Basaglar: Package Insert / Prescribing Info
Package insert / product label
Generic name: insulin glargine
Dosage form: injection, solution
Drug class: Insulin
J Code (medical billing code): J1815 (Per 5 units, injection)
Medically reviewed by Drugs.com. Last updated on Dec 19, 2023.
On This Page
- Indications and Usage
- Dosage and Administration
- Dosage Forms and Strengths
- Contraindications
- Warnings and Precautions
- Adverse Reactions/Side Effects
- Drug Interactions
- Use In Specific Populations
- Overdosage
- Description
- Clinical Pharmacology
- Nonclinical Toxicology
- Clinical Studies
- How Supplied/Storage and Handling
- Storage and Handling
- Patient Counseling Information
Highlights of Prescribing Information
BASAGLAR (insulin glargine) injection, for subcutaneous use
Initial U.S. Approval: 2015
Indications and Usage for Basaglar
Basaglar Dosage and Administration
- Individualize dosage based on metabolic needs, blood glucose monitoring, glycemic control, type of diabetes, prior insulin use. (2.2, 2.3, 2.4)
- Administer subcutaneously once daily at any time of day, but at the same time every day. (2.2)
- Rotate injection sites into the abdominal area, thigh, or deltoid to reduce the risk of lipodystrophy and localized cutaneous amyloidosis. (2.1)
- Closely monitor glucose when converting to BASAGLAR and during initial weeks thereafter. (2.2)
- Do not dilute or mix with any other insulin or solution. (2.1)
Dosage Forms and Strengths
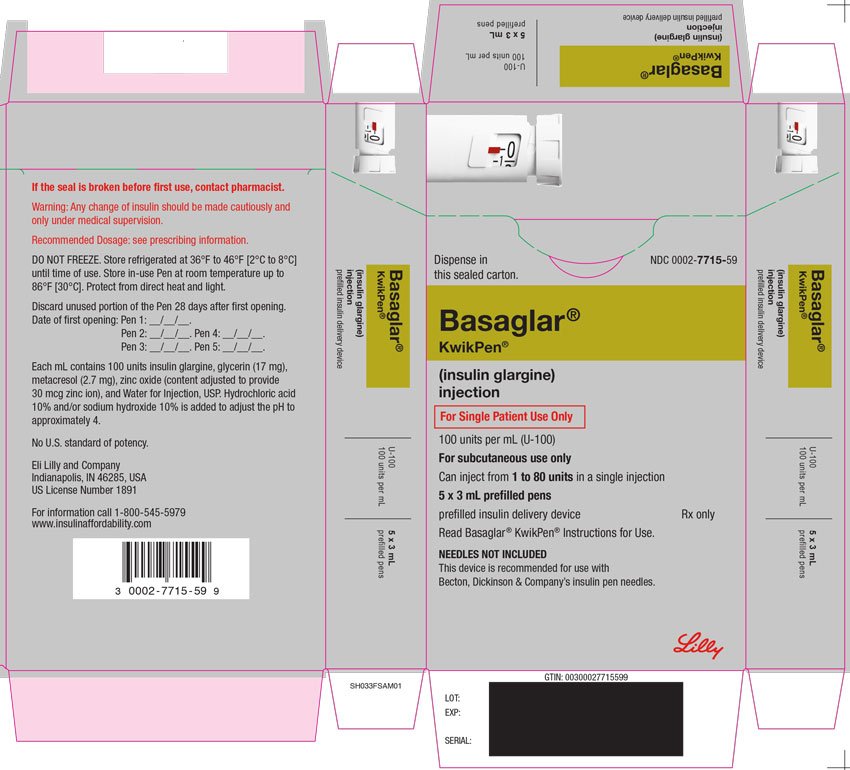
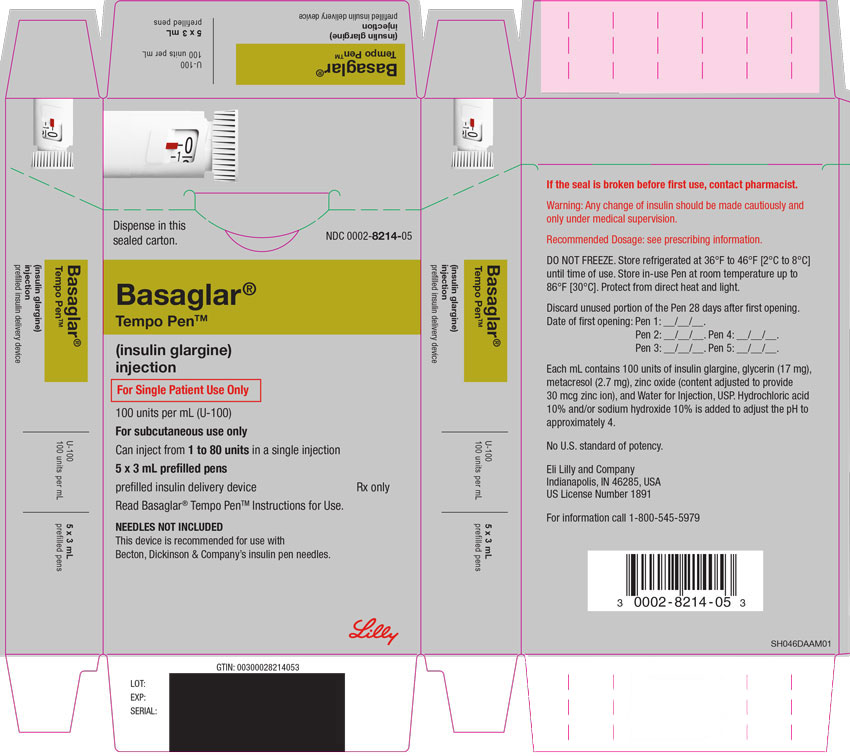
Injection: 100 units/mL (U-100) is available as: (3)
- 3 mL single-patient-use BASAGLAR KwikPen®
- 3 mL single-patient-use BASAGLAR Tempo PenTM
Contraindications
Warnings and Precautions
- Never share a BASAGLAR prefilled pen between patients, even if the needle is changed. (5.1)
- Hyperglycemia or hypoglycemia with changes in insulin regimen: Make changes to a patient's insulin regimen (e.g., insulin strength, manufacturer, type, injection site or method of administration) under close medical supervision with increased frequency of blood glucose monitoring. (5.2)
- Hypoglycemia: May be life-threatening. Increase frequency of glucose monitoring with changes to: insulin dosage, co-administered glucose lowering medications, meal pattern, physical activity; and in patients with renal or hepatic impairment and hypoglycemia unawareness. (5.3, 6.1)
- Hypoglycemia due to medication errors: Accidental mix-ups between insulin products can occur. Instruct patients to check insulin labels before injection. (5.4)
- Hypersensitivity reactions: Severe, life-threatening, generalized allergy, including anaphylaxis, can occur. Discontinue BASAGLAR, monitor and treat if indicated. (5.5, 6.1)
- Hypokalemia: May be life-threatening. Monitor potassium levels in patients at risk of hypokalemia and treat if indicated. (5.6)
- Fluid retention and heart failure with concomitant use of thiazolidinediones (TZDs): Observe for signs and symptoms of heart failure; consider dosage reduction or discontinuation if heart failure occurs. (5.7)
Adverse Reactions/Side Effects
Adverse reactions commonly (≥5%) associated with insulin glargine products are: Hypoglycemia, allergic reactions, injection site reaction, lipodystrophy, pruritus, rash, edema, and weight gain. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact Eli Lilly and Company at 1-800-LillyRx (1-800-545-5979) or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
Drug Interactions
- Drugs that may increase the risk of hypoglycemia: antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates, somatostatin analog (e.g., octreotide), and sulfonamide antibiotics (7).
- Drugs that may decrease the blood glucose lowering effect: atypical antipsychotics, corticosteroids, danazol, diuretics, estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g., in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g., albuterol, epinephrine, terbutaline), and thyroid hormones (7).
- Drugs that may increase or decrease the blood glucose lowering effect: alcohol, beta-blockers, clonidine, lithium salts, and pentamidine (7).
- Drugs that may blunt the signs and symptoms of hypoglycemia: beta-blockers, clonidine, guanethidine, and reserpine (7).
See 17 for PATIENT COUNSELING INFORMATION and FDA-approved patient labeling.
Revised: 7/2021
Full Prescribing Information
1. Indications and Usage for Basaglar
BASAGLAR® is indicated to improve glycemic control in adults and pediatric patients with type 1 diabetes mellitus and in adults with type 2 diabetes mellitus.
2. Basaglar Dosage and Administration
2.1 Important Administration Instructions
- Always check insulin labels before administration [see Warnings and Precautions (5.4)].
- Visually inspect BASAGLAR prefilled pens for particulate matter and discoloration prior to administration. Only use if the solution is clear and colorless with no visible particles.
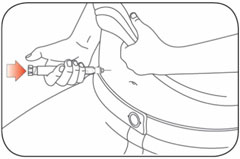
- Administer BASAGLAR subcutaneously into the abdominal area, thigh, or deltoid, and rotate injection sites within the same region from one injection to the next to reduce the risk of lipodystrophy and localized cutaneous amyloidosis. Do not inject into areas of lipodystrophy or localized cutaneous amyloidosis [see Warnings and Precautions (5.2) and Adverse Reactions (6)].
- During changes to a patient's insulin regimen, increase the frequency of blood glucose monitoring [see Warnings and Precautions (5.2)].
- Use BASAGLAR with caution in patients with visual impairment that may rely on audible clicks to dial their dose.
- Do not dilute or mix BASAGLAR with any other insulin or solution.
- Do not administer intravenously or via an insulin pump.
2.2 General Dosing Instructions
- In patients with type 1 diabetes, BASAGLAR must be used concomitantly with short-acting insulin.
- Inject BASAGLAR subcutaneously once daily at any time of day but at the same time every day.
- Individualize and adjust the dosage of BASAGLAR based on the individual's metabolic needs, blood glucose monitoring results and glycemic control goal.
- Dosage adjustments may be needed with changes in physical activity, changes in meal patterns (i.e., macronutrient content or timing of food intake), during acute illness, or changes in renal or hepatic function. Dosage adjustments should only be made under medical supervision with appropriate glucose monitoring [see Warnings and Precautions (5.2)].
- The BASAGLAR prefilled pens each dials in 1 unit increments and delivers a maximum dose of 80 units per injection.
2.3 Initiation of BASAGLAR Therapy
- The recommended starting dose of BASAGLAR in patients with type 1 diabetes should be approximately one-third of the total daily insulin requirements. Short- or rapid-acting, pre-meal insulin should be used to satisfy the remainder of the daily insulin requirements.
- The recommended starting dose of BASAGLAR in patients with type 2 diabetes is 0.2 units/kg or up to 10 units once daily.
2.4 Changing to BASAGLAR from Other Insulin Therapies
- If changing patients from another insulin glargine product, 100 units/mL, to BASAGLAR, the dose of BASAGLAR should be the same as the other insulin glargine product, 100 units/mL.
- If changing patients from a once-daily insulin glargine product, 300 units/mL, to once-daily BASAGLAR, the recommended initial BASAGLAR dosage is 80% of the insulin glargine product, 300 units/mL [see Warnings and Precautions (5.2)].
- If changing from a treatment regimen with an intermediate- or long-acting insulin to a regimen with BASAGLAR, a change in the dose of the basal insulin may be required.
- If changing patients from twice-daily NPH insulin to once-daily BASAGLAR, the recommended initial BASAGLAR dosage is 80% of the total daily NPH dosage [see Warnings and Precautions (5.2)].
3. Dosage Forms and Strengths
Injection: 100 units/mL (U-100) clear and colorless solution available as:
- 3 mL single-patient-use BASAGLAR KwikPen
- 3 mL single-patient-use BASAGLAR Tempo Pen
5. Warnings and Precautions
5.1 Never Share a BASAGLAR Prefilled Pen Between Patients
BASAGLAR prefilled pens must never be shared between patients, even if the needle is changed. Sharing poses a risk for transmission of blood-borne pathogens.
5.2 Hyperglycemia or Hypoglycemia with Changes in Insulin Regimen
Changes in an insulin regimen (e.g., insulin strength, manufacturer, type, injection site or method of administration) may affect glycemic control and predispose to hypoglycemia [see Warnings and Precautions (5.3)] or hyperglycemia. Repeated insulin injections into areas of lipodystrophy or localized cutaneous amyloidosis have been reported to result in hyperglycemia; and a sudden change in the injection site (to an unaffected area) has been reported to result in hypoglycemia [see Adverse Reactions (6)].
Make any changes to a patient's insulin regimen under close medical supervision with increased frequency of blood glucose monitoring. Advise patients who have repeatedly injected into areas of lipodystrophy or localized cutaneous amyloidosis to change the injection site to unaffected areas and closely monitor for hypoglycemia. For patients with type 2 diabetes, dosage adjustments of concomitant anti-diabetic products may be needed.
5.3 Hypoglycemia
Hypoglycemia is the most common adverse reaction associated with insulins, including BASAGLAR [see Adverse Reactions (6.1)]. Severe hypoglycemia can cause seizures, may be life-threatening or cause death. Hypoglycemia can impair concentration ability and reaction time; this may place an individual and others at risk in situations where these abilities are important (e.g., driving or operating other machinery). BASAGLAR, or any insulin, should not be used during episodes of hypoglycemia [see Contraindications (4)].
Hypoglycemia can happen suddenly and symptoms may differ in each individual and change over time in the same individual. Symptomatic awareness of hypoglycemia may be less pronounced in patients with longstanding diabetes, in patients with diabetic nerve disease, in patients using medications that block the sympathetic nervous system (e.g., beta-blockers) [see Drug Interactions (7)], or in patients who experience recurrent hypoglycemia.
Risk Factors for Hypoglycemia
The risk of hypoglycemia after an injection is related to the duration of action of the insulin and, in general, is highest when the glucose lowering effect of the insulin is maximal. As with all insulins, the glucose lowering effect time course of BASAGLAR may vary in different individuals or at different times in the same individual and depends on many conditions, including the area of injection as well as the injection site blood supply and temperature [see Clinical Pharmacology (12.2)]. The risk of hypoglycemia generally increases with intensity of glycemic control. Other factors which may increase the risk of hypoglycemia include changes in meal pattern (e.g., macronutrient content or timing of meals), changes in level of physical activity, or changes to co-administered medication [see Drug Interactions (7)]. Patients with renal or hepatic impairment may be at higher risk of hypoglycemia [see Use in Specific Populations (8.6, 8.7)].
Risk Mitigation Strategies for Hypoglycemia
Patients and caregivers must be educated to recognize and manage hypoglycemia. Self-monitoring of blood glucose plays an essential role in the prevention and management of hypoglycemia. In patients at higher risk for hypoglycemia and patients who have reduced symptomatic awareness of hypoglycemia, increased frequency of blood glucose monitoring is recommended.
The long-acting effect of BASAGLAR may delay recovery from hypoglycemia.
5.4 Hypoglycemia Due to Medication Errors
Accidental mix-ups between insulin products have been reported. To avoid medication errors between BASAGLAR and other insulins, instruct patients to always check the insulin label before each injection.
5.5 Hypersensitivity Reactions
Severe, life-threatening, generalized allergy, including anaphylaxis, can occur with insulins, including BASAGLAR. If hypersensitivity reactions occur, discontinue BASAGLAR; treat per standard of care and monitor until symptoms and signs resolve [see Adverse Reactions (6.1)]. BASAGLAR is contraindicated in patients who have had hypersensitivity reactions to insulin glargine or one of the excipients [see Contraindications (4)].
5.6 Hypokalemia
All insulins, including BASAGLAR, cause a shift in potassium from the extracellular to intracellular space, possibly leading to hypokalemia. Untreated hypokalemia may cause respiratory paralysis, ventricular arrhythmia, and death. Monitor potassium levels in patients at risk for hypokalemia if indicated (e.g., patients using potassium-lowering medications, patients taking medications sensitive to serum potassium concentrations).
5.7 Fluid Retention and Heart Failure with Concomitant Use of PPAR-gamma Agonists
Thiazolidinediones (TZDs), which are peroxisome proliferator-activated receptor (PPAR)-gamma agonists, can cause dose-related fluid retention, particularly when used in combination with insulin. Fluid retention may lead to or exacerbate heart failure. Patients treated with insulin, including BASAGLAR, and a PPAR-gamma agonist should be observed for signs and symptoms of heart failure. If heart failure develops, it should be managed according to current standards of care, and discontinuation or dose reduction of the PPAR-gamma agonist must be considered.
6. Adverse Reactions/Side Effects
The following adverse reactions are discussed elsewhere:
- Hypoglycemia [see Warnings and Precautions (5.3)].
- Hypoglycemia Due to Medication Errors [see Warnings and Precautions (5.4)].
- Hypersensitivity Reactions [see Warnings and Precautions (5.5)].
- Hypokalemia [see Warnings and Precautions (5.6)].
6.1 Clinical Trial Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates observed in the clinical trials of a drug cannot be directly compared to rates in the clinical trials of another drug and may not reflect the rates observed in practice.
Two clinical trials with BASAGLAR were conducted: one in type 1 diabetes and one in type 2 diabetes.
The type 1 diabetes population had the following characteristics: Mean age was 41 years and mean duration of diabetes was 16 years. 58% were male. 75% were Caucasian, 2% Black or African American and 4% American Indian or Alaskan native. 4% were Hispanic. At baseline, mean eGFR was 109 mL/min/1.73m2. 73.5 percent of patients had eGFR>90 mL/min/1.73m2. The mean BMI was approximately 26 kg/m2. HbA1c at baseline was 7.8%. The data in Table 1 reflect exposure of 268 patients to BASAGLAR with a mean exposure duration of 49 weeks.
The type 2 diabetes population had the following characteristics: Mean age was 59 years and mean duration of diabetes was 11 years. 50% were male. 78% were Caucasian, 8% Black or African American and 5% American Indian or Alaskan native. 28% were Hispanic. At baseline, mean eGFR was 109 mL/min/1.73m2. 67.5 percent of patients had eGFR>90 mL/min/1.73m2. The mean BMI was approximately 32 kg/m2. HbA1c at baseline was 8.3%. The data in Table 2 reflect exposure of 376 patients to BASAGLAR with a mean exposure duration of 22 weeks.
Common adverse reactions were defined as reactions occurring in ≥5% of the population studied. Common adverse reactions during clinical trials in patients with type 1 diabetes mellitus and type 2 diabetes mellitus (other than hypoglycemia) are listed in Table 1 and Table 2, respectively.
|
a Infections other than nasopharyngitis or upper respiratory tract infection. |
|
| BASAGLAR + Insulin Lispro, % (n=268) |
|
| Infectiona | 24 |
| Nasopharyngitis | 16 |
| Upper respiratory tract infection | 8 |
|
a Infections other than nasopharyngitis or upper respiratory tract infection. |
|
| BASAGLAR + Oral Antidiabetic Medication, % (n=376) |
|
| Infectiona | 17 |
| Nasopharyngitis | 6 |
| Upper respiratory tract infection | 5 |
The frequencies of adverse reactions during a clinical trial of 5 years duration with another insulin glargine product, 100 units/mL, in patients with type 2 diabetes mellitus are listed in Table 3.
| Another Insulin Glargine Product, % (n=514) | NPH, % (n=503) |
|
| Hypertension | 20 | 19 |
| Sinusitis | 19 | 18 |
| Cataract | 18 | 16 |
| Bronchitis | 15 | 14 |
| Back pain | 13 | 12 |
| Cough | 12 | 7 |
| Urinary tract infection | 11 | 10 |
| Diarrhea | 11 | 10 |
| Depression | 11 | 10 |
| Headache | 10 | 9 |
The frequencies of adverse reactions during clinical trials with another insulin glargine product, 100 units/mL, in children and adolescents with type 1 diabetes mellitus are listed in Table 4.
| Another Insulin Glargine Product, %
(n=174) | NPH, %
(n=175) |
|
| Rhinitis | 5 | 5 |
Severe Hypoglycemia
Hypoglycemia is the most commonly observed adverse reaction in patients using insulin, including BASAGLAR. The rates of reported hypoglycemia depend on the definition of hypoglycemia used, diabetes type, insulin dose, intensity of glucose control, background therapies, and other intrinsic and extrinsic patient factors. For these reasons, comparing rates of hypoglycemia in clinical trials for BASAGLAR with the incidence of hypoglycemia for other products may be misleading and also, may not be representative of hypoglycemia rates that will occur in clinical practice.
Severe symptomatic hypoglycemia was defined as an event with symptoms consistent with hypoglycemia requiring the assistance of another person and associated with either a blood glucose below 50 mg/dL (≤56 mg/dL in the 5-year trial and ≤36 mg/dL in the ORIGIN trial) or prompt recovery after oral carbohydrate, intravenous glucose or glucagon administration.
The incidence of severe symptomatic hypoglycemia in patients receiving BASAGLAR with type 1 diabetes mellitus and type 2 diabetes mellitus [see Clinical Studies (14)] was 4% at 52 weeks and 1% at 24 weeks, respectively.
The incidence of severe symptomatic hypoglycemia in a clinical trial with another insulin glargine product, 100 units/mL, in children and adolescents age 6 to 15 years with type 1 diabetes [see Clinical Studies (14)] was 23% at 26 weeks.
Table 5 displays the proportion of patients experiencing severe symptomatic hypoglycemia in another insulin glargine product, 100 units/mL, and Standard Care groups in the ORIGIN Trial [see Clinical Studies (14)].
| ORIGIN Trial
Median duration of follow-up: 6.2 years |
||
| Another Insulin Glargine Product, 100 units/mL (N=6231) | Standard Care (N=6273) |
|
| Percent of patients | 6 | 2 |
Allergic Reactions
Some patients taking insulins, including BASAGLAR have experienced erythema, local edema, and pruritus at the site of injection. These conditions were usually self-limiting. Severe cases of generalized allergy (anaphylaxis) have been reported.
Peripheral Edema
Some patients taking BASAGLAR have experienced sodium retention and edema, particularly if previously poor metabolic control is improved by intensified insulin therapy.
Lipodystrophy
Administration of insulins subcutaneously, including BASAGLAR, has resulted in lipoatrophy (depression in the skin) or lipohypertrophy (enlargement or thickening of tissue) in some patients [see Dosage and Administration (2.1)].
6.2 Immunogenicity
As with all therapeutic proteins, there is potential for immunogenicity.
In a 52-week study of type 1 diabetes patients, 42% of patients who received BASAGLAR once daily were positive for anti-drug antibodies (ADA) at least once during the study, including 17% that were positive at baseline and 25% of patients who developed ADA during the study. Sixty-five percent of the ADA positive patients on BASAGLAR with antibody testing at week 52 remained ADA positive at week 52.
In a 24-week study of type 2 diabetes patients, 17% of patients who received BASAGLAR once daily were positive for ADA at least once during the study. Among the subjects who were positive, 5% had ADA at baseline and 12% developed antibodies during the study. The percent binding of patients positive at baseline on BASAGLAR did not increase significantly during the study. Fifty-one percent of the ADA positive patients on BASAGLAR with antibody testing at week 24 remained ADA positive at week 24. There was no evidence that these antibodies had an impact on efficacy and safety outcomes.
The detection of antibody formation is highly dependent on the sensitivity and specificity of the assay and may be influenced by several factors such as: assay methodology, sample handling, timing of sample collection, concomitant medication, and underlying disease. For these reasons, comparison of the incidence of antibodies to BASAGLAR with the incidence of antibodies in other studies or to other products may be misleading.
6.3 Postmarketing Experience
The following adverse reactions have been identified during post-approval use of insulin glargine. Because these reactions are reported voluntarily from a population of uncertain size, it is not always possible to estimate reliably their frequency or establish a causal relationship to drug exposure.
Medication errors have been reported in which other insulin products, particularly rapid-acting insulins, have been accidentally administered instead of insulin glargine.
Localized cutaneous amyloidosis at the injection site has occurred. Hyperglycemia has been reported with repeated insulin injections into areas of localized cutaneous amyloidosis; hypoglycemia has been reported with a sudden change to an unaffected injection site.
Related/similar drugs
7. Drug Interactions
Table 6 includes clinically significant drug interactions with BASAGLAR
| Drugs That May Increase the Risk of Hypoglycemia | |
| Drugs: | Antidiabetic agents, ACE inhibitors, angiotensin II receptor blocking agents, disopyramide, fibrates, fluoxetine, monoamine oxidase inhibitors, pentoxifylline, pramlintide, salicylates, somatostatin analogs (e.g., octreotide), and sulfonamide antibiotics. |
| Intervention: | Dose reductions and increased frequency of glucose monitoring may be required when BASAGLAR is co-administered with these drugs. |
| Drugs That May Decrease the Blood Glucose Lowering Effect of BASAGLAR | |
| Drugs: | Atypical antipsychotics (e.g., olanzapine and clozapine), corticosteroids, danazol, diuretics, estrogens, glucagon, isoniazid, niacin, oral contraceptives, phenothiazines, progestogens (e.g., in oral contraceptives), protease inhibitors, somatropin, sympathomimetic agents (e.g., albuterol, epinephrine, terbutaline), and thyroid hormones |
| Intervention: | Dose increases and increased frequency of glucose monitoring may be required when BASAGLAR is co-administered with these drugs. |
| Drugs That May Increase or Decrease the Blood Glucose Lowering Effect of BASAGLAR | |
| Drugs: | Alcohol, beta-blockers, clonidine, and lithium salts. Pentamidine may cause hypoglycemia, which may sometimes be followed by hyperglycemia. |
| Intervention: | Dose adjustment and increased frequency of glucose monitoring may be required when BASAGLAR is co-administered with these drugs. |
| Drugs That May Blunt Signs and Symptoms of Hypoglycemia | |
| Drugs: | beta-blockers, clonidine, guanethidine, and reserpine |
| Intervention: | Increased frequency of glucose monitoring may be required when BASAGLAR is co-administered with these drugs. |
8. Use In Specific Populations
8.1 Pregnancy
Risk Summary
Published studies with use of insulin glargine products during pregnancy have not reported a clear
association with insulin glargine products and adverse developmental outcomes (see Data). There are risks to the mother and fetus associated with poorly controlled diabetes in pregnancy (see Clinical Considerations). In animal reproduction studies, another insulin glargine product was administered to rats before, during and throughout pregnancy at doses up to 7 times the clinical dose of 10 units/day and to rabbits during organogenesis at doses approximately 2 times the clinical dose of 10 units/day. The effects of this other insulin glargine product did not generally differ from those observed with regular human insulin in rats or rabbits (see Data).
The estimated background risk of major birth defects is 6-10% in women with pre-gestational diabetes with a HbA1c >7 and has been reported to be as high as 20-25% in women with a HbA1c >10. The estimated background risk of miscarriage for the indicated population is unknown. In the US general population, the estimated background risk of major birth defects and miscarriage in clinically recognized pregnancies is 2-4% and 15-20%, respectively.
Disease-associated maternal and/or embryo/fetal risk
Poorly controlled diabetes in pregnancy increases the maternal risk for diabetic ketoacidosis, pre-eclampsia, spontaneous abortions, preterm delivery, and delivery complications. Poorly controlled diabetes increases the fetal risk for major birth defects, stillbirth, and macrosomia related morbidity.
Human Data
Published data do not report a clear association with insulin glargine products and major birth defects, miscarriage, or adverse maternal or fetal outcomes when insulin glargine products are used during pregnancy. However, these studies cannot definitely establish the absence of any risk because of methodological limitations including small sample size and some with no comparative group.
Animal Data
Subcutaneous reproduction and teratology studies have been performed with another insulin glargine product and with regular human insulin in rats and Himalayan rabbits. This other insulin glargine product was given to female rats before mating, during mating, and throughout pregnancy at dose up to 0.36 mg/kg/day, which is approximately 7 times the recommended human subcutaneous starting dose of 10 units/day (0.008 mg/kg/day) based on mg/m2. In rabbits, doses of 0.072 mg/kg/day, which is approximately 2 times the recommended human subcutaneous starting dose of 10 units/day (0.008 mg/kg/day), based on mg/m2, were administered during organogenesis. The effects of this other insulin glargine product did not generally differ from those observed with regular human insulin in rats and rabbits. However, in rabbits, five fetuses from two litters of the high-dose group exhibited dilation of the cerebral ventricles. Fertility and early embryonic development appeared normal.
8.2 Lactation
Risk Summary
There are no data on the presence of insulin glargine in human milk, the effects on the breastfed infant, or the effects on milk production. Endogenous insulin is present in human milk.
The developmental and health benefits of breastfeeding should be considered along with the mother's clinical need for BASAGLAR and any potential adverse effects on the breastfed child from BASAGLAR or from the underlying maternal condition.
8.4 Pediatric Use
The safety and effectiveness of BASAGLAR have been established in pediatric patients (age 6 to 15 years) with type 1 diabetes based on an adequate and well-controlled trial of another insulin glargine product, 100 units/mL, in pediatric patients (age 6 to 15 years) with type 1 diabetes and additional data in adults with type 1 diabetes [see Clinical Studies (14.2)]. The safety and effectiveness of BASAGLAR in pediatric patients younger than 6 years of age with type 1 diabetes and pediatric patients with type 2 diabetes has not been established.
In the pediatric clinical trial, pediatric patients (age 6 to 15 years) with type 1 diabetes had a higher incidence of severe symptomatic hypoglycemia compared to the adults in trials with type 1 diabetes [see Adverse Reactions (6.1)].
8.5 Geriatric Use
Of the total number of subjects in clinical studies of patients with type 2 diabetes who were treated with BASAGLAR or another insulin glargine product, 100 units/mL, each in combination with oral agents in a controlled clinical trial environment, 28.3% were 65 and over, while 4.5% were 75 and over. No overall differences in safety or effectiveness were observed between these subjects and younger subjects, and other reported clinical experience has not identified differences in responses between the elderly and younger patients, but greater sensitivity of some older individuals cannot be ruled out.
Nevertheless, caution should be exercised when BASAGLAR is administered to geriatric patients. In elderly patients with diabetes, the initial dosing, dose increments, and maintenance dosage should be conservative to avoid hypoglycemic reactions. Hypoglycemia may be difficult to recognize in the elderly.
8.6 Renal Impairment
The effect of renal impairment on the pharmacokinetics of BASAGLAR has not been studied. Some studies with human insulin have shown increased circulating levels of insulin in patients with renal failure. Frequent glucose monitoring and dose adjustment may be necessary for BASAGLAR in patients with renal impairment [see Warnings and Precautions (5.3)].
8.7 Hepatic Impairment
The effect of hepatic impairment on the pharmacokinetics of BASAGLAR has not been studied. However, as with all insulin products, more frequent glucose monitoring and dose adjustment may be necessary for BASAGLAR in patients with hepatic impairment [see Warnings and Precautions (5.3)].
10. Overdosage
Excess insulin administration relative to food intake, energy expenditure, or both may lead to severe and sometimes prolonged and life-threatening hypoglycemia and hypokalemia [see Warnings and Precautions (5.3, 5.6)]. Mild episodes of hypoglycemia can be treated with oral glucose. Adjustments in drug dosage, meal patterns, or physical activity level may be needed. More severe episodes with coma, seizure, or neurologic impairment may be treated with a glucagon product for emergency use or concentrated intravenous glucose. Sustained carbohydrate intake and observation may be necessary because hypoglycemia may recur after apparent clinical recovery. Hypokalemia must be corrected appropriately.
11. Basaglar Description
Insulin glargine is a long-acting human insulin analog produced by recombinant DNA technology utilizing a non-pathogenic laboratory strain of Escherichia coli (K12) as the production organism. Insulin glargine differs from human insulin in that the amino acid asparagine at position A21 is replaced by glycine and two arginines are added to the C-terminus of the B-chain. Chemically, insulin glargine is 21A-Gly-30B-a-L-Arg-30Bb-L-Arg-human insulin and has the empirical formula C267H404N72O78S6 and a molecular weight of 6.063 kDa. Insulin glargine has the following structural formula:
BASAGLAR (insulin glargine) injection is a sterile clear and colorless aqueous solution for subcutaneous use. Each mL contains 100 units of insulin glargine (3.6378 mg).
The 3 mL BASAGLAR prefilled pen presentations contain the following inactive ingredients per mL: glycerin (17 mg), metacresol (2.7 mg), zinc oxide (content adjusted to provide 30 mcg zinc ion), and Water for Injection, USP.
The pH is adjusted by addition of aqueous solutions of hydrochloric acid 10% and/or sodium hydroxide 10%. BASAGLAR has a pH of approximately 4.
12. Basaglar - Clinical Pharmacology
12.1 Mechanism of Action
The primary activity of insulin, including insulin glargine, is regulation of glucose metabolism. Insulin and its analog lower blood glucose by stimulating peripheral glucose uptake, especially by skeletal muscle and fat, and by inhibiting hepatic glucose production. Insulin inhibits lipolysis and proteolysis, and enhances protein synthesis.
12.2 Pharmacodynamics
The pharmacodynamic profile for BASAGLAR was determined after subcutaneous administration of a single 0.5 U/kg dose in a euglycemic clamp study conducted in 91 healthy subjects. The median time to maximum effect of BASAGLAR (measured by the peak rate of glucose infusion) was approximately 12.0 hours. The pharmacodynamic profile of BASAGLAR following subcutaneous injection demonstrated sustained glucose lowering activity over 24 hours with no pronounced peak. The mean area under the glucose infusion rate curves (measure of overall pharmacodynamic effect) and maximum glucose infusion rate were 1670 mg/kg and 2.12 mg/kg/min, respectively.
A euglycemic clamp study in 20 patients with type 1 diabetes showed a similar pharmacodynamic profile with a sustained glucose lowering activity over 24 hours following a single 0.3 U/kg subcutaneous dose of BASAGLAR.
After subcutaneous injection of 0.3 units/kg of another insulin glargine product, 100 units/mL, in patients with type 1 diabetes, the duration of action after abdominal, deltoid, or thigh subcutaneous administration was similar.
The time course of action of insulins, including insulin glargine, may vary between individuals and within the same individual.
12.3 Pharmacokinetics
Absorption and Bioavailability
The pharmacokinetic profile for BASAGLAR was determined after subcutaneous administration of a single 0.5 U/kg dose in a euglycemic clamp study conducted in 91 healthy subjects. The insulin serum concentrations indicated a slow and prolonged absorption and a relatively constant concentration/time profile over 24 hours with no pronounced peak.
The median time to maximum serum insulin concentration was 12 hours after injection. On average, serum insulin concentrations declined to baseline by approximately 24 hours. The mean observed area under the serum insulin concentration-time curve from time zero to 24 hours and peak serum insulin concentration were 1720 pmol*hr/L and 103 pmol/L, respectively.
Metabolism and Elimination
After subcutaneous injection of another insulin glargine product, 100 units/mL, in diabetic patients, insulin glargine is metabolized at the carboxyl terminus of the Beta chain with formation of two active metabolites M1 (21A-Gly-insulin) and M2 (21A-Gly-des-30B-Thr-insulin). The in vitro activity of M1 and M2 were similar to that of insulin.
13. Nonclinical Toxicology
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
In mice and rats, standard two-year carcinogenicity studies with another insulin glargine product were performed at doses up to 0.455 mg/kg, which was for the rat approximately 10 times and for the mouse approximately 5 times the recommended human subcutaneous starting dose of 10 units/day (0.008 mg/kg/day), based on mg/m2. The findings in female mice were not conclusive due to excessive mortality in all dose groups during the study. Histiocytomas were found at injection sites in male rats (statistically significant) and male mice (not statistically significant) in acid vehicle containing groups. These tumors were not found in female animals, in saline control, or insulin comparator groups using a different vehicle. The relevance of these findings to humans is unknown.
Another insulin glargine product was not mutagenic in tests for detection of gene mutations in bacteria and mammalian cells (Ames- and HGPRT-test) and in tests for detection of chromosomal aberrations (cytogenetics in vitro in V79 cells and in vivo in Chinese hamsters).
In a combined fertility and prenatal and postnatal study of another insulin glargine product in male and female rats at subcutaneous doses up to 0.36 mg/kg/day, which was approximately 7 times the recommended human subcutaneous starting dose of 10 units/day (0.008 mg/kg/day), based on mg/m2, maternal toxicity due to dose-dependent hypoglycemia, including some deaths, was observed. Consequently, a reduction of the rearing rate occurred in the high-dose group only. Similar effects were observed with NPH insulin.
14. Clinical Studies
14.1 Overview of Clinical Studies
The safety and effectiveness of another insulin glargine product, 100 units/mL, given once-daily at bedtime was compared to that of once-daily and twice-daily NPH insulin in open-label, randomized, active-controlled, parallel studies of 2,327 adults and 349 pediatric patients with type 1 diabetes mellitus and 1,563 adult patients with type 2 diabetes mellitus (see Tables 8, 9, 11, and 12). In general, the reduction in glycated hemoglobin (HbA1c) with this other insulin glargine product was similar to that with NPH insulin.
14.2 Clinical Studies in Adult and Pediatric Patients with Type 1 Diabetes
Patients with inadequately controlled type 1 diabetes participated in a 24-week open-label, active-controlled study with a 28 week extension to evaluate the glucose lowering effect of once-daily BASAGLAR compared to that of once-daily administration of another insulin glargine product, 100 units/mL, or a non-U.S.-licensed insulin glargine, 100 units/mL, (comparator insulin glargine products, 100 units/mL) both in combination with mealtime insulin lispro. Randomized were 535 adults with type 1 diabetes. Mean age was 41.2 years and mean duration of diabetes was 16.39 years. 57.9% were male. 74.5% were Caucasian, 2.1% Black or African American and 4.3% American Indian or Alaskan native. 3.9% were Hispanic. 73.5 percent of patients had GFR>90 mL/min/1.73m2. The mean BMI was approximately 25.54 kg/m2. At week 24, treatment with BASAGLAR provided a mean reduction in HbA1c that was non-inferior to that achieved with comparator insulin glargine products, 100 units/mL (see Table 7).
|
a One patient randomized to the BASAGLAR group was not included in the Full Analysis Set. |
||
|
b “Comparator insulin glargine products, 100 units/mL” refers to another insulin glargine product, 100 units/mL, and a non-U.S.-licensed insulin glargine, 100 units/mL, used in this study. |
||
|
c ANCOVA Model includes treatment, country and time of baseline basal insulin injection (daytime or evening/bedtime) as fixed effects and baseline HbA1c as covariate. |
||
|
d The results were calculated based on the number of patients in the Full Analysis Set using their last observed post-baseline value of HbA1c. Observed HbA1c data at 24 weeks were available from 256 (95.5%) and 258 (96.6%) subjects randomized to the BASAGLAR and comparator insulin glargine products, 100 units/mL, groups, respectively. |
||
| Efficacy Parameter | BASAGLAR + insulin lispro (N=268a) | Comparator Insulin Glargine Products, 100 units/mLb
+ insulin lispro (N=267) |
| HbA1c (%) | ||
| Baseline (mean) | 7.75 | 7.79 |
| Change from baseline (adjusted meanc,d) | -0.35 | -0.46 |
| Difference from comparator (adjusted meanc,d) (95% CI) | 0.11 (-0.002, 0.219) |
|
| Proportion of patients achieving HbA1c <7%d | 34.5% | 32.2% |
In two clinical studies (Studies A and B), patients with type 1 diabetes (Study A; n=585, Study B; n=534) were randomized to 28 weeks of basal-bolus treatment with another insulin glargine product, 100 units/mL, or NPH insulin. Regular human insulin was administered before each meal. This other insulin glargine product was administered at bedtime. NPH insulin was administered once daily at bedtime or in the morning and at bedtime when used twice daily. In Study A, the average age was 39.2 years. The majority of patients were Caucasian (99%) and 55.7% were male. The mean BMI was approximately 24.9 kg/m2. The mean duration of diabetes was 15.5 years. In Study B, the average age was 38.5 years. The majority of patients were Caucasian (95.3%) and 50.6% were male. The mean BMI was approximately 25.8 kg/m2. The mean duration of diabetes was 17.4 years.
In another clinical study (Study C), patients with type 1 diabetes (n=619) were randomized to 16 weeks of basal-bolus treatment with another insulin glargine product, 100 units/mL, or NPH insulin. Insulin lispro was used before each meal. This other insulin glargine product was administered once daily at bedtime and NPH insulin was administered once or twice daily. The average age was 39.2 years. The majority of patients were Caucasian (96.9%) and 50.6% were male. The mean BMI was approximately 25.6 kg/m2. The mean duration of diabetes was 18.5 years.
In these 3 studies, another insulin glargine product, 100 units/mL, and NPH insulin had similar effects on HbA1c (see Table 8) with a similar overall rate of hypoglycemia [see Adverse Reactions (6.1)].
| Treatment duration
Treatment in combination with | Study A 28 weeks Regular insulin | Study B 28 weeks Regular insulin | Study C 16 weeks Insulin lispro |
||||
| Another Insulin Glargine Product | NPH | Another Insulin Glargine Product | NPH | Another Insulin Glargine Product | NPH | ||
| Number of subject treated | 292 | 293 | 264 | 270 | 310 | 309 | |
| HbA1c (%) | |||||||
| Baseline (mean) | 8.0 | 8.0 | 7.7 | 7.7 | 7.6 | 7.7 | |
| Adjusted mean change at trial end | +0.2 | +0.1 | -0.2 | -0.2 | -0.1 | -0.1 | |
| Treatment Difference (95% CI) | +0.1 (0.0; + 0.2) | +0.1(-0.1; + 0.2) | 0.0 (+0.1; + 0.1) | ||||
| Fasting blood glucose (mg/dL) | |||||||
| Baseline (mean) | 167 | 166 | 166 | 175 | 175 | 173 | |
| Adjusted mean change at trial end | -21 | -16 | -20 | -17 | -29 | -12 | |
Type 1 Diabetes – Pediatric (see Table 9)
The efficacy of BASAGLAR to improve glycemic control in pediatric patients with type 1 diabetes mellitus is based on an adequate and well-controlled trial of another insulin glargine product, 100 units/mL, in pediatric patients with type 1 diabetes mellitus (Study D). In this randomized, active-controlled clinical study (Study D), pediatric patients (age range 6 to 15 years) with type 1 diabetes (n=349) were treated for 28 weeks with a basal-bolus insulin regimen where regular human insulin was used before each meal. Patients were randomized to either this other insulin glargine product administered once daily at bedtime or NPH insulin administered once or twice daily. The average age was 11.7 years. The majority of patients were Caucasian (96.8%) and 51.9% were male. The mean BMI was approximately 18.9 kg/m2. The mean duration of diabetes was 4.8 years. Similar effects on HbA1c (see Table 9) were observed in both treatment groups.
| Study D | ||
| Another Insulin Glargine Product + Regular Insulin | NPH + Regular Insulin | |
| Number of subjects treated | 174 | 175 |
| HbA1c | ||
| Baseline mean | 8.5 | 8.8 |
| Change from baseline (adjusted mean) | +0.3 | +0.3 |
| Difference from NPH (adjusted mean) (95% CI) | 0.0 (-0.2; +0.3) |
|
| Fasting blood glucose (mg/dL) | ||
| Baseline mean | 194 | 191 |
| Mean change from baseline | -23 | -12 |
14.3 Clinical Studies in Adults with Type 2 Diabetes
Patients with type 2 diabetes participated in a double-blind, active-controlled study to evaluate the glucose lowering effect of once-daily BASAGLAR plus oral antidiabetic medication (OAM) compared to that of another insulin glargine product, 100 units/mL, or a non-U.S.-licensed insulin glargine, 100 units/mL (comparator insulin glargine products, 100 units/mL) administered once-daily along with OAMs. Patients were either insulin naïve (approximately 60%) and had failed to achieve adequate glycemic control on at least 2 OAMs, or were already on another insulin glargine product, 100 units/mL, or a non-U.S.-licensed insulin glargine, 100 units/mL, along with at least 2 OAMs with adequate or inadequate glycemic control (approximately 40%). A total of 759 patients were randomized. Three patients randomized to BASAGLAR did not receive study drug and were not included in efficacy analysis. The average age was approximately 59 years. The majority of patients were White (78%) and 50% of the patients were male. Sixty-eight percent of patients had GFR>90 mL/min/1.73m2. The mean BMI was approximately 32 kg/m2. At week 24, treatment with BASAGLAR provided a mean reduction in HbA1c that was non-inferior to that achieved with comparator insulin glargine products, 100 units/mL (see Table 10).
|
a Three patients randomized to BASAGLAR did not receive study drug and were not included in the Full Analysis Set. |
||
|
b “Comparator insulin glargine products, 100 units/mL” refers to another insulin glargine product, 100 units/mL, and a non-U.S.-licensed insulin glargine, 100 units/mL, used in this study. |
||
|
c ANCOVA Model includes treatment, country, sulfonylurea use and time of baseline basal insulin injection (daytime or evening/bedtime) as fixed effects and baseline HbA1c as covariate. |
||
|
d The results were calculated based on the number of patients in the Full Analysis Set using their last observed post-baseline value of HbA1c. Observed HbA1c data at 24 weeks were available from 331 (88%) and 329 (87%) subjects randomized to the BASAGLAR and comparator insulin glargine products, 100 units/mL, groups, respectively. |
||
| BASAGLAR + Oral Antidiabetic Medication (N=376)a | Comparator Insulin Glargine Products, 100 units/mLb + Oral Antidiabetic Medication (N=380) | |
| HbA1c (%) | ||
| Baseline (mean) | 8.35 | 8.31 |
| Change from baseline (adjusted meanc,d) | -1.3 | -1.3 |
| Difference from comparator (adjusted meanc,d) (95% CI) | 0.05 (-0.07, 0.17) |
|
| Proportion of patients achieving HbA1c <7%d | 48.8% | 52.5% |
In a randomized, controlled clinical study (Study E) (n=570), another insulin glargine product, 100 units/mL, was evaluated for 52 weeks in combination with oral anti-diabetic medications (a sulfonylurea, metformin, acarbose, or combination of these drugs). The average age was 59.5 years. The majority of patients were Caucasian (92.8%) and 53.7% were male. The mean BMI was approximately 29.1 kg/m2. The mean duration of diabetes was 10.3 years. This other insulin glargine product administered once daily at bedtime was as effective as NPH insulin administered once daily at bedtime in reducing HbA1c and fasting glucose (see Table 11). The rate of hypoglycemia was similar in this other insulin glargine product and NPH insulin treated patients [see Adverse Reactions (6.1)].
In a randomized, controlled clinical study (Study F), in patients with type 2 diabetes not using oral anti-diabetic medications (n=518), a basal-bolus regimen of another insulin glargine product, 100 units/mL, once daily at bedtime or NPH insulin administered once or twice daily was evaluated for 28 weeks. Regular human insulin was used before meals, as needed. The average age was 59.3 years. The majority of patients were Caucasian (80.7%) and 60% were male. The mean BMI was approximately 30.5 kg/m2. The mean duration of diabetes was 13.7 years. This other insulin glargine product had similar effectiveness as either once- or twice daily NPH insulin in reducing HbA1c and fasting glucose (see Table 11) with a similar incidence of hypoglycemia [see Adverse Reactions (6.1)].
In a randomized, controlled clinical study (Study G), patients with type 2 diabetes were randomized to 5 years of treatment with another insulin glargine product, 100 units/mL, once-daily or twice-daily NPH insulin. For patients not previously treated with insulin, the starting dose of this other insulin glargine product or NPH insulin was 10 units daily. Patients who were already treated with NPH insulin either continued on the same total daily NPH insulin dose or started this other insulin glargine product at a dose that was 80% of the total previous NPH insulin dose. The primary endpoint for this study was a comparison of the progression of diabetic retinopathy by 3 or more steps on the ETDRS scale. HbA1c change from baseline was a secondary endpoint. Similar glycemic control in the 2 treatment groups was desired in order to not confound the interpretation of the retinal data. Patients or study personnel used an algorithm to adjust this other insulin glargine product and NPH insulin doses to a target fasting plasma glucose ≤100 mg/dL. After this other insulin glargine product or NPH insulin dose was adjusted, other anti-diabetic agents, including pre-meal insulin were to be adjusted or added. The average age was 55.1 years. The majority of patients were Caucasian (85.3%) and 53.9% were male. The mean BMI was approximately 34.3 kg/m2. The mean duration of diabetes was 10.8 years. This other insulin glargine product group had a smaller mean reduction from baseline in HbA1c compared to the NPH insulin group, which may be explained by the lower daily basal insulin doses in this other insulin glargine product group (see Table 11). Both treatment groups had a similar incidence of reported symptomatic hypoglycemia. The incidence of severe symptomatic hypoglycemia in the ORIGIN Trial is given in Table 5 [see Adverse Reactions (6.1)].
| Treatment duration
Treatment in combination with | Study E 52 weeks Oral agents | Study F 28 weeks Regular insulin | Study G 5 years Regular insulin |
|||
| Another Insulin Glargine Product | NPH | Another Insulin Glargine Product | NPH | Another Insulin Glargine Product | NPH | |
| Number of subjects treated | 289 | 281 | 259 | 259 | 513 | 504 |
| HbA1c | ||||||
| Baseline mean | 9.0 | 8.9 | 8.6 | 8.5 | 8.4 | 8.3 |
| Adjusted mean change from baseline | -0.5 | -0.4 | -0.4 | -0.6 | -0.6 | -0.8 |
| Another insulin glargine product, 100 units/mL – NPH | -0.1 | +0.2 | +0.2 | |||
| 95% CI for Treatment difference | (-0.3; +0.1) | (0.0; +0.4) | (+0.1; +0.4) | |||
| Fasting blood glucose (mg/dL) | ||||||
| Baseline mean | 179 | 180 | 164 | 166 | 190 | 180 |
| Adjusted mean change from baseline | -49 | -46 | -24 | -22 | -45 | -44 |
Another Insulin Glargine Product, 100 units/mL, Timing of Daily Dosing (see Table 12)
The safety and efficacy of this other insulin glargine product administered pre-breakfast, pre-dinner, or at bedtime were evaluated in a randomized, controlled clinical study in patients with type 1 diabetes (Study H; n=378). Patients were also treated with insulin lispro at mealtime. The average age was 40.9 years. All patients were Caucasian (100%) and 53.7% were male. The mean BMI was approximately 25.3 kg/m2. The mean duration of diabetes was 17.3 years. This other insulin glargine product administered at different times of the day resulted in similar reductions in HbA1c compared to that with bedtime administration (see Table 12). In these patients, data are available from 8-point home glucose monitoring. The maximum mean blood glucose was observed just prior to injection of this other insulin glargine product regardless of time of administration.
In this study, 5% of patients in this other insulin glargine product-breakfast arm discontinued treatment because of lack of efficacy. No patients in the other two arms discontinued for this reason. The safety and efficacy of this other insulin glargine product administered pre-breakfast or at bedtime were also evaluated in a randomized, active-controlled clinical study (Study I, n=697) in patients with type 2 diabetes not adequately controlled on oral anti-diabetic therapy. All patients in this study also received glimepiride 3 mg daily. The average age was 60.8 years. The majority of patients were Caucasian (96.6%) and 53.7% were male. The mean BMI was approximately 28.7 kg/m2. The mean duration of diabetes was 10.1 years. This other insulin glargine product given before breakfast was at least as effective in lowering HbA1c as this other insulin glargine product given at bedtime or NPH insulin given at bedtime (see Table 12).
|
a Intent to treat. |
||||||
|
b Total number of patients evaluable for safety. |
||||||
|
c Not applicable. |
||||||
| Treatment duration
Treatment in combination with | Study H 24 weeks Insulin lispro | Study I 24 weeks Glimepiride |
||||
| Another Insulin Glargine Product Breakfast | Another Insulin Glargine Product Dinner | Another Insulin Glargine Product Bedtime | Another Insulin Glargine Product Breakfast | Another Insulin Glargine Product Bedtime | NPH
Bedtime |
|
| Number of subjects treateda | 112 | 124 | 128 | 234 | 226 | 227 |
| HbA1c | ||||||
| Baseline mean | 7.6 | 7.5 | 7.6 | 9.1 | 9.1 | 9.1 |
| Mean change from baseline | -0.2 | -0.1 | 0.0 | -1.3 | -1.0 | -0.8 |
Five-year Trial Evaluating the Progression of Retinopathy
Retinopathy was evaluated in clinical studies with another insulin glargine product, 100 units/mL, by analysis of reported retinal adverse events and fundus photography. The numbers of retinal adverse events reported for this other insulin glargine product and NPH insulin treatment groups were similar for patients with type 1 and type 2 diabetes.
Another insulin glargine product, 100 units/mL, was compared to NPH insulin in a 5-year randomized clinical trial that evaluated the progression of retinopathy as assessed with fundus photography using a grading protocol derived from the Early Treatment Diabetic Retinopathy Scale (ETDRS). Patients had type 2 diabetes (mean age 55 years) with no (86%) or mild (14%) retinopathy at baseline. Mean baseline HbA1c was 8.4%. The primary outcome was progression by 3 or more steps on the ETDRS scale at study endpoint. Patients with pre-specified post-baseline eye procedures (pan-retinal photocoagulation for proliferative or severe nonproliferative diabetic retinopathy, local photocoagulation for new vessels, and vitrectomy for diabetic retinopathy) were also considered as 3-step progressions regardless of actual change in ETDRS score from baseline. Retinopathy graders were blinded to treatment group assignment. The results for the primary endpoint are shown in Table 13 for both the per-protocol and Intent-to-Treat populations, and indicate similarity of this other insulin glargine product to NPH in the progression of diabetic retinopathy as assessed by this outcome.
|
a Difference = another insulin glargine product, 100 units/mL – NPH. |
||||
|
b Using a generalized linear model (SAS GENMOD) with treatment and baseline HbA1c strata (cutoff 9.0%) as the classified independent variables, and with binomial distribution and identity link function. |
||||
| Another Insulin Glargine Product, 100 units/mL (%) | NPH (%) | Differencea,b (SE) | 95% CI for difference | |
| Per-protocol | 53/374 (14.2%) | 57/363 (15.5%) | -2.0% (2.6%) | -7.0% to +3.1% |
| Intent-to-Treat | 63/502 (12.5%) | 71/487 (14.6%) | -2.1% (2.1%) | -6.3% to +2.1% |
The ORIGIN Study
The Outcome Reduction with Initial Glargine Intervention trial (i.e., ORIGIN) was an open-label, randomized, 2-by-2, factorial design study. One intervention in ORIGIN compared the effect of another insulin glargine product, 100 units/mL, to standard care on major adverse cardiovascular outcomes in 12,537 participants ≥50 years of age with abnormal glucose levels [i.e., impaired fasting glucose (IFG) and/or impaired glucose tolerance (IGT)] or early type 2 diabetes mellitus and established cardiovascular (i.e., CV) disease or CV risk factors at baseline.
The objective of the trial was to demonstrate that use of this other insulin glargine product could significantly lower the risk of major cardiovascular outcomes compared to standard care. Two co-primary composite cardiovascular endpoints were used in ORIGIN. The first co-primary endpoint was the time to first occurrence of a major adverse cardiovascular event defined as the composite of CV death, nonfatal myocardial infarction and nonfatal stroke. The second co-primary endpoint was the time to the first occurrence of CV death or nonfatal myocardial infarction or nonfatal stroke or revascularization procedure or hospitalization for heart failure.
Participants were randomized to either this other insulin glargine product (N=6264) titrated to a goal fasting plasma glucose of ≤95 mg/dL or to standard care (N=6273). Anthropometric and disease characteristics were balanced at baseline. The mean age was 64 years and 8% of participants were 75 years of age or older. The majority of participants were male (65%). Fifty nine percent were Caucasian, 25% were Latin, 10% were Asian and 3% were Black. The median baseline BMI was 29 kg/m2. Approximately 12% of participants had abnormal glucose levels (IGT and/or IFG) at baseline and 88% had type 2 diabetes. For patients with type 2 diabetes, 59% were treated with a single oral antidiabetic drug, 23% had known diabetes but were on no antidiabetic drug and 6% were newly diagnosed during the screening procedure. The mean HbA1c (SD) at baseline was 6.5% (1.0). Fifty nine percent of participants had had a prior cardiovascular event and 39% had documented coronary artery disease or other cardiovascular risk factors.
Vital status was available for 99.9% and 99.8% of participants randomized to this other insulin glargine product and standard care respectively at end of trial. The median duration of follow-up was 6.2 years [range: 8 days to 7.9 years]. The mean HbA1c (SD) at the end of the trial was 6.5% (1.1) and 6.8% (1.2) in this other insulin glargine product and standard group respectively. The median dose of this other insulin glargine product at end of trial was 0.45 U/kg. Eighty-one percent of patients randomized to this other insulin glargine product were using this other insulin glargine product at end of the study. The mean change in body weight from baseline to the last treatment visit was 2.2 kg greater in this other insulin glargine group than in the standard care group.
Overall, the incidence of major adverse cardiovascular outcomes was similar between groups (see Table 14). All-cause mortality was also similar between groups.
| Another Insulin Glargine Product, 100 units/mL N=6264 | Standard Care
N=6273 | Another Insulin Glargine Product, 100 units/mL vs. Standard Care | |
| n (Events per 100 PY) | n (Events per 100 PY) |
Hazard Ratio (95% CI) |
|
| Co-primary endpoints | |||
| CV death, nonfatal myocardial infarction, or nonfatal stroke | 1041 (2.9) | 1013 (2.9) | 1.02 (0.94, 1.11) |
| CV death, nonfatal myocardial infarction, nonfatal stroke, hospitalization for heart failure or revascularization procedure | 1792 (5.5) | 1727 (5.3) | 1.04 (0.97, 1.11) |
| Components of co-primary endpoints | |||
| CV death | 580 | 576 | 1.00 (0.89, 1.13) |
| Myocardial Infarction (fatal or nonfatal) | 336 | 326 | 1.03 (0.88, 1.19) |
| Stroke (fatal or nonfatal) | 331 | 319 | 1.03 (0.89, 1.21) |
| Revascularizations | 908 | 860 | 1.06 (0.96, 1.16) |
| Hospitalization for heart failure | 310 | 343 | 0.90 (0.77, 1.05) |
In the ORIGIN trial, the overall incidence of cancer (all types combined) or death from cancer in the ORIGIN trial (see Table 15) was similar between treatment groups.
| Another Insulin Glargine Product, 100 units/mL N=6264 | Standard Care
N=6273 | Another Insulin Glargine Product, 100 units/mL vs. Standard Care | |
| n (Events per 100 PY) | n (Events per 100 PY) |
Hazard Ratio (95% CI) |
|
| Cancer endpoints | |||
| Any cancer event (new or recurrent) | 559 (1.56) | 561 (1.56) | 0.99 (0.88, 1.11) |
| New cancer events | 524 (1.46) | 535 (1.49) | 0.96 (0.85, 1.09) |
| Death due to Cancer | 189 (0.51) | 201 (0.54) | 0.94 (0.77, 1.15) |
16. How is Basaglar supplied
16.1 How Supplied
BASAGLAR (insulin glargine) injection is a clear, colorless solution, 100 units/mL (U-100), available as:
|
a Tempo Pen contains a component that allows for data connectivity when used with a compatible transmitter. |
|||
| BASAGLAR | Total Volume | NDC Number | Package Size |
| BASAGLAR single-patient-use KwikPen | 3 mL | 0002-7715-59 | 5 pens |
| BASAGLAR single-patient-use Tempo Pena | 3 mL | 0002-8214-05 | 5 pens |
The BASAGLAR KwikPen and Tempo Pen dial in 1 unit increments.
Needles are not included.
This device is recommended for use with Becton, Dickinson & Company's insulin pen needles which are sold separately.
16.2 Storage and Handling
Dispense in the original sealed carton with the enclosed Instructions for Use.
Protect BASAGLAR from heat and light. Do not freeze BASAGLAR.
In-use BASAGLAR prefilled pens must be used within 28 days or be discarded, even if they still contain BASAGLAR.
Storage conditions are summarized in the following table:
| Not In-Use (Unopened)
Room Temperature (up to 86°F [30°C]) | Not In-Use (Unopened)
Refrigerated (36°F to 46°F [2°C to 8°C]) | In-Use (Opened) Room Temperature, (up to 86°F [30°C]) | |
| 3 mL single-patient-use BASAGLAR KwikPen | 28 days | Until expiration date | 28 days, Do not refrigerate. |
| 3 mL single-patient-use BASAGAR Tempo Pen | 28 days | Until expiration date | 28 days, Do not refrigerate. |
17. Patient Counseling Information
See FDA-approved patient labeling (Patient Information and Instructions for Use).
Never Share a BASAGLAR Prefilled Pen Between Patients
Advise patients that they must never share a BASAGLAR prefilled pen with another person, even if the needle is changed, because doing so carries a risk for transmission of blood-borne pathogens [see Warnings and Precautions (5.1)].
Hyperglycemia or Hypoglycemia
Inform patients that hypoglycemia is the most common adverse reaction with insulin. Inform patients of the symptoms of hypoglycemia. Inform patients that the ability to concentrate and react may be impaired as a result of hypoglycemia. This may present a risk in situations where these abilities are especially important, such as driving or operating other machinery. Advise patients who have frequent hypoglycemia or reduced or absent warning signs of hypoglycemia to use caution when driving or operating machinery.
Advise patients that changes in insulin regimen can predispose to hyperglycemia or hypoglycemia and that changes in insulin regimen should be made under close medical supervision [see Warnings and Precautions (5.2)].
Medication errors
Inform patients to always check the insulin label before each injection [see Warnings and Precautions (5.4)].
|
This Patient Information has been approved by the U.S. Food and Drug Administration |
| Patient Information
BASAGLAR® (baz-a-glar) (insulin glargine) injection, for subcutaneous use 100 units/mL (U-100) |
| Do not share your BASAGLAR prefilled pen with other people, even if the needle has been changed. You may give other people a serious infection, or get a serious infection from them.
What is BASAGLAR?
|
| Who should not use BASAGLAR?
Do not use BASAGLAR if you:
|
| What should I tell my healthcare provider before using BASAGLAR?
Before using BASAGLAR, tell your healthcare provider about all your medical conditions, including if you:
|
| Tell your healthcare provider about all the medicines you take, including prescription and over-the-counter medicines, vitamins and herbal supplements. Before you start using BASAGLAR, talk to your healthcare provider about low blood sugar and how to manage it. |
How should I use BASAGLAR?
|
| Keep BASAGLAR and all medicines out of the reach of children. |
Your dose of BASAGLAR may need to change because of:
|
| What should I avoid while using BASAGLAR?
While using BASAGLAR do not:
|
| What are the possible side effects of BASAGLAR?
BASAGLAR may cause serious side effects that can lead to death, including:
|
| Treatment with TZDs and BASAGLAR may need to be changed or stopped by your healthcare provider if you have new or worse heart failure. Get emergency medical help if you have:
|
The most common side effects of BASAGLAR include:
|
| These are not all the possible side effects of BASAGLAR. Call your doctor for medical advice about side effects. You may report side effects to FDA at 1-800-FDA-1088 (1-800-332-1088). |
| General information about the safe and effective use of BASAGLAR.
Medicines are sometimes prescribed for purposes other than those listed in a Patient Information leaflet. Do not use BASAGLAR for a condition for which it was not prescribed. Do not give BASAGLAR to other people, even if they have the same symptoms that you have. It may harm them. This Patient Information leaflet summarizes the most important information about BASAGLAR. If you would like more information, talk with your healthcare provider. You can ask your pharmacist or healthcare provider for information about BASAGLAR that is written for health professionals. For more information, go to www.basaglar.com or call 1-800-545-5979. |
What are the ingredients in BASAGLAR?
|
| Patient Information revised: November 2023 |
| Manufactured by: Eli Lilly and Company, Indianapolis, IN 46285 USA US License Number 1891 Copyright © 2015, 2023, Eli Lilly and Company. All rights reserved. |
BAS-0006-PPI-20231129
BASAGLAR KWIKPEN INSTRUCTIONS FOR USE
Instructions for Use
BASAGLAR® KwikPen®
(insulin glargine)
injection, for subcutaneous use
100 units/mL, 3 mL single-patient-use pen
Read the Instructions for Use before you start using BASAGLAR and each time you get another BASAGLAR® KwikPen®. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Do not share your BASAGLAR KwikPen with other people, even if the needle has been changed. You may give other people a serious infection or get a serious infection from them.
BASAGLAR KwikPen (“Pen”) is a disposable single-patient-use prefilled pen containing 300 units (3mL) of BASAGLAR. One pen contains multiple doses of medicine.
- Your healthcare provider will tell you how many units to give as your dose and how to inject your prescribed dose of medicine.
- You can give a dose of 1 to 80 units in a single injection.
- If your prescribed dose is more than 80 units, you will need to give yourself more than 1 injection.
- The plunger only moves a little with each injection, and you may not notice that it moves. When the plunger reaches the end of the cartridge, you have used all 300 units in the Pen.
People who are blind or have vision problems should not use the Pen without help from a person trained to use the BASAGLAR prefilled pen.
How to recognize your BASAGLAR KwikPen
- Pen color: Light grey
- Dose Knob: Light grey with green ring on the end
- Labels: Light grey with green color bars
Supplies needed to give your injection
- BASAGLAR KwikPen
- KwikPen compatible Needle (Becton, Dickinson and Company Pen Needles recommended)
- Alcohol swab
Preparing your Pen
- Wash your hands with soap and water.
- Check the Pen to make sure you are taking the right type of insulin. This is especially important if you use more than 1 type of insulin.
- Do not use your Pen past the expiration date printed on the Label or for more than 28 days after you first start using the Pen.
- Always use a new needle for each injection to help prevent infections and blocked needles. Do not reuse or share your needles with other people. You may give other people a serious infection or get a serious infection from them.
Priming your Pen
Prime before each injection.
- Priming means removing the air from the Needle and Cartridge that may collect during normal use. It is important to prime your Pen before each injection so that it will work correctly.
- If you do not prime before each injection, you may get too much or too little insulin.
Selecting your dose
- If your dose is more than 80 units, you will need to give more than 1 injection.
- -
- Talk to your healthcare provider about how to give your dose.
- -
- Use a new Needle for each injection and repeat the priming step.
The Pen will not let you dial more than the number of units left in the Pen.
- If you need to inject more than the number of units left in the Pen, you may either:
- -
- inject the amount left in your Pen and then use a new Pen to give the rest of your dose, or
- -
- get a new Pen and inject the full dose.
- It is normal to see a small amount of insulin left in the Pen that you can not inject.
Giving your injection
- Inject your insulin as your healthcare provider has shown you.
- Change (rotate) your injection sites within the area you choose for each dose to reduce your risk of getting lipodystrophy (pits in skin or thickened skin) and localized cutaneous amyloidosis (skin with lumps) at the injection sites. Do not inject where the skin has pits, is thickened, or has lumps. Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin.
- Do not try to change your dose while injecting.
After your injection
Disposing of Pens and Needles
- Put your used needles in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles in your household trash.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- -
- made of a heavy-duty plastic,
- -
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- -
- upright and stable during use,
- -
- leak-resistant, and
- -
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- The used Pen may be discarded in your household trash after you have removed the needle.
Storing your BASAGLAR KwikPen
Unused Pens
- Store unused Pens in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Do not freeze BASAGLAR. Do not use if it has been frozen.
- Unused Pens may be used until the expiration date printed on the Label, if the Pen has been kept in the refrigerator.
In-use Pen
- Store the Pen you are currently using at room temperature [up to 86°F (30°C)] and away from heat and light.
- Throw away the Pen you are using after 28 days, even if it still has insulin left in it.
General information about the safe and effective use of your Pen
- Keep your Pen and needles out of the sight and reach of children.
- Always use a new needle for each injection.
- Do not share your Pen or needles with other people. You may give other people a serious infection or get a serious infection from them.
- Do not use your Pen if any part looks broken or damaged.
- Always carry an extra Pen in case yours is lost or damaged.
Troubleshooting
- If you can not remove the Pen Cap, gently twist the cap back and forth, and then pull the cap straight off.
- If the Dose Knob is hard to push:
- -
- Pushing the Dose Knob more slowly will make it easier to inject.
- -
- Your Needle may be blocked. Put on a new Needle and prime the Pen.
- -
- You may have dust, food, or liquid inside the Pen. Throw the Pen away and get a new Pen.
If you have any questions or problems with your BASAGLAR KwikPen, contact Lilly at 1-800-LillyRx (1-800- 545-5979) or call your healthcare provider for help. For more information on BASAGLAR KwikPen and insulin, go to www.basaglar.com.
Scan this code to launch www.basaglar.com
This Instructions for Use have been approved by the U.S. Food and Drug Administration. BASAGLAR® and BASAGLAR® KwikPen® are trademarks of Eli Lilly and Company.
Instructions for Use revised: November 2022
Manufactured by:
Eli Lilly and Company
Indianapolis, IN 46285, USA
US License Number 1891
Copyright © 2015, 2022, Eli Lilly and Company. All rights reserved.
| BASAGLAR KwikPen meets the current dose accuracy and functional requirements of ISO 11608-1. |
BASKP-0009-IFU-20221115
BASAGLAR TEMPO PEN INSTRUCTIONS FOR USE
Instructions for Use
BASAGLAR® Tempo Pen™ (insulin glargine) injection, for subcutaneous use
100 units/mL, 3 mL pen, single-patient-use
Read the Instructions for Use before you start using BASAGLAR and each time you get another BASAGLAR Tempo Pen. There may be new information. This information does not take the place of talking to your healthcare provider about your medical condition or your treatment.
Do not share your BASAGLAR Tempo Pen with other people, even if the needle has been changed. You may give other people a serious infection or get a serious infection from them.
BASAGLAR Tempo Pen (“Pen”) is a disposable single-patient-use prefilled pen containing 300 units (3mL) of BASAGLAR. One pen contains multiple doses of medicine.
- Your healthcare provider will tell you how many units to give as your dose and how to inject your prescribed dose of medicine.
- You can give a dose of 1 to 80 units in a single injection.
- If your prescribed dose is more than 80 units, you will need to give yourself more than 1 injection.
- The Plunger only moves a little with each injection, and you may not notice that it moves. When the Plunger reaches the end of the cartridge, you have used all 300 units in the Pen.
People who are blind or have vision problems should not use the Pen without help from a person trained to use the BASAGLAR prefilled pen.
This BASAGLAR Tempo Pen contains a component that allows for data connectivity when used with a compatible transmitter.
How to recognize your BASAGLAR Tempo Pen
- Pen color: Light grey
- Dose Knob: Light grey
- Labels: Light grey with green color bars
Supplies needed to give your injection
- BASAGLAR Tempo Pen
- Tempo Pen compatible Needle (Becton, Dickinson and Company Pen Needles recommended)
- Alcohol swab
Preparing your Pen
- Wash your hands with soap and water.
- Check the Pen to make sure you are taking the right type of insulin. This is especially important if you use more than 1 type of insulin.
- Do not use your Pen past the expiration date printed on the Label or for more than 28 days after you first start using the Pen.
- Always use a new needle for each injection to help prevent infections and blocked needles. Do not reuse or share your needles with other people. You may give other people a serious infection or get a serious infection from them.
Priming your Pen
Prime before each injection.
- Priming means removing the air from the Needle and Cartridge that may collect during normal use. It is important to prime your Pen before each injection so that it will work correctly.
- If you do not prime before each injection, you may get too much or too little insulin.
Selecting your dose
- You can give a dose of 1 to 80 units in a single injection.
- If your dose is more than 80 units, you will need to give more than 1 injection.
- -
- Talk to your healthcare provider about how to give your dose.
- -
- Use a new Needle for each injection and repeat the priming step.
- The Pen will not let you dial more than the number of units left in the Pen.
- If you need to inject more than the number of units left in the Pen, you may either:
- -
- inject the amount left in your Pen and then use a new Pen to give the rest of your dose, or
- -
- get a new Pen and inject the full dose.
- It is normal to see a small amount of insulin left in the Pen that you cannot inject.
Giving your injection
- Inject your insulin as your healthcare provider has shown you.
- Change (rotate) your injection sites within the area you choose for each dose to reduce your risk of getting lipodystrophy (pits in skin or thickened skin) and localized cutaneous amyloidosis (skin with lumps) at the injection sites. Do not inject where skin has pits, is thickened, or has lumps. Do not inject where the skin is tender, bruised, scaly or hard, or into scars or damaged skin.
- Do not try to change your dose while injecting.
After your injection
Disposing of Pens and Needles
- Put your used needles in a FDA-cleared sharps disposal container right away after use. Do not throw away (dispose of) loose needles in your household trash.
- If you do not have a FDA-cleared sharps disposal container, you may use a household container that is:
- -
- made of a heavy-duty plastic,
- -
- can be closed with a tight-fitting, puncture-resistant lid, without sharps being able to come out,
- -
- upright and stable during use,
- -
- leak-resistant, and
- -
- properly labeled to warn of hazardous waste inside the container.
- When your sharps disposal container is almost full, you will need to follow your community guidelines for the right way to dispose of your sharps disposal container. There may be state or local laws about how you should throw away used needles and syringes. For more information about safe sharps disposal, and for specific information about sharps disposal in the state that you live in, go to the FDA's website at: http://www.fda.gov/safesharpsdisposal
- Do not dispose of your used sharps disposal container in your household trash unless your community guidelines permit this. Do not recycle your used sharps disposal container.
- The used Pen may be thrown away (discarded) in your household trash after you have removed the needle.
Storing your BASAGLAR Tempo Pen
Unopened Pens
- Store unopened Pens in the refrigerator at 36°F to 46°F (2°C to 8°C).
- Do not freeze BASAGLAR. Do not use if it has been frozen.
- Unopened Pens may be used until the expiration date printed on the Label, if the Pen has been kept in the refrigerator.
In-use Pen
- Store the Pen you are currently using at room temperature [up to 86°F (30°C)] and away from heat and light.
- Throw away the Pen you are using after 28 days, even if it still has insulin left in it.
General information about the safe and effective use of your Pen
- Keep your Pen and needles out of the sight and reach of children.
- Always use a new needle for each injection.
- Do not share your Pen or needles with other people. You may give other people a serious infection or get a serious infection from them.
- Do not use your Pen if any part looks broken or damaged.
- Always carry an extra Pen in case yours is lost or damaged.
Troubleshooting
- If you cannot remove the Pen Cap, gently twist the cap back and forth, and then pull the cap straight off.
- If the Dose Knob is hard to push:
- -
- Pushing the Dose Knob more slowly will make it easier to inject.
- -
- Your Needle may be blocked. Put on a new Needle and prime the Pen.
- -
- You may have dust, food, or liquid inside the Pen. Throw the Pen away and get a new Pen.
If you have any questions or problems with your BASAGLAR Tempo Pen, contact Lilly at 1-800-LillyRx (1-800-545-5979) or call your healthcare provider for help. For more information on BASAGLAR Tempo Pen and insulin, go to www.basaglar.com.
Scan this code to launch
www.basaglar.com
This Instructions for Use have been approved by the U.S. Food and Drug Administration.
BASAGLAR® is a registered trademark and Tempo PenTM is a trademark of Eli Lilly and Company.
Instructions for Use revised: November 2022
Manufactured by:
Eli Lilly and Company
Indianapolis, IN 46285, USA
US License Number 1891
Copyright © 2021, 2022, Eli Lilly and Company. All rights reserved.
| BASAGLAR Tempo Pen meets the current dose accuracy and functional requirements of ISO 11608-1. |
BASTP-0004-IFU-20221115
PACKAGE CARTON – BASAGLAR KwikPen 80 UNIT PEN
Dispense in this sealed carton.
NDC 0002-7715-59
Basaglar®
KwikPen®
(insulin glargine)
injection
For Single Patient Use Only
100 units per mL (U-100)
For subcutaneous use only
Can inject from 1 to 80 units in a single injection
5 x 3 mL prefilled pens
prefilled insulin delivery device
Rx only
Read Basaglar® KwikPen® Instructions for Use.
NEEDLES NOT INCLUDED
This device is recommended for use with Becton, Dickinson & Company's insulin pen needles.
Lilly
PACKAGE CARTON – BASAGLAR Tempo Pen 80 UNIT PEN
Dispense in this sealed carton.
NDC 0002-8214-05
Basaglar®
Tempo Pen™
(insulin glargine)
injection
For Single Patient Use Only
100 units per mL (U-100)
For subcutaneous use only
Can inject from 1 to 80 units in a single injection
5 x 3 mL prefilled pens
prefilled insulin delivery device
Rx only
Read Basaglar® Tempo Pen™ Instructions for Use.
NEEDLES NOT INCLUDED
This device is recommended for use with Becton, Dickinson & Company's insulin pen needles.
Lilly
| BASAGLAR
KWIKPEN
insulin glargine injection, solution |
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
|
||||||||||||||||||||||||||||||
| BASAGLAR
TEMPO PEN
insulin glargine injection, solution |
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
|
||||||||||||||||||||
| Labeler - Eli Lilly and Company (006421325) |
Biological Products Related to Basaglar
Find detailed information on biosimilars for this medication.
Frequently asked questions
- Basaglar and Lantus - What is the difference between them?
- How and where should I inject insulin?
- When is the best time to take Toujeo?
- How long can Toujeo stay out of the refrigerator?
- What are the different types of insulin?
- Soliqua vs Lantus: What’s the difference between them?
- Can Toujeo be given twice a day?
- How many pens are in a box of Toujeo?
- Is Toujeo a fast or long-acting insulin?
More about Basaglar (insulin glargine)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (149)
- Latest FDA alerts (3)
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: insulin
- En español
Patient resources
Professional resources
Other brands
Lantus, Toujeo SoloStar, Semglee, Rezvoglar
Related treatment guides
Copyright © 2015, 2021, Eli Lilly and Company. All rights reserved.

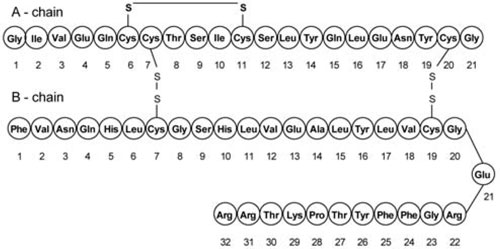

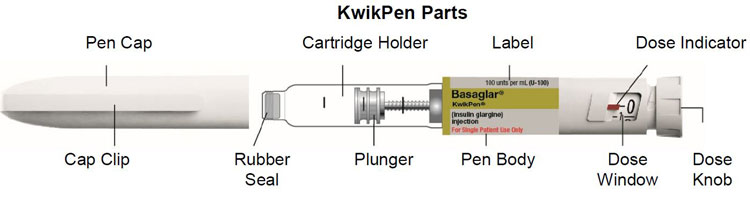
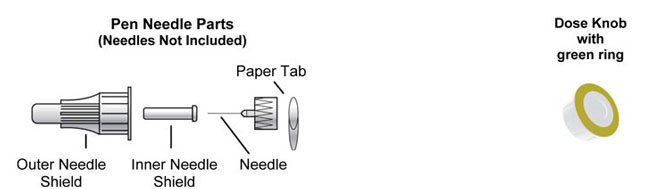
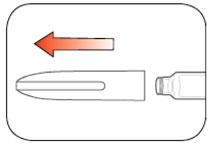

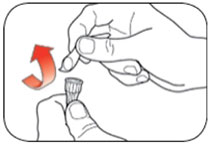
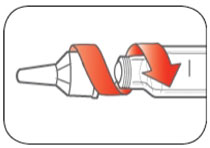
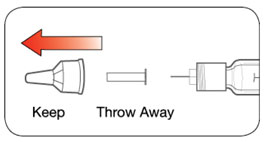
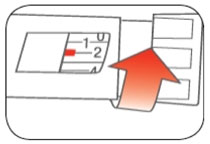
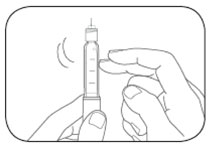
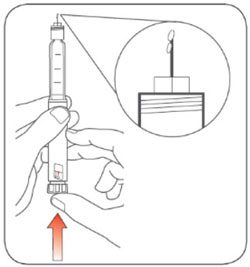
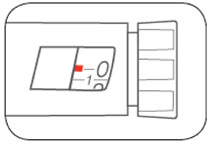
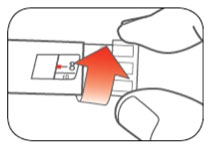
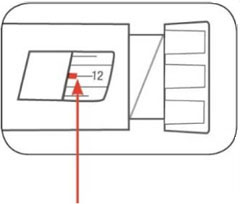
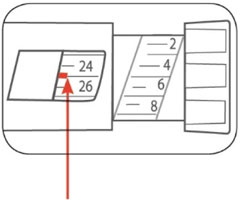 (Example: 25 units shown in the Dose Window)
(Example: 25 units shown in the Dose Window)
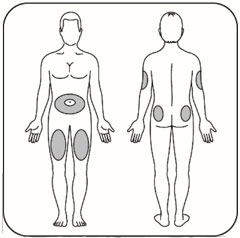

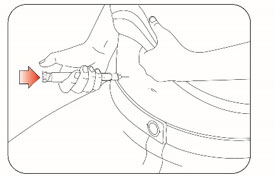
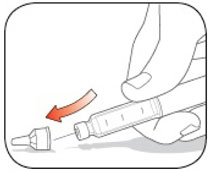
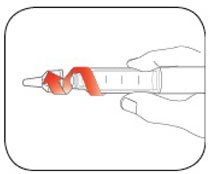
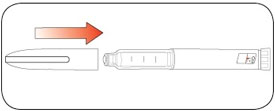


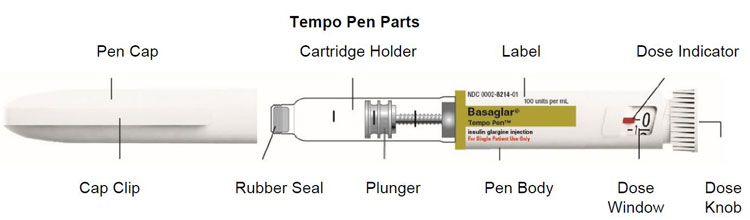


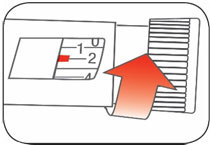
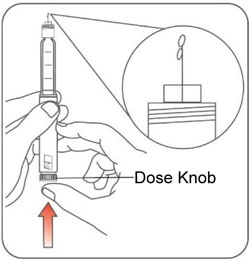
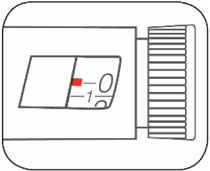
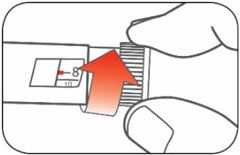
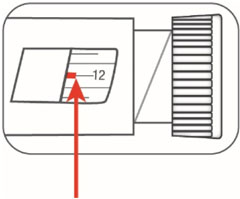 (Example: 12 units shown in the Dose Window)
(Example: 12 units shown in the Dose Window)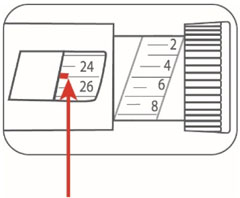 (Example: 25 units shown in the Dose Window)
(Example: 25 units shown in the Dose Window)