Pimavanserin (Monograph)
Brand name: Nuplazid
Drug class: Atypical Antipsychotics
Warning
- Increased Mortality in Geriatric Patients with Dementia-related Psychosis
-
Geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death.
-
Antipsychotic agents, including pimavanserin, are not approved for the treatment of dementia-related psychosis.
Introduction
Atypical antipsychotic agent.
Uses for Pimavanserin
Parkinson's Disease Psychosis
Management of hallucinations and delusions associated with Parkinson's disease psychosis.
A 2019 evidence-based medicine review by the International Parkinson and Movement Disorder Society states that clozapine and pimavanserin are “clinically useful” agents for the treatment of psychosis associated with Parkinson’s disease.
Not approved for treatment of dementia-related psychosis not related to the hallucinations and delusions associated with Parkinson’s disease psychosis.
Pimavanserin Dosage and Administration
General
Pretreatment Screening
-
Assess patients for a history of cardiac arrhythmias, symptomatic bradycardia, hypokalemia, or hypomagnesemia that could increase the risk of torsades de pointes and/or sudden death with pimavanserin use. Avoid pimavanserin use in such patients.
-
Screen patients for known QT prolongation and the use of other medications known to prolong the QT interval such as class 1A (e.g., quinidine, procainamide), or class 3 antiarrhythmics (e.g., amiodarone, sotalol), certain antipsychotic medications (e.g., ziprasidone, chlorpromazine, thioridazine) and fluoroquinolones.
Administration
Oral Administration
Administer orally (as tablets or capsules) without regard to food.
Swallow capsules whole, or opened and sprinkled over 15 mL (1 tablespoon) of applesauce, yogurt, pudding, or liquid nutritional supplement. If the capsule is opened and a drug/food mixture is created, swallow the mixture immediately and do not save for future use.
Dosage
Available as pimavanserin tartrate; dosage expressed in terms of pimavanserin.
Adults
Parkinson's Disease Psychosis
Oral
34 mg once daily without dosage titration.
If used concomitantly with a potent CYP3A4 inhibitor, reduce dosage to 10 mg once daily.
Avoid concomitant use with potent or moderate CYP3A4 inducers.
Special Populations
Hepatic Impairment
No dosage adjustment required.
Renal Impairment
No dosage adjustment required; however, increased exposure to pimavanserin observed in patients with severe renal impairment (Clcr≤30 mL/minute). Use with caution in severe renal impairment and end-stage renal disease.
Geriatric Patients
No dosage adjustment required.
Cautions for Pimavanserin
Contraindications
-
Known hypersensitivity to pimavanserin or any of its components.
Warnings/Precautions
Warnings
Increased Mortality in Geriatric Patients with Dementia-related Psychosis
Possible increased risk of death with antipsychotics in geriatric patients with dementia-related psychosis. (See Boxed Warning.)
Pimavanserin is not approved for the management of patients with dementia-related psychosis not related to hallucinations and delusions associated with Parkinson’s disease psychosis.
Other Warnings and Precautions
QT Interval Prolongation
Risk of QT interval prolongation.
Avoid use in patients with known QT interval prolongation and in those receiving drugs that prolong the QT interval. Avoid use in patients with history of cardiac arrhythmias or other conditions that may increase the risk of torsades de pointes and/or sudden death (e.g., symptomatic bradycardia, hypokalemia or hypomagnesemia).
Specific Populations
Pregnancy
No available data in pregnant women. Animal reproduction studies revealed no evidence of teratogenic effects; however, maternal toxicity and reduced pup survival and growth observed.
Lactation
Not known whether distributed into human milk. Also not known if drug has any effect on milk production or the nursing infant.
Consider benefits of breast-feeding along with importance of pimavanserin to the woman and any potential adverse effects on infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
Majority of patients in clinical studies were ≥65 years of age. No clinically important differences in safety or efficacy observed between patients 65–75 years of age and those >75 years of age.
Hepatic Impairment
No dosage adjustments necessary based on exposure differences observed in patients with and without hepatic impairment.
Renal Impairment
Pimavanserin exposure in patients with mild to moderate renal impairment similar to that in patients with normal renal function.
Pimavanserin exposure increased in patients with severe renal impairment based on peak plasma concentrations and AUC. Use with caution in patients with severe renal impairment and end-stage renal disease. Dialysis not shown to alter concentrations of pimavanserin.
Common Adverse Effects
Adverse effects reported in ≥5% of patients receiving pimavanserin in clinical studies at more than twice the rate as with placebo include peripheral edema and confusional state.
Drug Interactions
Metabolized principally by CYP3A4 and 3A5. Does not cause clinically important inhibition or induction of CYP3A4. The active metabolite does not induce CYP3A to a clinically important extent and is not expected to induce other CYP enzymes. Neither pimavanserin nor its active metabolite appears to inhibit any of the major CYP isoenzymes involved in drug metabolism (CYP1A2, 2B6, 2C8, 2C9, 2C19, 2D6, and 3A4).
Not a substrate of P-glycoprotein (P-gp), breast cancer resistance protein (BCRP), or organic anion transport proteins (OATP) 1B1 and 1B3.
Drugs Affecting Hepatic Microsomal Enzymes
Potent inhibitors of CYP3A4: Possible increased exposure of pimavanserin. Reduce pimavanserin dosage to 10 mg once daily.
Potent and moderate inducers of CYP3A4: Avoid concomitant use.
Drugs Associated with QT Prolongation
Potential additive effects on QT interval prolongation, which may increase risk of cardiac arrhythmias. Avoid concomitant use.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Antiarrhythmic agents, class Ia and III (e.g., amiodarone, disopyramide, procainamide, quinidine, sotalol) |
Potential additive effect on QT interval prolongation |
Avoid concomitant use |
|
Anticonvulsants (carbamazepine, phenytoin) |
Possible decreased exposure of pimavanserin |
Avoid concomitant use |
|
Anti-infective agents that prolong QT interval (e.g., gatifloxacin, moxifloxacin) |
Potential additive effect on QT interval prolongation |
Avoid concomitant use |
|
Antipsychotic agents that prolong QT interval (e.g., chlorpromazine, thioridazine, ziprasidone) |
Potential additive effect on QT interval prolongation |
Avoid concomitant use |
|
Carbidopa/levodopa |
No dosage adjustment of carbidopa/levodopa necessary |
|
|
Clarithromycin |
Possible increased exposure of pimavanserin |
Reduce dosage of pimavanserin to 10 mg once daily |
|
Indinavir |
Possible increased exposure of pimavanserin |
Reduce dosage of pimavanserin to 10 mg once daily |
|
Itraconazole |
Possible increased exposure of pimavanserin |
Reduce dosage of pimavanserin to 10 mg once daily |
|
Ketoconazole |
Increased peak plasma concentration and AUC of pimavanserin by 1.5- and 3-fold, respectively |
Reduce dosage of pimavanserin to 10 mg once daily |
|
Midazolam |
Based on pharmacokinetic studies, no effect of pimavanserin on midazolam |
|
|
Rifampin |
Possible decreased exposure of pimavanserin |
Avoid concomitant use |
|
St. John's wort (Hypericum perforatum) |
Possible decreased exposure of pimavanserin |
Avoid concomitant use |
Pimavanserin Pharmacokinetics
Absorption
Bioavailability
> 99.7% following oral administration.
Exhibits dose-proportional pharmacokinetics following single oral doses (range 17–255 mg).
Food
Food exhibits no substantial effect; peak plasma concentration decreased by approximately 9%, while AUC increased by 8% when administered with a high-fat meal.
Distribution
Extent
Not known if distributed into human milk.
Plasma Protein Binding
Approximately 95%.
Elimination
Metabolism
Metabolized principally by CYP3A4/5, and to a lesser extent by CYP2D6, CYP2J2, and various other CYP and flavin-containing monooxygenase isoenzymes.
Elimination Route
Approximately 0.6% of radiolabeled dose excreted in urine as unchanged drug, and 1.5% eliminated in feces after 10 days.
<1% of administered dose of pimavanserin and its active metabolite recovered in urine.
Half-life
Approximately 57 hours; 200 hours for active metabolite.
Stability
Storage
Oral
Capsules and tablets
20–25°C (excursions permitted to 15–30°C).
Actions
-
Exact mechanism of antipsychotic action unclear; may be mediated by a combination of inverse agonist and antagonist activity at serotonin type 2A (5-HT2A) receptors, and to a lesser extent at 5-HT2C receptors.
-
Exhibits potent inverse agonist activity at 5-HT2A receptors; lesser affinity for 5-HT2C receptors.
-
No appreciable affinity for 5-HT2B, dopaminergic, muscarinic, histaminergic, or adrenergic receptors.
-
Structurally and pharmacologically distinct from other atypical antipsychotic agents.
Advice to Patients
-
Advise patients and caregivers that geriatric patients with dementia-related psychosis treated with antipsychotic agents are at an increased risk of death. Patients and caregivers also should be informed that pimavanserin is not approved for the management of patients with dementia-related psychosis not related to the hallucinations and delusions associated with Parkinson’s disease psychosis.
-
Importance of patients informing their providers of any history of cardiac arrhythmias, symptomatic bradycardia, hypokalemia, or hypomagnesemia that could increase the risk of torsades de pointes or sudden death with pimavanserin use.
-
Importance of informing clinicians of existing or contemplated therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Pimavanserin is available only from designated specialty distributors and pharmacies. The manufacturer should be contacted for additional information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
34 mg (of pimavanserin) |
Nuplazid |
Acadia |
|
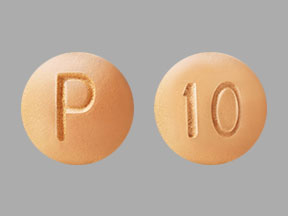
Tablets |
10 mg (of pimavanserin) |
Nuplazid |
Acadia |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
More about pimavanserin
- Check interactions
- Compare alternatives
- Reviews (15)
- Side effects
- Dosage information
- During pregnancy
- Drug class: atypical antipsychotics
- Breastfeeding
- En español