Valsartan (Monograph)
Brand names: Diovan, Exforge (combination), Exforge HCT (combination)
Drug class: Angiotensin II Receptor Antagonists
VA class: CV805
Chemical name: N-(1-Oxopentyl)-N-[[2′-(1H-tetrazol-5-yl) [1,1′-biphenyl]-4-yl]methyl)]-l-valine
Molecular formula: C24H29N5O3
CAS number: 137862-53-4
Warning
-
May cause fetal and neonatal morbidity and mortality if used during pregnancy. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
-
If pregnancy is detected, discontinue as soon as possible.
Introduction
Valsartan is an angiotensin II type 1 (AT1) receptor antagonist (i.e., angiotensin II receptor blocker, ARB).
Uses for Valsartan
Hypertension
Management of hypertension (alone or in combination with other classes of antihypertensive agents); may be used in fixed combination with amlodipine and/or hydrochlorothiazide when such combined therapy is indicated.
Angiotensin II receptor antagonists are recommended as one of several preferred agents for the initial management of hypertension according to current evidence-based hypertension guidelines; other preferred options include ACE inhibitors, calcium-channel blockers, and thiazide diuretics. While there may be individual differences with respect to recommendations for initial drug selection and use in specific patient populations, current evidence indicates that these antihypertensive drug classes all generally produce comparable effects on overall mortality and cardiovascular, cerebrovascular, and renal outcomes.
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension. (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP. However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk. In addition, an SBP goal of <130 mm Hg is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg. These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.
Previous hypertension guidelines generally have based target BP goals on age and comorbidities. Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk and have used higher BP thresholds and target BPs in elderly patients compared with those recommended by the 2017 ACC/AHA hypertension guideline.
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the current ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient’s BP treatment goal.
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors. ASCVD risk assessment recommended by ACC/AHA for all adults with hypertension.
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.
Adults with hypertension and diabetes mellitus, chronic kidney disease (CKD), or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP. Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.
Black hypertensive patients generally tend to respond better to monotherapy with calcium-channel blockers or thiazide diuretics than to angiotensin II receptor antagonists. However, the combination of an ACE inhibitor or an angiotensin II receptor antagonist with a calcium-channel blocker or thiazide diuretic produces similar BP lowering in black patients as in other racial groups.
Angiotensin II receptor antagonists or ACE inhibitors may be particularly useful in hypertensive patients with diabetes mellitus or CKD; angiotensin II receptor antagonists also may be preferred, as an alternative to ACE inhibitors, in hypertensive patients with heart failure or ischemic heart disease and/or post-MI.
Heart Failure
Used in the management of heart failure.
Because of their established benefits, ACE inhibitors have been the preferred drugs for inhibition of the renin-angiotensin-aldosterone (RAA) system in patients with heart failure and reduced left ventricular ejection fraction (LVEF); however, some evidence indicates that therapy with an ACE inhibitor (enalapril) may be less effective than angiotensin receptor-neprilysin inhibitor (ARNI) therapy (e.g., sacubitril/valsartan) in reducing cardiovascular death and heart failure-related hospitalization.
Angiotensin II receptor antagonists may be used as an alternative for those patients in whom use of an ACE inhibitor or ARNI is inappropriate.
No additional therapeutic benefit when angiotensin II receptor antagonist used in combination with an ACE inhibitor.
ACCF, AHA, and the Heart Failure Society of America (HFSA) recommend that patients with chronic symptomatic heart failure and reduced LVEF (NYHA class II or III) who are able to tolerate an ACE inhibitor or angiotensin II receptor antagonist be switched to therapy containing an ARNI to further reduce morbidity and mortality.
Heart Failure or Left Ventricular Dysfunction After Acute MI
Valsartan is used to reduce the risk of cardiovascular mortality in clinically stable patients who have demonstrated clinical signs of heart failure or left ventricular dysfunction following MI.
While ACE inhibitors generally are the preferred agents for this use because of their established benefits, angiotensin II receptor antagonists may be substituted in patients who are intolerant to ACE inhibitor therapy.
Diabetic Nephropathy
A recommended agent in the management of patients with diabetes mellitus and persistent albuminuria† [off-label] who have modestly elevated (30–300 mg/24 hours) or higher (>300 mg/24 hours) levels of urinary albumin excretion; slows rate of progression of renal disease in such patients.
Valsartan Dosage and Administration
General
BP Monitoring and Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug until BP controlled.
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., calcium-channel blocker, thiazide diuretic). Many patients will require at least 2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.
Administration
Oral Administration
Administer valsartan orally once or twice daily without regard to meals.
Administer valsartan as extemporaneously prepared oral suspension in pediatric patients unable to swallow tablets or in those for whom the calculated daily dosage does not correspond to the available tablet strengths.
Reconstitution
Preparation of extemporaneous suspension containing valsartan 4 mg/mL: Add 80 mL of suspending vehicle (e.g., Ora-Plus) to an amber glass bottle containing 8 valsartan 80-mg tablets; shake the contents for ≥2 minutes. Allow concentrated suspension to stand for ≥1 hour, then shake for ≥1 additional minute. Dilute the concentrated suspension with 80 mL of sweetening vehicle (e.g., Ora-Sweet SF); shake the contents for ≥10 seconds. Shake suspension for ≥10 seconds before dispensing each dose.
Dosage
Pediatric Patients
Hypertension
Oral
Children 6–16 years of age: Initially, valsartan 1.3 mg/kg (up to 40 mg) once daily. Adjust dosage according to patient response; some experts state dosage may be increased every 2–4 weeks until BP controlled, maximum dosage reached, or adverse effects occur. Dosages >2.7 mg/kg (up to 160 mg) once daily have not been studied in children.
May need to increase dosage when converting from extemporaneously prepared suspension to oral tablet, since exposure to valsartan with the suspension is 1.6 times greater than with the tablet.
Adults
Hypertension
Valsartan Therapy
OralManufacturers recommend initial dosage of 80 or 160 mg once daily as monotherapy in adults without intravascular volume depletion.
Usual dosage is 80–320 mg once daily. However, at dosages >80 mg daily, addition of diuretic produces greater BP reduction than increases in valsartan dosage.
Valsartan/Amlodipine Fixed-combination Therapy
OralFixed-combination preparation may be used for initial treatment of hypertension in patients likely to require combination therapy with multiple antihypertensive agents to control BP. Consider potential benefits and risks of initiating therapy with the fixed combination, including whether the patient is likely to tolerate the lowest available dosage of the combined drugs.
If the patient’s baseline BP is 160/100 mm Hg, the estimated probability of achieving SBP control (SBP <140 mm Hg) is 47, 67, or 80% and of achieving DBP control (DBP <90 mm Hg) is 62, 80, or 85% with valsartan (320 mg daily) alone, amlodipine (10 mg daily) alone, or valsartan combined with amlodipine (same dosages), respectively.
In studies using valsartan/amlodipine fixed combination in dosages of valsartan 160–320 mg daily and amlodipine 5–10 mg daily, BP response increased with increasing dosages of the drugs.
If BP is not adequately controlled by monotherapy with valsartan (or another angiotensin II receptor antagonist) or amlodipine (or another dihydropyridine-derivative calcium-channel blocker), can switch to valsartan/amlodipine fixed combination.
If dose-limiting adverse effects have developed during monotherapy with valsartan or amlodipine, can switch to a fixed combination containing a lower dose of that drug to achieve similar BP control; adjust dosage according to patient’s response after 3–4 weeks of therapy.
If BP is controlled with valsartan and amlodipine (administered separately), can switch to the fixed-combination preparation containing the corresponding individual doses for convenience.
When used for initial therapy of hypertension in patients likely to require combination therapy with multiple antihypertensive agents, recommended initial dosage is valsartan 160 mg and amlodipine 5 mg once daily in those who are not volume depleted.
Increase to maximum dosage of valsartan 320 mg and amlodipine 10 mg once daily, if needed, to control BP. May adjust dosage at intervals of 1–2 weeks, since most of the antihypertensive effect of a given dosage is achieved within 2 weeks after a change in dosage.
Valsartan/Hydrochlorothiazide Fixed-combination Therapy
OralFixed-combination preparation may be used for initial treatment of hypertension in patients likely to require combination therapy with multiple antihypertensive agents to control BP. Consider potential benefits and risks of initiating therapy with the fixed combination. Not recommended as initial therapy in patients who are volume depleted.
If the patient’s baseline BP is 160/100 mm Hg, the estimated probability of achieving SBP control (SBP <140 mm Hg) is 41, 50, or 84% and of achieving DBP control (DBP <90 mm Hg) is 60, 57, or 80% with valsartan (320 mg daily) alone, hydrochlorothiazide (25 mg daily) alone, or valsartan combined with hydrochlorothiazide (same dosages), respectively.
If BP is not adequately controlled by monotherapy with valsartan (or another angiotensin II receptor antagonist) or hydrochlorothiazide, can switch to fixed-combination tablets containing valsartan 160 mg and hydrochlorothiazide 12.5 mg once daily.
If dose-limiting adverse effects have developed during monotherapy with valsartan or hydrochlorothiazide, can switch to a fixed combination containing a lower dose of that drug to achieve similar BP control; adjust dosage according to patient’s response after 3–4 weeks of therapy.
If BP is controlled with valsartan and hydrochlorothiazide (administered separately), can switch to the fixed-combination preparation containing the corresponding individual doses for convenience.
When used for initial therapy of hypertension in patients likely to require combination therapy with multiple antihypertensive agents, recommended initial dosage is valsartan 160 mg and hydrochlorothiazide 12.5 mg daily in those who are not volume depleted. Adjust dosage according to patient’s response after 1–2 weeks of therapy.
Increase to maximum dosage of valsartan 320 mg and hydrochlorothiazide 25 mg daily, if needed, to control BP. Maximum antihypertensive effect of a given dosage is achieved within 2–4 weeks after a change in dosage.
Valsartan/Amlodipine/Hydrochlorothiazide Fixed-combination Therapy
OralManufacturers state fixed-combination preparation should not be used for initial treatment of hypertension.
Can switch to fixed-combination valsartan/amlodipine/hydrochlorothiazide tablets if BP is not adequately controlled by combined therapy with any 2 of the following drug classes: angiotensin II receptor antagonists, calcium-channel blockers, or diuretics.
In patients who experience dose-limiting adverse effects of valsartan, amlodipine, or hydrochlorothiazide while receiving any dual combination of these drugs, may switch to the triple fixed-combination preparation containing a lower dose of that component.
Can use the fixed combination as a substitute for the individually titrated drugs.
May increase dosage of the fixed combination after 2 weeks if additional BP control is needed (up to maximum of valsartan 320 mg, amlodipine 10 mg, and hydrochlorothiazide 25 mg once daily).
Heart Failure
Oral
Initially, valsartan 40 mg twice daily recommended by manufacturer; some experts recommend initial dosage of 20–40 mg twice daily. Increase dosage to 160 mg twice daily (maximum dosage used in clinical trials) or highest tolerated dosage. (See Hypotension under Cautions.)
Heart Failure or Left Ventricular Dysfunction After Acute MI
Oral
Manufacturers state that valsartan therapy may be initiated ≥12 hours post-MI with a dosage of 20 mg twice daily. May increase dosage to 40 mg twice daily within 7 days, with subsequent titration to a target maintenance dosage of 160 mg twice daily, as tolerated.
Consider dosage reduction if symptomatic hypotension or renal dysfunction occurs.
Special Populations
The following information addresses dosage of valsartan in special populations. Dosages of drugs administered in fixed combination with valsartan also may require adjustment in certain patient populations; the need for such dosage adjustments must be considered in the context of cautions, precautions, and contraindications specific to that population and drug.
Hepatic Impairment
No adjustment of initial valsartan dosage necessary in patients with mild to moderate hepatic impairment. Cautious dosing recommended in patients with hepatic impairment.
Amount of amlodipine in valsartan/amlodipine fixed combinations exceeds the recommended initial dosage of amlodipine (2.5 mg daily) in patients with hepatic impairment.
Renal Impairment
No adjustment of initial valsartan dosage necessary in patients with mild to moderate renal impairment. Cautious dosing recommended in adults with severe impairment. Use of valsartan in pediatric patients with GFR <30 mL/minute per 1.73 m2 not studied.
Safety and efficacy of valsartan/hydrochlorothiazide fixed combination not established in patients with severe impairment (Clcr ≤30 mL/minute).
Geriatric Patients
No adjustment of initial valsartan dosage is necessary.
Amount of amlodipine in valsartan/amlodipine fixed combinations exceeds the recommended initial dosage of amlodipine (2.5 mg daily) in patients ≥75 years of age.
Volume- and/or Salt-Depleted Patients
Correct volume and/or salt depletion prior to initiation of valsartan therapy or initiate therapy under close medical supervision.
Cautions for Valsartan
Contraindications
-
Known hypersensitivity to valsartan or any ingredient in the formulation.
-
Concomitant use of aliskiren and valsartan in patients with diabetes mellitus. (See Specific Drugs under Interactions.)
-
When valsartan is used in fixed combination with hydrochlorothiazide or amlodipine, consider contraindications associated with the concomitant agent.
Warnings/Precautions
Warnings
Fetal/Neonatal Morbidity and Mortality
Possible fetal and neonatal morbidity and mortality when drugs that act directly on the renin-angiotensin system (e.g., angiotensin II receptor antagonists, ACE inhibitors) are used during the second and third trimesters of pregnancy. (See Boxed Warning.) ACE inhibitors also may increase the risk of major congenital malformations when administered during the first trimester of pregnancy.
Discontinue valsartan as soon as possible when pregnancy is detected, unless continued use is considered lifesaving. Nearly all women can be transferred successfully to alternative therapy for the remainder of their pregnancy.
Sensitivity Reactions
Anaphylactoid reactions and/or angioedema possible with angiotensin II receptor antagonists; extreme caution in patients with a history of angioedema associated with or unrelated to ACE inhibitor or angiotensin II receptor antagonist therapy.
Other Warnings and Precautions
Hypotension
Possible symptomatic hypotension with valsartan, particularly in volume- and/or salt-depleted patients (e.g., those treated with diuretics). (See Volume- and/or Salt-Depleted Patients under Dosage and Administration.)
Transient hypotension is not a contraindication to additional doses; may reinstate valsartan therapy cautiously after BP is stabilized (e.g., with volume expansion).
Initiate valsartan therapy and subsequent dosage adjustments under close medical supervision in patients with heart failure; consider reducing diuretic dosage.
Malignancies
In July 2010, FDA initiated a safety review of angiotensin II receptor antagonists after a published meta-analysis found a modest but statistically significant increase in risk of new cancer occurrence in patients receiving an angiotensin II receptor antagonist compared with control. However, subsequent studies, including a larger meta-analysis conducted by FDA, have not shown such risk. Based on currently available data, FDA has concluded that angiotensin II receptor antagonists do not increase the risk of cancer.
Renal Effects
Possible acute renal failure in patients with severe heart failure, renal artery stenosis, CKD, or volume depletion.
Hyperkalemia
Hyperkalemia may occur, especially in patients with heart failure and preexisting renal impairment.
Use of Fixed Combinations
When valsartan is used in fixed combination with amlodipine and/or hydrochlorothiazide, consider the cautions, precautions, contraindications, and interactions associated with the concomitant agent(s). Consider cautionary information applicable to specific populations (e.g., pregnant or nursing women, individuals with hepatic or renal impairment, geriatric patients) for each drug in the fixed combination.
Specific Populations
Pregnancy
Category D.
Can cause fetal and neonatal morbidity and death when administered to a pregnant woman. (See Boxed Warning.)
Lactation
Valsartan is distributed into milk in rats; not known whether valsartan is distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy of valsartan in pediatric patients 6–16 years of age with hypertension established in a controlled clinical trial. Some evidence of efficacy in controlled clinical trials in pediatric patients 6 months to 5 years of age; however, 2 deaths and 3 cases of transaminase elevations were observed in an open-label extension study in patients 1–5 years of age. Although causal relationship to valsartan has not been established, use is not recommended in pediatric patients <6 years of age.
Safety and efficacy of valsartan not established in children with GFR <30 mL/minute per 1.73 m2.
Safety and efficacy of valsartan in fixed combination with amlodipine and/or hydrochlorothiazide not established in children.
Geriatric Use
No substantial differences in safety or efficacy relative to younger adults, but increased sensitivity to valsartan alone or in fixed combination with amlodipine and/or hydrochlorothiazide cannot be ruled out.
Hepatic Impairment
Systemic exposure to valsartan may be increased (see Absorption: Special Populations, under Pharmacokinetics). Use with caution.
Renal Impairment
Valsartan not studied in patients with Clcr <10 mL/minute; use with caution in adults with severe renal impairment. Valsartan not studied in children with GFR <30 mL/minute per 1.73 m2.
Deterioration of renal function may occur. (See Renal Effects under Cautions.)
Valsartan in fixed combination with hydrochlorothiazide not studied in patients with Clcr ≤30 mL/minute.
Black Patients
BP reduction with angiotensin II receptor antagonists may be smaller in black patients than in patients of other races. (See Hypertension under Uses.)
Common Adverse Effects
Viral infection, fatigue, abdominal pain; also, dizziness, hypotension, postural dizziness or hypotension, hyperkalemia, arthralgia, diarrhea, and back pain in patients with heart failure.
Drug Interactions
When valsartan is used in fixed combination with hydrochlorothiazide and/or amlodipine, also consider interactions associated with the concomitant agent.
Valsartan is minimally metabolized by CYP2C9 and does not inhibit CYP enzymes at therapeutic concentrations.
In vitro data suggest that valsartan is a substrate of organic anion transporter protein (OATP) 1B1 (hepatic uptake transporter) and multidrug resistance protein MRP2 (hepatic efflux transporter).
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Drug interactions mediated by CYP enzymes unlikely.
Drugs That Inhibit Hepatic Transport Systems
Inhibitors of OATP 1B1 or MRP2: Possible increased systemic exposure to valsartan.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantly |
|
Aliskiren |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantly Concomitant use contraindicated in patients with diabetes mellitus Avoid concomitant use in patients with GFR <60 mL/minute |
|
Amlodipine |
Pharmacokinetic interaction unlikely |
|
|
Angiotensin II receptor antagonists |
Increased risk of renal impairment, hyperkalemia, and hypotension |
Generally avoid concomitant use; monitor BP, renal function, and electrolytes if used concomitantly |
|
Atenolol |
Pharmacokinetic interaction unlikely Additive antihypertensive effect; heart rate unaffected |
|
|
Cimetidine |
Pharmacokinetic interaction unlikely |
|
|
Cyclosporine |
Possible increased systemic exposure to valsartan |
|
|
Digoxin |
Pharmacokinetic interactions unlikely |
|
|
Diuretics, potassium-sparing (e.g., amiloride, spironolactone, triamterene) |
Possible additive hyperkalemic effects; possible increase in Scr in patients with heart failure |
Monitor serum potassium concentrations |
|
Furosemide |
Pharmacokinetic interactions unlikely |
|
|
Glyburide |
Pharmacokinetic interactions unlikely |
|
|
Heparin |
Possible additive hyperkalemic effect; possible increase in Scr in patients with heart failure |
Monitor serum potassium concentrations |
|
Hydrochlorothiazide |
Pharmacokinetic interactions unlikely Additive hypotensive effects |
|
|
Indomethacin |
Pharmacokinetic interactions unlikely |
|
|
Lithium |
Increased serum lithium concentrations; possible toxicity |
Monitor serum lithium concentrations |
|
NSAIAs, including selective cyclooxygenase-2 (COX-2) inhibitors |
Possible deterioration of renal function in geriatric, volume-depleted, or renally impaired patients Possible reduced antihypertensive effects |
Monitor renal function periodically |
|
Potassium supplements and potassium-containing salt substitutes |
Possible additive hyperkalemic effect; possible increase in Scr in patients with heart failure |
Monitor serum potassium concentrations |
|
Rifampin |
Possible increased systemic exposure to valsartan |
|
|
Ritonavir |
Possible increased systemic exposure to valsartan |
|
|
Warfarin |
Pharmacokinetic interactions unlikely; INR unaffected |
Valsartan Pharmacokinetics
Absorption
Bioavailability
Absolute bioavailability of valsartan tablets is about 25% (range: 10–35%). Bioavailability of extemporaneously prepared suspension (see Reconstitution under Dosage and Administration) is 1.6 times greater than that of the tablets.
Peak plasma concentration of valsartan reached about 2–4 hours following oral administration.
Onset
Antihypertensive effect of valsartan evident within 2 weeks, with maximum BP reduction after 4 weeks.
Food
Food may decrease rate and extent (e.g., AUC decreased by about 40%) of absorption of valsartan.
Special Populations
In patients with mild to moderate chronic liver disease, systemic exposure to valsartan is doubled.
Distribution
Extent
Valsartan crosses the placenta and is distributed in the fetus in animals.
Valsartan is distributed into milk in rats; not known whether valsartan is distributed into human milk.
Plasma Protein Binding
Valsartan: 95% (mainly albumin).
Elimination
Metabolism
Minimally metabolized in the liver by CYP2C9.
Elimination Route
Valsartan is eliminated mainly as unchanged drug in feces (83%) and urine (13%).
Half-life
Biexponential; average half-life of valsartan is approximately 6 hours following IV administration.
Valsartan clearance is similar in adults and children.
Special Populations
Valsartan is not removed by hemodialysis.
Stability
Storage
Oral
Extemporaneous Suspension
Valsartan 4 mg/mL in Ora-Sweet SE and Ora-Plus (see Reconstitution under Dosage and Administration), stored in amber glass bottle with child-resistant screw-cap closure: Up to 30 days at <30ºC or up to 75 days at 2–8ºC.
Tablets
Valsartan, valsartan/amlodipine, valsartan/hydrochlorothiazide, and valsartan/amlodipine/hydrochlorothiazide tablets: Tight container at 25°C (may be exposed to 15–30°C). Protect from moisture.
Actions
-
Valsartan blocks the physiologic actions of angiotensin II, including vasoconstrictor and aldosterone-secreting effects.
-
Valsartan does not interfere with response to bradykinins and substance P.
-
Valsartan does not share the ACE inhibitor common adverse effect of dry cough.
Advice to Patients
-
When valsartan is used in fixed combination with hydrochlorothiazide and/or amlodipine, importance of advising patients of important precautionary information about the concomitant agent(s).
-
Risks of use during pregnancy.
-
Importance of women informing their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs (including salt substitutes containing potassium).
-
Importance of contacting clinician if dizziness or faintness develops or if unexplained weight gain or swelling of the feet, ankles, or hands occurs.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
40 mg* |
Diovan (scored) |
Novartis |
|
Valsartan Tablets |
||||
|
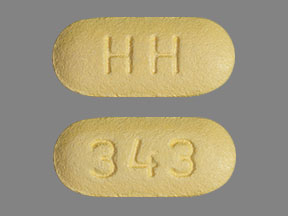
80 mg* |
Diovan |
Novartis |
||
|
Valsartan Tablets |
||||
|
160 mg* |
Diovan |
Novartis |
||
|
Valsartan Tablets |
||||
|
320 mg* |
Diovan |
Novartis |
||
|
Valsartan Tablets |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
80 mg with Hydrochlorothiazide 12.5 mg* |
Diovan HCT |
Novartis |
|
Valsartan and Hydrochlorothiazide Tablets |
||||
|
160 mg with Amlodipine Besylate 5 mg (of amlodipine)* |
Amlodipine Besylate and Valsartan Tablets |
|||
|
Exforge |
Novartis |
|||
|
160 mg with Amlodipine Besylate 5 mg (of amlodipine) and Hydrochlorothiazide 12.5 mg* |
Amlodipine Besylate, Valsartan, and Hydrochlorothiazide Tablets |
|||
|
Exforge HCT |
Novartis |
|||
|
160 mg with Amlodipine Besylate 5 mg (of amlodipine) and Hydrochlorothiazide 25 mg* |
Amlodipine Besylate, Valsartan, and Hydrochlorothiazide Tablets |
|||
|
Exforge HCT |
Novartis |
|||
|
160 mg with Amlodipine Besylate 10 mg (of amlodipine)* |
Amlodipine Besylate and Valsartan Tablets |
|||
|
Exforge |
Novartis |
|||
|
160 mg with Amlodipine Besylate 10 mg (of amlodipine) and Hydrochlorothiazide 12.5 mg* |
Amlodipine Besylate, Valsartan, and Hydrochlorothiazide Tablets |
|||
|
Exforge HCT |
Novartis |
|||
|
160 mg with Amlodipine Besylate 10 mg (of amlodipine) and Hydrochlorothiazide 25 mg* |
Amlodipine Besylate, Valsartan, and Hydrochlorothiazide Tablets |
|||
|
Exforge HCT |
Novartis |
|||
|
160 mg with Hydrochlorothiazide 12.5 mg* |
Diovan HCT |
Novartis |
||
|
Valsartan and Hydrochlorothiazide Tablets |
||||
|
160 mg with Hydrochlorothiazide 25 mg* |
Diovan HCT |
Novartis |
||
|
Valsartan and Hydrochlorothiazide Tablets |
||||
|
320 mg with Amlodipine Besylate 5 mg (of amlodipine)* |
Amlodipine Besylate and Valsartan Tablets |
|||
|
Exforge |
Novartis |
|||
|
320 mg with Amlodipine Besylate 10 mg (of amlodipine)* |
Amlodipine Besylate and Valsartan Tablets |
|||
|
Exforge |
Novartis |
|||
|
320 mg with Amlodipine Besylate 10 mg (of amlodipine) and Hydrochlorothiazide 25 mg* |
Amlodipine Besylate, Valsartan, and Hydrochlorothiazide Tablets |
|||
|
Exforge HCT |
Novartis |
|||
|
320 mg with Hydrochlorothiazide 12.5 mg* |
Diovan HCT |
Novartis |
||
|
Valsartan and Hydrochlorothiazide Tablets |
||||
|
320 mg with Hydrochlorothiazide 25 mg* |
Diovan HCT |
Novartis |
||
|
Valsartan and Hydrochlorothiazide Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions November 5, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Losartan vs Valsartan - What's the difference between them?
- What is the strength of Prexxartan (valsartan) oral solution?
More about valsartan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (152)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: angiotensin receptor blockers
- Breastfeeding
- En español