including fatalities), hyperbilirubinemia, jaundice
- Frequency not reported: Autoimmune hepatitis with lupus-like symptoms, increased liver function test values, acute hepatic failure, liver injury, acute hypersensitivity hepatitis associated with eosinophilia and dermatitis[Ref]
Some hepatic reactions had an autoimmune basis and occurred after several months of therapy.
In 1 case, a patient developed rapidly progressing liver failure after using this drug for 4 weeks for acne. The patient had stopped this drug 2 weeks prior to onset of malaise. Liver transplantation was considered, but the patient slowly recovered without significant intervention.
Other reports of immunologically-mediated progressive liver dysfunction have rarely occurred. In 1 case, a patient received a liver transplant after fulminant hepatic failure which was thought to be related to a 3-year history of daily therapy to treat acne. The dose of this drug ranged from 50 to 200 mg/day. A second patient had been using this drug to treat acne for 1 year just prior to seeking medical attention for an "influenza-like" syndrome. Upon hospitalization, it was determined that the patient was experiencing an autoimmune-mediated hepatitis, most probably related to this drug. Resolution of symptoms occurred in both of these cases after therapy was discontinued and each patient had received appropriate supportive medical care.
Hepatitis and liver failure have also been reported during postmarketing experience.[Ref]
Renal
- Rare (0.01% to 0.1%): Increased BUN/serum urea, interstitial nephritis, acute renal failure
- Postmarketing reports: Reversible acute renal failure
Tetracyclines:
- Frequency not reported: Aggravation of preexisting renal failure, azotemia/uremia, nephrotoxicity (associated with acute fatty liver), renal tubular damage, Fanconi-like syndrome[Ref]
Nephrotoxicity associated with acute fatty liver has been reported with high tetracycline doses. High serum levels of tetracyclines have been associated with azotemia, hyperphosphatemia, and acidosis in patients with renal dysfunction.
Degraded tetracycline may cause renal tubular damage and a Fanconi-like syndrome.[Ref]
Hematologic
- Rare (0.01% to 0.1%): Eosinophilia, leukopenia, neutropenia, thrombocytopenia
- Very rare (less than 0.01%): Hemolytic anemia, pancytopenia
- Frequency not reported: Agranulocytosis, antineutrophil cytoplasmic antibody (ANCA)-positive vasculitis[Ref]
Hemolytic anemia, thrombocytopenia, and eosinophilia have also been reported during postmarketing experience.[Ref]
Respiratory
- Rare (0.01% to 0.1%): Cough, dyspnea, pulmonary infiltration
- Very rare (less than 0.01%): Bronchospasm, exacerbation of asthma, pulmonary eosinophilia
- Frequency not reported: Pneumonitis, hypersensitivity pneumonitis, pulmonary lupus, eosinophilic pneumonia, pleural effusions, relapsing acute respiratory failure
- Postmarketing reports: Pulmonary infiltrates with eosinophilia[Ref]
Cardiovascular
- Rare (0.01% to 0.1%): Myocarditis, pericarditis[Ref]
Metabolic
- Rare (0.01% to 0.1%): Anorexia
Tetracyclines:
- Frequency not reported: Hyperphosphatemia, acidosis[Ref]
High serum levels of tetracyclines have been associated with azotemia, hyperphosphatemia, and acidosis in patients with renal dysfunction.[Ref]
Endocrine
- Very rare (less than 0.01%): Abnormal thyroid function, brown-black microscopic thyroid discoloration
- Frequency not reported: Discolored breast secretions[Ref]
A condition characterized by dark pigmentation (brown-black microscopic discoloration) of the thyroid gland has been reported; however, there was no clinical or laboratory evidence of thyroid dysfunction (unknown clinical implications).
Brown-black microscopic thyroid discoloration and abnormal thyroid function have also been reported during postmarketing experience.[Ref]
Genitourinary
- Very rare (less than 0.01%): Balanitis (due to lesions on the glans penis), vulvovaginitis
- Postmarketing reports: Deleterious effects on spermatogenesis[Ref]
Balanitis has also been reported during postmarketing experience.[Ref]
Local
- Frequency not reported: Injection site erythema, injection site pain[Ref]
Oncologic
- Frequency not reported: Papillary thyroid cancer
- Postmarketing reports: Thyroid cancer
Ocular
- Frequency not reported: Discoloration of conjunctiva, discoloration of lacrimal secretions, grey scleral pigmentation, macular pigmentation[Ref]
Cases of grey scleral pigmentation and macular pigmentation have been reported in elderly patients after chronic use of this drug (5 to 12 years).[Ref]
References
1. Joy VA (1979) "Minocycline and ototoxicity." N Engl J Med, 301, p. 1450
2. Friedlander IR (1979) "Minocycline and ototoxicity." N Engl J Med, 1301, p. 1450-1
3. Delaney RA, Narayanaswamy TR (1990) "Pseudo-tumor cerebri and acne." Mil Med, 155, p. 511
4. Donnet A, Dufour H, Graziani N, Grisoli F (1992) "Minocycline and benign intracranial hypertension." Biomed Pharmacother, 46, p. 171-2
5. (2002) "Product Information. Minocin (minocycline)." Lederle Laboratories
6. Lewis PA, Kearney PJ (1997) "Pseudotumor cerebri induced by minocycline treatment for acne vulgaris." Acta Derm Venereol, 77, p. 83
7. Chiu AM, Chuenkongkaew WL, Cornblath WT, Trobe JD, Digre KB, Dotan SA, Musson KH, Eggenberger ER (1998) "Minocycline treatment and pseudotumor cerebri syndrome." Am J Ophthalmol, 126, p. 116-21
8. Matteson EL, Johnson BW, Maher JD (1998) "Arthralgias, myalgias, and autoimmune hepatitis with minocycline therapy." J Rheumatol, 25, p. 1653-4
9. Weese-Mayer DE, Yang RJ, Mayer JR, Zaparackas Z (2001) "Minocycline and Pseudotumor cerebri: The well-known but well-kept secret." Pediatrics, 108, p. 519-20
10. Settgast AM, Groth T, Gertner E (2003) "Minocycline-induced central nervous system-pulmonary hypersensitivity syndrome." Int J Dermatol, 42, p. 316-7
11. Cerner Multum, Inc. "UK Summary of Product Characteristics."
12. Cerner Multum, Inc. "Australian Product Information."
13. Caro I (1980) "Discoloration of the teeth related to minocycline therapy for acne." J Am Acad Dermatol, 3, p. 317-8
14. McGrae JD, Zelickson AS (1980) "Skin pigmentation secondary to minocycline therapy." Arch Dermatol, 116, p. 1262-5
15. Wolfe ID, Reichmister J (1984) "Minocycline hyperpigmentation: skin, tooth, nail, and bone involvement." Cutis, 33, p. 457-8
16. Gordon G, Sparano BM, Iatropoulos MJ (1985) "Hyperpigmentation of the skin associated with minocycline therapy." Arch Dermatol, 121, p. 618-23
17. Bridges AJ, Graziano FM, Calhoun W, Reizner GT (1990) "Hyperpigmentation, neutrophilic alveolitis, and erythema nodosum resulting from minocycline." J Am Acad Dermatol, 22, p. 959-62
18. Mensing H, Kowalzick L (1991) "Acute febrile neutrophilic dermatosis (Sweet's syndrome) caused by minocycline." Dermatologica, 182, p. 43-6
19. Meyerson MA, Cohen PR, Hymes SR (1995) "Lingual hyperpigmentation associated with minocycline therapy." Oral Surg Oral Med Oral Pathol, 79, p. 180-4
20. Odell EW, Hodgson RP, Haskell R (1995) "Oral presentation of minocycline-induced black bone disease." Oral Surg Oral Med Oral Pathol, 79, p. 459-61
21. Katz J, Barak S, Shemer J, Langevitz P, Livneh A (1995) "Black tongue associated with minocycline therapy." Arch Dermatol, 131, p. 620
22. Hung PH, Caldwell JB, James WD (1995) "Minocycline-induced hyperpigmentation." J Fam Pract, 41, p. 183-5
23. Thibault MJ, Billick RC, Srolovitz H (1992) "Minocycline-induced Sweet's syndrome." J Am Acad Dermatol, 27, p. 801-4
24. Fleming CJ, Hunt MJ, Salisbury ELC, Mccarthy SW, Barnetson RS (1996) "Minocycline-induced hyperpigmentation in leprosy." Br J Dermatol, 134, p. 784-7
25. Tsao H, Busam K, Barnhill RL, Dover JS (1996) "Treatment of minocycline-induced hyperpigmentation with the q-switched ruby laser." Arch Dermatol, 132, p. 1250-1
26. Yamamoto T, Minatohara K (1997) "Minocycline-induced acute generalized exanthematous pustulosis in a patient with generalized pustular psoriasis showing elevated level of sELAM-1." Acta Derm Venereol, 77, p. 168-9
27. Elkayam O, Levartovsky D, Brautbar C, Yaron M, Burke M, Vardinon N, Caspi D (1998) "Clinical and immunological study of 7 patients with minocycline-induced autoimmune phenomena." Am J Med, 105, p. 484-7
28. Tanzi EL, Hecker MS (2000) "Minocycline-induced hyperpigmentation of the tongue." Arch Dermatol, 136, p. 427-8
29. Ho NC, McInerney A, Levy H, Francomano CA, Elkayam O (2000) "Minocycline-induced generalized postinflammatory elastolysis." Am J Med, 109, p. 340-1
30. Schaffer J, Davidson DM, McNiff JM, Bolognia JL (2001) "Perinuclear antineutrophilic cytoplasmic antibody-positive cutaneous polyarteritis nodosa associated with minocycline therapy for acne vulgaris." J Am Acad Dermatol, 44, p. 198-206
31. MarzoOrtega H, Misbah S, Emery P (2001) "Minocycline induced autoimmune disease in rheumatoid arthritis: A missed diagnosis?." Journal of Rheumatology, 28, p. 377-8
32. Khan Durani B, Jappe U (2002) "Drug-induced Sweet's syndrome in acne caused by different tetracyclines: case report and review of the literature." Br J Dermatol, 147, p. 558-62
33. Peyriere H, Dereure O, Breton H, et al. (2006) "Variability in the clinical pattern of cutaneous side-effects of drugs with systemic symptoms: does a DRESS syndrome really exist?" Br J Dermatol, 155, p. 422-8
34. Huq F, Durso SC (2008) "Spurious bruising in a patient taking warfarin: minocycline-induced skin hyperpigmentation." J Am Geriatr Soc, 56, p. 1156-7
35. Tavares J, Leung WW (2011) "Discoloration of nail beds and skin from minocycline." CMAJ, 183, p. 224
36. Wetter DA (2012) "Minocycline hyperpigmentation." Mayo Clin Proc, 87, e33
37. Kalai C, Brand R, Yu L (2012) "Minocycline-induced Sweet syndrome (acute febrile neutrophilic dermatosis)." J Am Acad Dermatol, 67, e289-91
38. Boyle MP (2001) "Minocycline-induced pancreatitis in cystic fibrosis." Chest, 119, p. 1283-5
39. Matsuura T, Shimizu Y, Fujimoto H, Miyazaki T, Kano S (1992) "Minocycline-related lupus." Lancet, 340, p. 1553
40. Knights SE, Leandro MJ, Khamashta MA, Hughes GRV (1998) "Minocycline-induced arthritis." Clin Exp Rheumatol, 16, p. 587-90
41. Raad I, Hachem R, Hanna H, et al. (2001) "Treatment of vancomycin-resistant enterococcal infections in the immunocompromised host: quinupristin-dalfopristin in combination with minocycline." Antimicrob Agents Chemother, 45, p. 3202-4
42. (2002) "Minocycline hypersensitivity syndrome manifesting with rhabdomyolysis." Int J Dermatol, 41, p. 530-531
43. Narvaez J, Vilaseca-Momplet J (2004) "Severe acute myopathy induced by minocycline." Am J Med, 116, p. 282-3
44. Chatham WW, Ross DW (1983) "Leukemoid blood reaction to tetracycline." South Med J, 76, p. 1195-6
45. Otero M, Goodpasture HC (1983) "Pulmonary infiltrates and eosinophilia from minocycline." JAMA, 250, p. 2602
46. LePaw MI (1983) "Fixed drug eruption due to minocycline-report of one case." J Am Acad Dermatol, 8, p. 263-4
47. Rosin MA (1984) "Viral-like syndrome associated with minocycline." Arch Dermatol, 120, p. 575
48. Shoji A, Someda Y, Hamada T (1987) "Stevens-Johnson syndrome due to minocycline therapy." Arch Dermatol, 123, p. 18-20
49. Puyana J, Urena V, Quirce S, Fernandez-Rivas M, Cuevas M, Fraj J (1990) "Serum sickness-like syndrome associated with minocycline therapy." Allergy, 45, p. 313-5
50. Gorard DA (1990) "Late-onset drug fever associated with minocycline." Postgrad Med J, 66, p. 404-5
51. Guillon JN, Joly P, Autran B, et al. (1992) "Minocycline-induced cell-mediated hypersensitivity pneumonitis." Ann Intern Med, 117, p. 476-81
52. Sitbon O, Bidel N, Dussopt C, Azarian R, Braud ML, Lebargy F, Fourme T, Deblay F, Piard F, Camus P (1994) "Minocycline pneumonitis and eosinophilia - a report on eight patients." Arch Intern Med, 154, p. 1633-40
53. Kaufmann D, Pichler W, Beer JH (1994) "Severe episode of high fever with rash, lymphadenopathy, neutropenia, and eosinophilia after minocycline therapy for acne." Arch Intern Med, 154, p. 1983-4
54. Quilty B, Mchugh N (1994) "Lupus-like syndrome associated with the use of minocycline." Br J Rheumatol, 33, p. 1197-8
55. Gordon PM, White MI, Herriot R, Martin JC, Reid DM (1995) "Minocycline-associated lupus erythematosus." Br J Dermatol, 132, p. 120-1
56. Dykhuizen RS, Legge JS (1995) "Minocycline induced pulmonary eosinophilia." Respir Med, 89, p. 61-2
57. Parneixspake A, Bastujigarin S, Lobut JB, Erner J, Guyetrousset P, Revuz J, Roujeau JC (1995) "Minocycline as possible cause of severe and protracted hypersensitivity drug reaction." Arch Dermatol, 131, p. 490-1
58. Dykhuizen RS, Zaidi AM, Godden DJ, Jegarajah S, Legge JS (1995) "Lesson of the week: minocycline and pulmonary eosinophilia." BMJ, 310, p. 1520-1
59. Piperno D, Donne C, Loire R, Cordier JF (1995) "Bronchiolitis obliterans organizing pneumonia associated with minocycline therapy: a possible cause." Eur Respir J, 8, p. 1018-20
60. Ferner RE, Moss C (1996) "Minocycline for acne - first line antibacterial treatment of acne should be with tetracycline or oxytetracycline." BMJ, 312, p. 138
61. Macneil M, Haase DA, Tremaine R, Marrie TJ (1997) "Fever, lymphadenopathy, eosinophilia, lymphocytosis, hepatitis, and dermatitis: a severe adverse reaction to minocycline." J Am Acad Dermatol, 36, p. 347-50
62. Bentur L, Bar-Kana Y, Livni E, et al. (1997) "Severe minocycline-induced eosinophilic pneumonia: extrapulmonary manifesations and the use of in vitro immunoassays." Ann Pharmacother, 31, p. 733-5
63. Shapiro LE, Knowles SR, Shear NH (1997) "Comparative safety of tetracycline, minocycline, and doxycycline." Arch Dermatol, 133, p. 1224-30
64. Akin E, Miller LC, Tucker LB (1998) "Minocycline-induced lupus in adolescents." Pediatrics, 101, p. 926-8
65. Bhat G, Jordan J, Sokalski S, Bajaj V, Marshall R, Berkelhammer C (1998) "Minocycline-induced hepatitis with autoimmune features and neutropenia." J Clin Gastroenterol, 27, p. 74-5
66. Hara H, Fujitsuka A, Morishima C, Kurihara N, Yamaguchi ZI, Morishima T (1998) "Severe drug-induced pneumonitis associated with minocycline and nicotinamide therapy of a bullous pemphigoid." Acta Derm Venereol, 78, p. 393-4
67. Hess EV (1998) "Minocycline and autoimmunity." Clin Exp Rheumatol, 16, p. 519-21
68. Teitelbaum JE, PerezAtayde AR, Cohen M, Bousvaros A, Jonas MM (1998) "Minocycline-related autoimmune hepatitis: Case series and literature review." Arch Pediatr Adolesc Med, 152, p. 1132-6
69. Angulo JM, Sigal LH, Espinoza LR (1998) "Coexistent minocycline-induced systemic lupus erythematosus and autoimmune hepatitis." Semin Arthritis Rheum, 28, p. 187-92
70. Schrodt BJ, Callen JP (1999) "Polyarteritis nodosa attributable to minocycline treatment for acne vulgaris." Pediatrics, 103, p. 503-5
71. Sturkenboom MCJM, Meier CR, Jick H, Stricker BHC (1999) "Minocycline and lupuslike syndrome in acne patients." Arch Intern Med, 159, p. 493-7
72. Christodoulou CS, Emmanuel P, Ray RA, Good RA, Schnapf BM, Cawkwell GD (1999) "Respiratory distress due to minocycline-induced pulmonary lupus." Chest, 115, p. 1471-3
73. Angulo JM, Sigal LH, Espinoza LR (1999) "Minocycline induced lupus and autoimmune hepatitis." J Rheumatol, 26, p. 1420-1
74. Pohle T, Menzel J, Domschke W (2000) "Minocycline and fulminant hepatic failure necessitating liver transplantation." Am J Gastroenterol, 95, p. 560-1
75. Kettaneh A, Fain O, Ziol M, Lejeune F, EclacheSaudreau V, Biaggi A, GuettierBouttier C, Thomas M (2000) "Minocycline-induced systemic adverse reaction with liver and bone marrow granulomas and Sezary-like cells." Am J Med, 108, p. 353-4
76. Malakar S, Dhar S, Malakar RS (2001) "Is serum sickness an uncommon adverse effect of minocycline treatment?." Arch Dermatol, 137, p. 100-1
77. Grim SA, Romanelli F, Jennings PR, Ofotokun I (2003) "Late-onset drug fever associated with minocycline: case report and review of the literature." Pharmacotherapy, 23, p. 1659-62
78. Kounis GN, Kouni SA, Chiladakis JA, Kounis NG (2009) "Comment: Mesalamine-Associated Hypersensitivity Myocarditis in Ulcerative Colitis and the Kounis Syndrome (February)." Ann Pharmacother, 43, p. 393-4
79. Shaughnessy KK, Bouchard SM, Mohr MR, Herre JM, Salkey KS (2009) "Minocycline-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome with persistent myocarditis." J Am Acad Dermatol, 62, p. 315-8
80. (2009) "Drugs for rheumatoid arthritis." Treat Guidel Med Lett, 7, p. 37-46
81. Byrne PAC, Williams BD, Pritchard MH (1994) "Minocycline-related lupus." Br J Rheumatol, 33, p. 674-6
82. Gough A, Chapman S, Wagstaff K, Emery P, Elias E (1996) "Minocycline induced autoimmune hepatitis and systemic lupus erythematosus-like syndrome." BMJ, 312, p. 169-72
83. Harel L, Amir J, Livni E, Straussberg RS, Varsano I (1996) "Serum-sickness-like reaction associated with minocycline therapy in adolescents." Ann Pharmacother, 30, p. 481-3
84. Knowles SR, Shapiro L, Shear NH (1996) "Serious adverse reactions induced by minocycline: report of 13 patients and review of the literature." Arch Dermatol, 132, p. 934-9
85. Elkayam O, Yaron M, Caspi D (1996) "Minocycline induced arthritis associated with fever, livedo reticularis, and pANCA." Ann Rheum Dis, 55, p. 769-71
86. Masson C, Chevailler A, Pascaretti C, Legrand E, Bregeon C, Audran M (1996) "Minocycline related lupus." J Rheumatol, 23, p. 2160-1
87. Golstein PE, Deviere J, Cremer M (1997) "Acute hepatitis and drug-related lupus induced by minocycline treatment." Am J Gastroenterol, 92, p. 143-6
88. Crosson J, Stillman MT (1997) "Minocycline-related lupus erythematosus with associated liver disease." J Am Acad Dermatol, 36, p. 867-8
89. Farver DK (1997) "Minocycline-induced lupus." Ann Pharmacother, 31, p. 1160-3
90. Gordon MM, Porter D (2001) "Minocycline induced lupus: Case series in the West of Scotland." J Rheumatol, 28, p. 1004-6
91. Balestrero S, Ciambellotti A, Parodi A, Rebora A (2001) "Minocycline-induced lupus-like syndrome." Int J Dermatol, 40, p. 474-5
92. Sethi S, Sahani M, Oei LS (2003) "ANCA-positive crescentic glomerulonephritis associated with minocycline therapy." Am J Kidney Dis, 42, E27-31
93. Margolis DJ, Hoffstad O, Bilker W (2007) "Association or lack of association between tetracycline class antibiotics used for acne vulgaris and lupus erythematosus." Br J Dermatol, 15, p. 540-6
94. Gait RC, Affleck AG, Leach IH, Varma S (2008) "Perinuclear antineutrophilic cytoplasmic antibody-positive polyarteritis nodosa secondary to minocycline treatment for acne vulgaris." J Am Acad Dermatol, 58(5 Suppl 1), S123-4
95. Burette A, Finet C, Prigogine T, De Roy G, Deltenre M (1984) "Acute hepatic injury associated with minocycline." Arch Intern Med, 144, p. 1491-2
96. Min DI, Burke PA, Lewis D, Jenkins RL (1992) "Acute hepatic failure associated with oral minocycline: a case report." Pharmacotherapy, 12, p. 68-71
97. Malcolm A, Heap TR, Eckstein RP, Lunzer MR (1996) "Minocycline-induced liver injury." Am J Gastroenterol, 91, p. 1641-3
98. Nietsch HH, Libman BS, Pansze TW, Eicher JN, Reeves JRT, Krawitt EL (2000) "Minocycline-induced hepatitis." Am J Gastroenterol, 95, p. 2993-5
99. Seaman HE, Lawrenson RA, Williams TJ, MacRae KD, Farmer RDT (2001) "The risk of liver damage associated with minocycline: A comparative study." J Clin Pharmacol, 41, p. 852-60
100. Oddo M, Liaudet L, Lepori M, Broccard AF, Schaller MD (2003) "Relapsing acute respiratory failure induced by minocycline." Chest, 123, p. 2146-8
101. Ohaki Y, Misugi K, Hasegawa H (1986) ""Black thyroid" associated with minocycline therapy." Acta Pathol Jpn, 36, p. 1367-75
102. Landas SK, Schelper RL, Tio FO, Turner JW, Moore KC, Bennett-Gray J (1986) "Black thyroid syndrome: exaggeration of a normal process?" Am J Clin Pathol, 85, p. 411-8
103. Bradfield YS, Robertson DM, Salomao DR, Link TP, Rostvold JA (2003) "Photo essay: minocycline-induced ocular pigmentation." Arch Ophthalmol, 121, p. 144-5
Frequently asked questions
More about Dynacin (minocycline)
- Check interactions
- Compare alternatives
- Reviews (2)
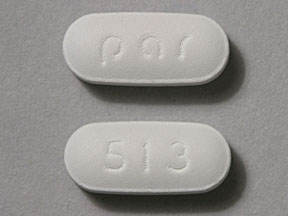
- Drug images
- Dosage information
- During pregnancy
- Drug class: tetracyclines
- Breastfeeding
Patient resources
Other brands
Minocin, Emrosi, Minolira, Solodyn, ... +2 more
Professional resources
Other brands
Minocin, Emrosi, Minocin for Injection, Minolira, ... +2 more
Related treatment guides
Further information
Dynacin side effects can vary depending on the individual. Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
Note: Medication side effects may be underreported. If you are experiencing side effects that are not listed, submit a report to the FDA by following this guide.