valACYclovir (Monograph)
Brand name: Valtrex
Drug class: Nucleosides and Nucleotides
Introduction
Antiviral; prodrug of acyclovir, a nucleoside.
Uses for valACYclovir
Genital Herpes
Treatment of initial episodes of genital herpes in immunocompetent or HIV-infected† [off-label] adults and adolescents.
Episodic treatment of recurrent episodes of genital herpes in immunocompetent or HIV-infected† [off-label] adults and adolescents.
Chronic suppressive therapy of recurrent episodes of genital herpes in immunocompetent or HIV-infected adults and adolescents. When used for suppressive therapy in immunocompetent individuals, the risk of heterosexual transmission of genital herpes to susceptible partners is reduced; efficacy for reducing transmission not established in those with multiple partners or in non-heterosexual couples.
CDC and others recommend oral acyclovir, oral famciclovir, or oral valacyclovir as drug of choice for treatment of initial episodes of genital herpes and for episodic treatment or chronic suppressive therapy of recurrent genital herpes.
Herpes Labialis
Treatment of herpes labialis (perioral herpes, cold sores, fever blisters) in adults and adolescents.
Safety and efficacy not established in immunocompromised patients.
Mucocutaneous Herpes Simplex Virus (HSV) Infections
Treatment of recurrent mucocutaneous HSV infections in HIV-infected adults† [off-label].
Chronic suppressive or maintenance therapy (secondary prophylaxis) against recurrence of HSV infections† [off-label] in HIV-infected individuals who have frequent or severe recurrences.
Herpes Zoster
Treatment of acute, localized herpes zoster (shingles, zoster) in adults and adolescents.
Treatment of localized dermatomal herpes zoster in HIV-infected adults or adolescents† [off-label]. If cutaneous lesions are extensive or there is clinical evidence of visceral involvement, IV acyclovir should be used for initial treatment.
Safety and efficacy not established in immunocompromised patients.
Safety and efficacy not established for treatment of disseminated herpes zoster.
Prevention of Cytomegalovirus (CMV) Disease in Transplant Recipients
Prevention of CMV disease in kidney transplant recipients† at high risk (CMV-seropositive donor).
Not recommended for prevention of CMV disease in hematopoietic stem cell transplant (HSCT) recipients because the drug is presumed to be less effective than ganciclovir.
Not recommended for primary prevention of CMV disease in HIV-infected individuals because of an unexplained trend toward increased mortality in clinical studies.
valACYclovir Dosage and Administration
Administration
Oral Administration
Administer orally without regard to meals.
Patients should maintain adequate hydration during treatment.
Extemporaneously Compounded Oral Liquid
Extemporaneously compounded oral liquid formulations of valacyclovir containing 50 mg/mL have been prepared using the commercially available caplets and commonly used syrups.
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral liquid formulation of valacyclovir have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web].
|
Concentration Standards |
|---|
|
50 mg/mL |
Dosage
Available as valacyclovir hydrochloride; dosage expressed in terms of valacyclovir.
Pediatric Patients
Genital Herpes, Herpes Labialis, Mucocutaneous Herpes Simplex Virus (HSV) Infections, and Herpes Zoster
Oral
Adolescents should receive dosage recommended for adults. (See Adults under Dosage and Administration.)
Adults
Genital Herpes
Treatment of First Episodes
OralImmunocompetent adults: 1 g twice daily for 7–10 days. CDC suggests duration of treatment may be extended if healing is incomplete after 10 days.
HIV-infected adults: 1 g twice daily for 7–14 days recommended by CDC and others.
Initiate therapy within 48 hours of onset of signs and symptoms; efficacy not established if initiated >72 hours after onset of signs or symptoms.
Episodic Treatment of Recurrent Episodes
OralImmunocompetent adults: 500 mg twice daily for 3 days. Alternatively, CDC recommends 1 g once daily for 5 days†.
HIV-infected adults: CDC recommends 1 g twice daily for 5–10 days; may be continued for 7–14 days.
Initiate therapy at first sign or symptom of an episode; efficacy not established if initiated >24 hours after onset of signs or symptoms.
Suppressive Therapy of Recurrent Episodes
OralImmunocompetent adults: 1 g once daily. Alternatively, 500 mg once daily for those with a history of ≤9 recurrences per year.
HIV-infected adults: 500 mg twice daily.
Manufacturer states safety and efficacy not established beyond a duration of 1 year in immunocompetent or 6 months in HIV-infected individuals.
Because frequency of recurrent episodes diminishes over time in many patients, CDC and others recommend suppressive antiviral therapy be discontinued periodically (e.g., once yearly) to assess the need for continued therapy.
Reduction of Transmission
Oral500 mg once daily in source partner with a history of ≤9 recurrences per year.
Efficacy for reducing transmission not established beyond a duration of 8 months in discordant couples.
Herpes Labialis
Oral
Immunocompetent adults: 2 g every 12 hours for 1 day; treatment for cold sores should not exceed 1 day.
Initiate treatment at earliest symptom of cold sore (e.g., tingling, itching, burning); efficacy not established if initiated after development of clinical signs of cold sore (e.g., papule, vesicle, ulcer).
Mucocutaneous Herpes Simplex Virus (HSV) Infections
Chronic Suppression of Recurrent Episodes
OralHIV-infected adults: 500 mg twice daily for chronic suppressive or maintenance therapy (secondary prophylaxis) of HSV infections in those who have frequent or severe recurrences.
Herpes Zoster
Oral
Immunocompetent adults: 1 g 3 times daily for 7 days.
Local dermatomal herpes zoster in HIV-infected adults or adolescents†: 1 g 3 times daily for 7–10 days recommended by CDC and others.
Initiate therapy at earliest sign or symptom (preferably within 48 hours of rash onset); efficacy not established if initiated >72 hours after rash onset.
Special Populations
Hepatic Impairment
Dosage adjustments not recommended for patients with cirrhosis.
Renal Impairment
Genital Herpes
Oral
|
Clcr (mL/min) |
Daily Dosage |
|---|---|
|
First Episodes |
|
|
≥50 |
1 g every 12 hours |
|
30–49 |
1 g every 12 hours |
|
10–29 |
1 g once every 24 hours |
|
<10 |
500 mg once every 24 hours |
|
Episodic Treatment of Recurrent Episodes |
|
|
≥50 |
500 mg every 12 hours |
|
30–49 |
500 mg every 12 hours |
|
10–29 |
500 mg once every 24 hours |
|
<10 |
500 mg once every 24 hours |
|
Suppressive Therapy of Recurrent Episodes (Immunocompetent with >9 Episodes/Year) |
|
|
≥50 |
1 g once every 24 hours |
|
30–49 |
1 g once every 24 hours |
|
10–29 |
500 mg once every 24 hours |
|
<10 |
500 mg once every 24 hours |
|
Suppressive Therapy of Recurrent Episodes (Immunocompetent with <9 Episodes/Year) |
|
|
≥50 |
500 mg once every 24 hours |
|
30–49 |
500 mg once every 24 hours |
|
10–29 |
500 mg once every 48 hours |
|
<10 |
500 mg once every 48 hours |
|
Suppressive Therapy of Recurrent Episodes (HIV-infected Individuals) |
|
|
≥50 |
500 mg every 12 hours |
|
30–49 |
500 mg every 12 hours |
|
10–29 |
500 mg once every 24 hours |
|
<10 |
500 mg once every 24 hours |
Herpes Labialis
Oral
|
Clcr (mL/min) |
Daily Dosage |
|---|---|
|
≥50 |
2 g every 12 hours for 1 day |
|
30–49 |
1 g every 12 hours for 1 day |
|
10–29 |
500 mg every 12 hours for 1 day |
|
<10 |
A single dose of 500 mg |
Herpes Zoster
Oral
|
Clcr (mL/min) |
Daily Dosage |
|---|---|
|
≥50 |
1 g every 8 hours |
|
30–49 |
1 g every 12 hours |
|
10–29 |
1 g once every 24 hours |
|
<10 |
500 mg once every 24 hours |
Hemodialysis
Usual dose should be administered after hemodialysis.
Peritoneal Dialysis
Supplemental doses unnecessary following CAPD or CAVHD.
Geriatric Patients
No dosage adjustments except those related to renal impairment.
Cautions for valACYclovir
Contraindications
-
Known hypersensitivity or intolerance to valacyclovir, acyclovir, or any component of the formulation.
Warnings/Precautions
Warnings
Hematologic Effects
Thrombotic thrombocytopenic purpura/hemolytic uremic syndrome (sometimes fatal) reported in patients with advanced HIV infection and in allogeneic bone marrow or renal transplant recipients receiving high dosages (8 g daily).
General Precautions
Renal Effects
Use of inappropriately high dosage for the level of renal function has resulted in acute renal failure in patients with underlying renal disease.
Acyclovir may precipitate in renal tubules if solubility (2.5 mg/mL) is exceeded in intratubular fluid. Maintain adequate hydration.
If acute renal failure and anuria occur, hemodialysis recommended until normal renal function returns.
CNS Effects
Use of inappropriately high dosage for the level of renal function has resulted in CNS symptoms in patients with underlying renal disease.
Genital Herpes
Valacyclovir is not a cure for genital herpes.
Avoid sexual contact while lesions and/or symptoms are present due to risk of infecting sexual partners. Infection can be transmitted in the absence of symptoms through asymptomatic viral shedding.
Although use for suppressive therapy in immunocompetent individuals with genital herpes decreases the risk for heterosexual transmission, safer sex practices also should be used. Efficacy for reducing transmission not established in individuals with multiple partners or in non-heterosexual couples.
Type-specific serologic testing of asymptomatic partners of individuals with genital herpes can determine whether risk for HSV-2 acquisition exists.
Valacyclovir has not been shown to reduce transmission of sexually transmitted infections other than HSV-2.
Recommended by CDC and others for episodic treatment of genital herpes or chronic suppressive therapy of recurrent episodes in HIV-infected adults and adolescents, but manufacturer says efficacy not established for treatment of genital herpes in HIV-infected individuals and safety and efficacy not established for chronic suppressive therapy in those with advanced HIV disease (CD4+ T-cell count <100/mm3).
Herpes Labialis
Valacyclovir is not a cure for cold sores.
Treatment should not exceed a single day; therapy beyond 1 day does not provide additional clinical benefits.
Because of high dosage, use caution when prescribing valacyclovir for treatment of cold sores in geriatric individuals or those with renal impairment. (See Special Populations under Dosage and Administration.)
Safety and efficacy not established for treatment of cold sores in immunocompromised individuals.
Herpes Zoster
Safety and efficacy not established for treatment of disseminated herpes zoster or for treatment of herpes zoster in immunocompromised individuals.
Specific Populations
Pregnancy
Category B.
Lactation
Acyclovir distributed into human milk following oral administration of valacyclovir. Use valacyclovir with caution.
Pediatric Use
Safety and efficacy not established in prepubertal children.
Geriatric Use
Increased risk of adverse renal or CNS effects. CNS effects reported more frequently in geriatric adults than in younger adults include agitation, hallucinations, confusion, delirium, and encephalopathy.
In herpes zoster, longer duration of pain after healing (post-herpetic neuralgia) than in younger adults.
Consider age-related decreases in renal function when selecting dosage and adjust dosage if necessary. (See Renal Impairment under Dosage and Administration.)
Renal Impairment
Decreased clearance; increased risk of adverse renal and CNS effects in patients with underlying renal disease receiving high dosages.
Adjust dosage as necessary. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Headache, nausea, vomiting.
Drug Interactions
Neither valacyclovir nor acyclovir metabolized by CYP isoenzymes.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
No effect on acyclovir pharmacokinetics |
Use usual dosages |
|
Cimetidine |
Potential increased peak plasma concentrations and AUC of acyclovir |
Not considered clinically important if renal function normal; use usual dosages |
|
Digoxin |
No effect on pharmacokinetics of acyclovir or digoxin |
Use usual dosages |
|
Probenecid |
Potential increased peak plasma concentrations and AUC of acyclovir |
Not considered clinically important if renal function normal; use usual dosage |
|
Thiazide diuretics |
No effect on acyclovir pharmacokinetics |
Use usual dosages |
valACYclovir Pharmacokinetics
Absorption
Bioavailability
Valacyclovir hydrochloride, a prodrug of acyclovir, is rapidly absorbed following oral administration and almost completely converted to acyclovir andl-valine by first-pass intestinal and/or hepatic metabolism.
Absolute bioavailability of acyclovir approximately 54% following oral administration of valacyclovir hydrochloride; peak acyclovir plasma concentrations attained within 1.7 hours.
Food
Administration of valacyclovir with food does not alter acyclovir bioavailability.
Distribution
Extent
Although there are no adequate studies using valacyclovir, acyclovir crosses the placenta.
Following oral administration of valacyclovir to the mother, acyclovir is distributed into milk.
Plasma Protein Binding
13.5–17.9% bound to plasma proteins.
Elimination
Metabolism
Valacyclovir hydrochloride rapidly converted to acyclovir and l-valine by first-pass intestinal and/or hepatic metabolism. Acyclovir converted to acyclovir monophosphate, diphosphate, and triphosphate in cells infected with herpesviruses.
Neither valacyclovir nor acyclovir metabolized by CYP enzymes.
Elimination Route
Valacyclovir principally eliminated as acyclovir; 46 and 47% of an oral dose eliminated in urine and feces, respectively.
Half-life
Plasma elimination half-life of acyclovir after oral administration of valacyclovir averages 2.5–3.3 hours.
Special Populations
Renal clearance and elimination half-life decreased in patients with renal impairment; half-life averages 14 hours in end-stage renal disease.
Pharmacokinetics in geriatric patients vary depending on renal function.
Stability
Storage
Oral
Tablets
15–25°C.
Actions and Spectrum
-
Valacyclovir is thel-valine ester of acyclovir. Prodrug with no antiviral activity until converted in vivo to acyclovir and subsequently to the active acyclovir triphosphate.
-
GI absorption of valacyclovir substantially greater than absorption of oral acyclovir resulting in plasma acyclovir concentrations comparable to those achieved with IV acyclovir.
-
Active against Herpesviridae including herpes simplex virus types 1 and 2 (HSV-1 and HSV-2), varicella-zoster virus (VZV), and cytomegalovirus (CMV).
-
Acyclovir highly selective for thymidine kinase encoded by HSV and VZV, which converts acyclovir into acyclovir monophosphate, which is further converted to the diphosphate and then to the active triphosphate via other cellular enzymes. Also exhibits activity against viruses that do not code for this enzyme.
-
Inhibits viral DNA replication by competitive inhibition of viral DNA polymerase, incorporation and termination of the growing viral DNA chain, and inactivation of the viral DNA polymerase.
-
Resistant strains of HSV and VZV reported.
Advice to Patients
-
Advise patients that valacyclovir is not a cure for genital herpes or herpes labialis (cold sores).
-
Importance of avoiding sexual contact with uninfected partners while genital herpes lesions and/or symptoms are present since there is a risk of transmission. Genital herpes can be transmitted in the absence of symptoms.
-
Importance of using safer sex practices in conjunction with use of valacyclovir for suppressive therapy of genital herpes.
-
Importance of initiating treatment of genital herpes recurrence as soon as possible following onset of signs and symptoms.
-
For treatment of herpes labialis, importance of initiating treatment immediately following onset of symptoms (tingling, itching, burning) and importance of not using valacyclovir for longer than 1 day.
-
Importance of maintaining adequate hydration during treatment.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
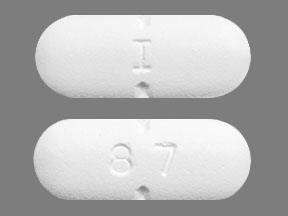
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
500 mg (of valacyclovir) |
Valtrex Caplets (with povidone) |
GlaxoSmithKline |
|
1 g (of valacyclovir) |
Valtrex Caplets (with povidone) |
GlaxoSmithKline |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What are the most common skin conditions? (with photos)
- What would be the benefits of taking valacyclovir vs acyclovir?
More about valacyclovir
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (496)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: purine nucleosides
- Breastfeeding
- En español