Clarithromycin (Monograph)
Brand name: Biaxin
Drug class: Other Macrolides
- Antimycobacterial Agents
Introduction
Antibacterial; macrolide antibiotic.
Uses for Clarithromycin
Acute Otitis Media (AOM)
Treatment of AOM caused by H. influenzae, M. catarrhalis, or S. pneumoniae.
Not a drug of first choice; considered an alternative for patients with a history of type I penicillin hypersensitivity. May not be effective for AOM that fails to respond to amoxicillin since S. pneumoniae resistant to amoxicillin also may be resistant to clarithromycin.
Pharyngitis and Tonsillitis
Treatment of pharyngitis or tonsillitis caused by susceptible Streptococcus pyogenes (group A β-hemolytic streptococci). Generally effective in eradicating S. pyogenes from the nasopharynx, but efficacy in the prevention of subsequent rheumatic fever has not been established to date.
CDC, AAP, IDSA, AHA, and others recommend oral penicillin V or IM penicillin G benzathine as treatments of choice; oral cephalosporins and oral macrolides considered alternatives. Amoxicillin sometimes used instead of penicillin V, especially for young children.
Consider that strains of S. pyogenes resistant to macrolides are common in some areas of the world (e.g., Japan, Finland) and clarithromycin-resistant strains have been reported in the US. (See Selection and Use of Anti-infectives under Cautions.)
Respiratory Tract Infections
Treatment of acute maxillary sinusitis caused by Haemophilus influenzae, Moraxella catarrhalis, or S. pneumoniae.
Treatment of acute bacterial exacerbations of chronic bronchitis caused by H. influenzae, H. parainfluenzae, M. catarrhalis, or S. pneumoniae.
Treatment of mild to moderate community-acquired pneumonia (CAP) caused by H. influenzae, Mycoplasma pneumoniae, Chlamydophila pneumoniae (Chlamydia pneumoniae), S. pneumoniae, H. parainfluenzae, or M. catarrhalis.
Treatment of Legionnaires’ disease† [off-label] caused by Legionella pneumophila. Drugs of choice are macrolides (usually azithromycin) or fluoroquinolones with or without rifampin.
Treatment of pertussis† [off-label] caused by Bordetella pertussis. Erythromycin traditionally has been drug of choice for treatment and postexposure prophylaxis of pertussis, but other macrolides (azithromycin, clarithromycin) appear to be as effective and may be associated with better compliance because they are better tolerated.
Skin and Skin Structure Infections
Treatment of uncomplicated skin or skin structure infections caused by Staphylococcus aureus or S. pyogenes.
Helicobacter pylori Infection and Duodenal Ulcer Disease
Treatment of Helicobacter pylori infection and duodenal ulcer disease (active or 1-year history of duodenal ulcer); eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence.
Used in a multidrug regimen that includes amoxicillin, clarithromycin, and either lansoprazole or omeprazole (triple therapy). Also used with omeprazole (dual therapy) or ranitidine bismuth citrate (dual therapy).
Bartonella Infections
Treatment of infections caused by B. henselae † [off-label] (e.g., cat scratch disease, bacillary angiomatosis, peliosis hepatitis).
Cat scratch disease generally self-limited in immunocompetent individuals and may resolve spontaneously in 2–4 months; some clinicians suggest that anti-infectives be considered for acutely or severely ill patients with systemic symptoms, particularly those with hepatosplenomegaly or painful lymphadenopathy, and such therapy probably is indicated in immunocompromised patients.
Anti-infectives also indicated in patients with B. henselae infections who develop bacillary angiomatosis, neuroretinitis, or Parinaud’s oculoglandular syndrome.
Optimum regimens have not been identified; some clinicians recommend azithromycin, clarithromycin, ciprofloxacin, erythromycin, doxycycline, rifampin, co-trimoxazole, gentamicin, or third generation cephalosporins.
Cryptosporidiosis
May decrease incidence of cryptosporidiosis† [off-label] in HIV-infected adults. Anti-infectives may suppress the infection, but none has been found to reliably eradicate Cryptosporidium. CDC, NIH, IDSA, and others state that the most appropriate treatment for cryptosporidiosis in HIV-infected individuals is the use of potent antiretroviral agents (to restore immune function) and symptomatic treatment of diarrhea.
Lyme Disease
Alternate for treatment of early Lyme disease† [off-label]. IDSA, AAP, and others recommend doxycycline, amoxicillin, or cefuroxime; macrolides may be less effective than these first-line agents.
Mycobacterial Infections
Primary prevention (primary prophylaxis) of Mycobacterium avium complex (MAC) bacteremia or disseminated infections in adults, adolescents, and children with advanced HIV infection. Recommended by USPHS/IDSA as a drug of choice for primary prevention of MAC in HIV-infected patients.
Treatment of disseminated MAC infection in HIV-infected adults, adolescents, and children. ATS, CDC, NIH, IDSA, and others recommend a regimen of clarithromycin (or azithromycin) and ethambutol and state that consideration may be given to adding a third drug (preferably rifabutin). Clarithromycin usually the preferred macrolide for initial treatment; azithromycin can be substituted if clarithromycin cannot be used because of drug interactions or intolerance and is preferred in pregnant women.
Prevention of recurrence (secondary prophylaxis) of disseminated MAC infection in HIV-infected adults, adolescents, and children. USPHS/IDSA, CDC, NIH, IDSA, and others recommend a macrolide (clarithromycin or azithromycin) given with ethambutol (with or without rifabutin). Azithromycin usually the preferred macrolide for use in conjunction with ethambutol for secondary prophylaxis in pregnant women.
Treatment of pulmonary MAC infections in HIV-negative patients†. A multiple-drug regimen of clarithromycin (or azithromycin), ethambutol, and either rifabutin or rifampin usually recommended.
Treatment of M. kansasii infections†; an alternative agent.
Treatment of cutaneous infections caused by M. abscessus or Mycobacterium chelonae †.
Treatment of cutaneous M. marinum infection†.
Toxoplasmosis
Has been used in conjunction with pyrimethamine for treatment of encephalitis caused by Toxoplasma gondii † in HIV-infected patients; not a preferred or alternative agent. CDC, NIH, IDSA, and others usually recommend pyrimethamine in conjunction with sulfadiazine and leucovorin for treatment of toxoplasmosis in adults and children, especially immunocompromised patients (e.g., HIV-infected individuals).
Prevention of Bacterial Endocarditis
Alternative for prevention of α-hemolytic (viridans group) streptococcal endocarditis† in penicillin-allergic patients undergoing certain dental, oral, respiratory tract, or esophageal procedures who have cardiac conditions that put them at high or moderate risk.
Consult most recent AHA recommendations for specific information on which cardiac conditions are associated with high or moderate risk of endocarditis and which procedures require prophylaxis.
Clarithromycin Dosage and Administration
Administration
Oral Administration
Conventional tablets and oral suspension: Administer orally without regard to meals. Oral suspension may be administered with milk.
Extended-release tablets: Administer orally with food. Should be swallowed whole and not chewed, broken, or crushed.
Reconstitution
Reconstitute granules for oral suspension at the time of dispensing by adding the amount of water specified on the bottle in two portions; agitate well after each addition. Agitate well just prior to use.
Dosage
Extended-release tablets may be used only for treatment of acute maxillary sinusitis, acute bacterial exacerbations of chronic bronchitis, and CAP in adults; safety and efficacy not established for treatment of other infections in adults or for use in pediatric patients.
Pediatric Patients
Acute Otitis Media (AOM)
Oral
7.5 mg/kg every 12 hours for 10 days.
Pharyngitis and Tonsillitis
Oral
7.5 mg/kg every 12 hours for 10 days.
Respiratory Tract Infections
Acute Bacterial Sinusitis
Oral7.5 mg/kg every 12 hours for 10 days.
Community-acquired Pneumonia (CAP)
Oral7.5 mg/kg every 12 hours for 10 days.
Pertussis†
Oral15–20 mg/kg daily in 2 divided doses (up to 1 g daily) for 7 days. 7.5 mg/kg twice daily for 7 days has been used in children 1 month to 16 years of age.
Skin and Skin Structure Infections
Oral
7.5 mg/kg every 12 hours for 10 days.
Bartonella Infections†
Cat Scratch Disease Caused by Bartonella henselae†
Oral500 mg daily for 4 weeks.
Bartonella Infections in HIV-infected Individuals†
OralAdolescents: 500 mg twice daily for ≥3 months recommended by CDC, NIH, and IDSA. If relapse occurs, consider lifelong secondary prophylaxis (chronic maintenance therapy) with erythromycin or doxycycline.
Lyme Disease†
Oral
7.5 mg/kg (up to 500 mg) twice daily for 14–21 days for treatment of early localized or early disseminated disease.
Mycobacterium avium Complex (MAC) Infections
Primary Prevention of MAC in Children with Advanced HIV Infection
Oral7.5 mg/kg (up to 500 mg) every 12 hours.
USPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <750/mm3 in those <1 year, <500/mm3 in those 1–2 years, <75/mm3 in those 2–6 years, or <50/mm3 in those ≥6 years of age.
Primary Prevention of MAC in Adolescents with Advanced HIV Infection
Oral500 mg every 12 hours.
USPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <50/mm3. May be discontinued if there is immune recovery in response to antiretroviral therapy and an increase in CD4+ T-cell count to >100/mm3 sustained for ≥3 months. Reinitiate prophylaxis if CD4+ T-cell count decreases to <50–100/mm3.
Treatment of Disseminated MAC in HIV-infected Children
OralManufacturer recommends 7.5 mg/kg (up to 500 mg) every 12 hours.
CDC, NIH, and IDSA recommend 7.5–15 mg/kg (maximum 500 mg) twice daily in conjunction with ethambutol (15–25 mg/kg once daily [up to 1 g daily]) with or without rifabutin (10–20 mg/kg once daily [up to 300 mg daily]).
Treatment of Disseminated MAC in HIV-infected Adolescents
Oral500 mg every 12 hours in conjunction with ethambutol (15 mg/kg daily) with or without a third drug (e.g., rifabutin 300 mg once daily) recommended by CDC, NIH, and IDSA. Higher dosage not recommended since such dosage has been associated with reduced survival in clinical studies.
Prevention of MAC Recurrence in HIV-infected Children
Oral7.5 mg/kg (maximum 500 mg) twice daily in conjunction with ethambutol (15 mg/kg [maximum 900 mg] once daily) with or without rifabutin (5 mg/kg [maximum 300 mg] once daily).
Secondary prophylaxis to prevent MAC recurrence in HIV-infected children usually continued for life. The safety of discontinuing secondary MAC prophylaxis in children whose CD4+ T-cell count increases in response to antiretroviral therapy has not been studied.
Prevention of MAC Recurrence in HIV-infected Adolescents
Oral500 mg every 12 hours in conjunction with ethambutol (15 mg/kg once daily) with or without rifabutin (300 mg once daily).
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adolescents. USPHS/IDSA states that consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 sustained for ≥6 months.
Treatment of Cutaneous Mycobacterium abscessus Infections†
Oral15 mg/kg daily (with or without incision and drainage of lesions) has been used in children 1–15 years of age.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental, Oral, Respiratory Tract, or Esophageal Procedures
Oral15 mg/kg as a single dose given 1 hour prior to the procedure.
Adults
Pharyngitis and Tonsillitis
Oral
250 mg every 12 hours for 10 days.
Respiratory Tract Infections
Acute Bacterial Sinusitis
OralConventional tablets or oral suspension: 500 mg every 12 hours for 14 days.
Extended-release tablets: 1 g (two 500-mg extended release tablets) once daily for 14 days.
Acute Exacerbations of Chronic Bronchitis
OralConventional tablets or oral suspension: 500 mg every 12 hours for 7–14 days for H. influenzae, 500 mg every 12 hours for 7 days for H. parainfluenzae, or 250 mg every 12 hours for 7–14 days for M. catarrhalis or S. pneumoniae.
Extended-release tablets: 1 g (two 500-mg extended-release tablets) once daily for 7 days.
Community-acquired Pneumonia (CAP)
OralConventional tablets or oral suspension: 250 mg every 12 hours for 7 days for H. influenzae or for 7–14 days for S. pneumoniae, C. pneumoniae, or M. pneumoniae.
Extended-release tablets: 1 g (two 500-mg extended-release tablets) once daily for 7 days.
Legionnaires’ Disease†
OralConventional tablets or oral suspension: 500 mg twice daily. Usual duration is 10 days for mild to moderate infections in immunocompetent patients; longer duration of treatment (3 weeks) may be necessary to prevent relapse, especially in those with more severe infections or with underlying comorbidity or immunodeficiency.
Skin and Skin Structure Infections
Oral
Conventional tablets or oral suspension: 250 mg every 12 hours for 7–14 days.
Helicobacter pylori Infection and Duodenal Ulcer Disease
Oral
Conventional tablets or oral suspension: 500 mg twice daily for 10 or 14 days given in conjunction with amoxicillin and lansoprazole (triple therapy); 500 mg twice daily for 10 days given in conjunction with amoxicillin and omeprazole (triple therapy); 500 mg 3 times daily for 14 days given in conjunction with omeprazole or ranitidine bismuth citrate (dual therapy).
Bartonella Infections†
Cat Scratch Disease Caused by Bartonella henselae†
OralConventional tablets or oral suspension: 500 mg daily for 4 weeks.
Bartonella Infections in HIV-infected Individuals†
OralConventional tablets or oral suspension: 500 mg twice daily for ≥3 months recommended by CDC, NIH, and IDSA. If relapse occurs, consider lifelong secondary prophylaxis (chronic maintenance therapy) with erythromycin or doxycycline.
Lyme Disease†
Oral
Conventional tablets or oral suspension: 500 mg twice daily for 14–21 days for treatment of early localized or early disseminated disease.
Mycobacterial Infections
Primary Prevention of MAC in Adults with Advanced HIV Infection
OralConventional tablets or oral suspension: 500 mg every 12 hours.
USPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <50/mm3. May be discontinued if there is immune recovery in response to antiretroviral therapy and an increase in CD4+ T-cell count to >100/mm3 sustained for ≥3 months. Reinitiate prophylaxis if CD4+ T-cell count decreases to <50–100/mm3.
Treatment of Disseminated MAC in HIV-infected Adults
OralConventional tablets or oral suspension: 500 mg every 12 hours in conjunction with ethambutol (15 mg/kg daily) with or without a third drug (e.g., rifabutin 300 mg once daily). Higher dosage not recommended since such dosage has been associated with reduced survival in clinical studies.
Prevention of MAC Recurrence in HIV-infected Adults
OralConventional tablets or oral suspension: 500 mg every 12 hours in conjunction with ethambutol (15 mg/kg once daily) with or without rifabutin (300 mg once daily).
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adults. USPHS/IDSA states that consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 sustained for ≥6 months.
Treatment of MAC in HIV-negative Adults†
OralConventional tablets or oral suspension: 500 mg every 12 hours in conjunction with ethambutol and rifabutin or rifampin.
Mycobacterium abscessus or M. chelonae Infections†
OralConventional tablets or oral suspension: 0.5–1 g twice daily for 6 months.
M. marinum Infections†
OralConventional tablets or oral suspension: 500 mg twice daily for at least 3 months.
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental, Oral, Respiratory Tract, or Esophageal Procedures
OralConventional tablets or oral suspension: 500 mg as a single dose given 1 hour prior to the procedure.
Special Populations
Hepatic Impairment
No dosage adjustment required.
Renal Impairment
If Clcr <30 mL/minute, reduce dose by 50% or double dosing interval. Alternatively (for conventional tablets or oral suspension), 500 mg initially followed by 250 mg twice daily (if the usual dosage in adults with normal renal function is 500 mg twice daily) or 250 mg daily (if the usual dosage in adults with normal renal function is 250 mg twice daily).
Geriatric Patients
No dosage adjustments except those related to renal impairment. (See Renal Impairment under Dosage and Administration.)
Cautions for Clarithromycin
Contraindications
-
Known hypersensitivity to clarithromycin, erythromycin, any macrolide, or any ingredient in the formulation.
Warnings/Precautions
Warnings
Increased Mortality
Increased risk of all-cause mortality reported during long-term follow-up of patients with coronary heart disease who received a 2-week course of clarithromycin in a randomized, placebo-controlled study. Variable results regarding effect of clarithromycin on risk of death or other heart-related adverse effects reported in other limited observational studies. A possible mechanism by which clarithromycin may increase the risk of death in patients with cardiovascular disease unknown.
Consider risk of all-cause mortality when weighing risks and potential benefits of the drug in all patients, particularly those with cardiovascular disease. Even if only a short course of clarithromycin is indicated, consider other available antibiotics in those with heart disease. Not indicated for the treatment of coronary artery disease.
Fetal/Neonatal Morbidity
Animal studies indicate adverse effects on pregnancy outcome and/or embryofetal development. Use during pregnancy only when safer drugs cannot be used or are ineffective.
Superinfection/Clostridium difficile-associated Colitis
Possible emergence and overgrowth of nonsusceptible bacteria or fungi with prolonged therapy. Institute appropriate therapy if superinfection occurs.
Treatment with anti-infectives may permit overgrowth of clostridia. Consider Clostridium difficile-associated diarrhea and colitis (antibiotic-associated pseudomembranous colitis) if diarrhea develops and manage accordingly.
Sensitivity Reactions
Hypersensitivity and Dermatologic Reactions
Possible allergic reactions (e.g., mild urticaria and skin eruptions). Severe reactions (e.g., anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported rarely.
General Precautions
Hepatic Effects
Severe, reversible hepatic dysfunction (including cholestasis, with or without jaundice) and hepatomegaly reported.
Fatal hepatic failure occurred in association with serious underlying disease and/or concomitant drugs.
Resistance in Helicobacter pylori
Increased risk of developing clarithromycin resistance if used as the sole anti-infective agent in regimens for treatment of H. pylori infection. If therapy fails, perform in vitro susceptibility testing. Do not use clarithromycin if H. pylori is resistant.
Cardiac Effects
Ventricular tachycardia and torsades de pointes reported rarely in patients with prolonged QT intervals.
History of Acute Porphyria
Concomitant therapy with ranitidine bismuth citrate not recommended.
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of clarithromycin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Consider that S. pyogenes (group A β-hemolytic streptococci) resistant to clarithromycin have been reported.
Specific Populations
Pregnancy
Category C. (See Fetal/Neonatal Morbidity under Cautions.)
Lactation
Distributed into milk following oral administration. Use with caution.
Pediatric Use
Safety and efficacy not established in children <6 months of age.
Manufacturer states safety not established in children <20 months of age with MAC infection, but USPHS/IDSA recommends use of the drug for HIV-infected infants and children.
Geriatric Use
Adverse effect profile similar to that in younger adults.
Dosage adjustment based solely on age not required.
Clearance may be reduced due to age-related decreases in renal function. Consider need for dosage adjustment in those with severe renal impairment. (See Renal Impairment under Dosage and Administration.)
Renal Impairment
Increased half-life. Dosage adjustment may be necessary. (See Renal Impairment under Dosage and Administration.)
Concomitant therapy with ranitidine bismuth citrate not recommended if Clcr <25 mL/minute.
Common Adverse Effects
GI adverse effects (diarrhea, nausea, abnormal taste, dyspepsia, abdominal pain) and headache.
Drug Interactions
Clarithromycin is metabolized by and inhibits CYP3A4.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with substrates, inhibitors, or inducers of CYP3A4 are likely.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amprenavir |
Increased amprenavir concentrations and AUC; possible decreased clarithromycin concentrations and decreased 14-hydroxyclarithromycin concentrations and AUC |
No dosage adjustments recommended |
|
Anticoagulants, oral |
Increased anticoagulant effect |
Monitor PT carefully |
|
Antihistamines (astemizole, terfenadine) |
Increased plasma concentrations of astemizole or terfenadine; prolonged QT interval and serious cardiac arrhythmias |
Contraindicated |
|
Antimycobacterials (rifabutin) |
Potential inhibition of rifabutin metabolism and induction of clarithromycin metabolism; possible increased incidence of uveitis with concomitant rifabutin and clarithromycin |
|
|
Atazanavir |
Increased atazanavir plasma concentrations; increased clarithromycin plasma concentrations and decreased 14-hydroxyclarithromycin plasma concentrations; increased clarithromycin concentrations may cause QTc prolongation |
Consider reducing clarithromycin dosage by 50%; consider alternative to clarithromycin for indications other than Mycobacterium avium complex (MAC) |
|
Benzodiazepines (alprazolam, midazolam, triazolam) |
Potential decreased clearance of midazolam or triazolam and increased pharmacologic effects of the benzodiazepines Somnolence and confusion reported with clarithromycin and triazolam |
|
|
Carbamazepine |
Increased carbamazepine plasma concentrations and carbamazepine toxicity (i.e., drowsiness, dizziness, ataxia) |
Use with caution; consider reducing carbamazepine dosage and/or monitoring plasma carbamazepine concentrations |
|
Cisapride |
Increased cisapride plasma concentrations; prolonged QT interval and serious cardiac arrhythmias; some fatalities |
Contraindicated |
|
Colchicine |
Possible increased risk of colchicine toxicity when used concomitantly with clarithromycin, especially in elderly patients and/or patients with renal impairment |
Some clinicians state colchicine and clarithromycin should not be used concomitantly |
|
Darifenacin |
Possible pharmacokinetic interaction |
Manufacturer of darifenacin states darifenacin dosage should not exceed 7.5 mg daily in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin) |
|
Delavirdine |
Increased clarithromycin concentrations and AUC; increased delavirdine concentrations |
Dosage adjustment not needed in those with normal renal function; reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute |
|
Didanosine |
No clinically important pharmacokinetic interactions |
|
|
Digoxin |
Increased serum digoxin concentrations and digoxin toxicity (including potentially fatal arrhythmias) |
Monitor serum digoxin concentrations carefully |
|
Disopyramide |
Potential increased half-life of disopyramide and risk of prolonged QT interval and serious cardiac arrhythmias |
Monitor ECGs and serum disopyramide concentrations |
|
Efavirenz |
Decreased clarithromycin AUC and peak plasma concentrations; increased 14-hydroxyclarithromycin AUC and peak plasma concentrations; no effect on AUC of efavirenz; rash reported with concomitant administration |
Dosage adjustment of efavirenz not recommended; monitor for efficacy of the macrolide or consider use of an alternative anti-infective |
|
Ergot alkaloids (ergotamine, dihydroergotamine) |
Acute ergot toxicity (vasospasm and ischemia of extremities and other tissues, including CNS) |
Concomitant use contraindicated |
|
Erlotinib |
Possible pharmacokinetic interaction |
Manufacturer of erlotinib recommends caution in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin); consider reducing erlotinib dosage if severe adverse effects occur |
|
Eszopiclone |
Possible pharmacokinetic interaction |
Manufacturer of eszopiclone recommends eszopiclone dosage be reduced in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin); initial eszopiclone dosage should be <1 mg, but may be increased to 2 mg if clinically indicated |
|
Fluconazole |
Increased clarithromycin plasma concentrations |
|
|
Fosamprenavir |
Studies using amprenavir indicate possible increased amprenavir concentrations and AUC |
Not considered clinically important; dosage adjustments not recommended |
|
Hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors |
Increased HMG-CoA reductase inhibitor plasma concentrations and potential for rhabdomyolysis |
|
|
Indinavir |
Increased indinavir and clarithromycin concentrations |
Indinavir manufacturer states appropriate dosages for concomitant use with respect to safety and efficacy not established; some experts state dosage adjustments not needed |
|
Lopinavir |
Increased clarithromycin AUC |
Reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute |
|
Nevirapine |
Decreased clarithromycin AUC and peak plasma concentration; increased 14-hydroxyclarithromycin AUC and peak plasma concentration; increased nevirapine concentrations |
Monitor for efficacy of the macrolide or use an alternative anti-infective |
|
Omeprazole |
Increased concentrations of clarithromycin, 14-hydroxyclarithromycin, and omeprazole |
|
|
Pimozide |
Potential increased pimozide plasma concentrations and risk of prolonged QT interval and serious cardiac arrhythmias |
Contraindicated |
|
Quinidine |
Risk of prolonged QT interval and serious cardiac arrhythmias |
Monitor ECGs and serum quinidine concentrations |
|
Ranitidine |
Increased plasma ranitidine concentrations and increased 14-hydroxyclarithromycin concentrations; not considered clinically important |
|
|
Ritonavir |
Increased AUC and peak plasma concentration of ritonavir and of clarithromycin; decreased AUC and peak plasma concentration of 14-hydroxyclarithromycin |
Dosage adjustment not needed in patients with normal renal function; reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute |
|
Saquinavir |
Increased clarithromycin AUC and plasma concentrations; decreased 14-hydroxyclarithromycin AUC; increased AUC and plasma concentrations of saquinavir |
Dosage adjustments may not be needed if used concomitantly for a limited time For those receiving ritonavir-boosted saquinavir, manufacturer of saquinavir states modification of dosage not necessary in those with normal renal function but clarithromycin dosage should be reduced 50% in those with Clcr 30–60 mL/minute and reduced 75% in those with Clcr <30 mL/minute |
|
Sildenafil |
Potential increased exposure to sildenafil |
Consider reducing sildenafil dosage |
|
Theophylline |
Potential increased serum theophylline concentrations |
Monitor serum theophylline concentrations in those receiving high theophylline dosage or with baseline in the upper therapeutic range; adjust theophylline dosage as needed when clarithromycin is initiated or discontinued |
|
Zidovudine |
Decreased zidovudine plasma concentrations |
Clarithromycin Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from GI tract. With conventional tablets or oral suspension, peak serum concentrations within 1–4 hours. With extended-release tablets, peak serum concentrations within 5–8 hours.
Absolute bioavailability of conventional tablets is about 50–55%; absolute bioavailability may be an underestimate of systemic activity because of rapid first-pass metabolism and an active metabolite (14-hydroxyclarithromycin).
Food
With conventional tablets, food causes a slight delay in onset of clarithromycin absorption but extent of absorption is unaffected. With extended-release tablets, food increases the extent of absorption by 30%.
Distribution
Extent
Clarithromycin and 14-hydroxyclarithromycin distributed into most body tissues and fluids in concentrations greater than serum concentrations.
Distributed into CSF following oral administration.
Not known whether clarithromycin is distributed into milk.
Plasma Protein Binding
42–72%.
Elimination
Metabolism
Extensively metabolized in the liver, principally by oxidative N-demethylation and hydroxylation. At least 7 metabolites identified; 14-hydroxyclarithromycin is the principal metabolite in serum and the only one with substantial antibacterial activity.
Elimination Route
Eliminated by both renal and nonrenal mechanisms; approximately 38% of a dose excreted in urine and 40% in feces.
Half-life
4–11 hours.
Special Populations
Renal impairment decreases clearance of clarithromycin and 14-hydroxyclarithromycin.
Hepatic impairment reduces formation of the active metabolite; however, an increase in renal clearance of the parent drug obviates the need for a dosage reduction unless renal impairment also is present.
Stability
Storage
Oral
For Suspension
Granules for oral suspension: Tight container at 15–30°C. Following reconstitution, do not refrigerate.
Tablets
Conventional 250-mg tablets: Tight, light-resistant container at 15–30°C and protect from light.
Conventional 500-mg tablets: Tight container at 20–25°C.
Extended-release tablets: 20–25°C (may be exposed to 15–30°C).
Clarithromycin Combinations
Kit containing clarithromycin, amoxicillin, and lansoprazole: 20–25°C.
Actions and Spectrum
-
Usually bacteriostatic, but may be bactericidal against highly susceptible organisms or when present in high concentrations.
-
Like other macrolides, inhibits protein synthesis in susceptible organisms by binding to 50S ribosomal subunits.
-
Spectrum of activity includes many gram-positive and -negative aerobic bacteria, many anaerobic bacteria, some mycobacteria, and some other organisms including Mycoplasma, Ureaplasma, Chlamydia, Toxoplasma, and Borrelia.
-
In vitro activity similar to or greater than that of erythromycin against erythromycin-susceptible organisms.
-
The principal metabolite (14-hydroxyclarithromycin) has clinically important antimicrobial activity.
-
Gram-positive aerobes: Active in vitro and in clinical infections against Staphylococcus aureus, S. pneumoniae, and S. pyogenes (group A β-hemolytic streptococci), Enterococci (e.g., Enterococcus faecalis) and oxacillin-resistant (methicillin-resistant) staphylococci are resistant.
-
Gram-negative aerobes: Active in vitro and in clinical infections against Haemophilus influenzae, H. parainfluenzae, and Moraxella catarrhalis.
-
Other organisms: Active in vitro and in clinical infections against C. pneumoniae and M. pneumoniae. Also active against MAC.
-
Organisms resistant to erythromycin generally resistant to clarithromycin.
-
Complete cross-resistance occurs between azithromycin and clarithromycin in MAC.
Advice to Patients
-
Advise patients that antibacterials (including clarithromycin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Importance of completing full course of therapy, even if feeling better after a few days.
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with clarithromycin or other antibacterials in the future.
-
Importance of taking clarithromycin extended-release tablets with food; clarithromycin immediate-release tablets and oral suspension can be taken without regard to meals.
-
Advise patients of the importance of informing clinician if they have heart disease, especially when an anti-infective is being prescribed, and the importance of seeking medical attention if they experience symptoms of a heart attack or stroke (e.g., chest pain, shortness of breath, pain or weakness in one part or side of the body, slurred speech).
-
Importance of reporting persistent or worsening symptoms of infection.
-
Importance of not refrigerating oral suspension.
-
Importance of discontinuing therapy and informing clinician if an allergic reaction occurs.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension |
125 mg/5 mL* |
Clarithromycin for Suspension |
|
|
250 mg/5 mL* |
Clarithromycin for Suspension |
|||
|
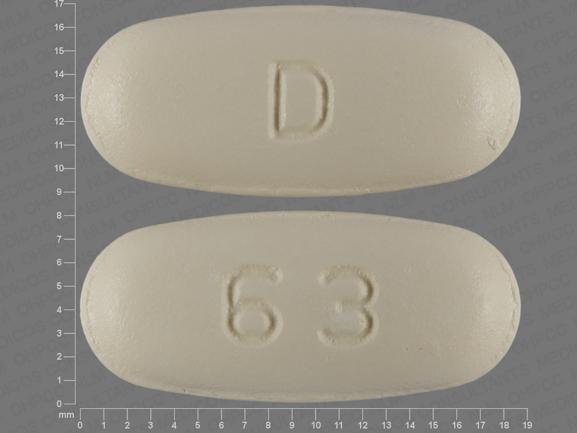
Tablets, film-coated |
250 mg* |
Biaxin Filmtab |
AbbVie |
|
|
Clarithromycin Tablets |
||||
|
500 mg* |
Biaxin Filmtab |
AbbVie |
||
|
Clarithromycin Tablets |
||||
|
Tablets, extended-release, film-coated |
500 mg* |
Clarithromycin Tablets Extended-release |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Kit |
4 Capsules, Amoxicillin (trihydrate) 500 mg (of amoxicillin) (Trimox) 2 Capsules, delayed-release (containing enteric-coated granules), Lansoprazole, 30 mg (Prevacid) 2 Tablets, film-coated, Clarithromycin, 500 mg (Biaxin Filmtab) 4 Capsules, Amoxicillin (trihydrate) 500 mg (of amoxicillin) 2 Capsules, delayed-release (containing enteric-coated granules), Lansoprazole, 30 mg 2 Tablets, film-coated, Clarithromycin, 500 mg |
Prevpac |
Takeda Pharmaceuticals |
|
Amoxicillin, Clarithromycin, and Lansoprazole |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What is the Best Antibiotic for Strep Throat?
- What are the best antibiotics for pneumonia?
- Do statins cause rhabdomyolysis, and how is it treated?
- Can Biaxin cause headaches?
- Can I drink alcohol while taking clarithromycin?
- Can clarithromycin be used to treat UTI's?
More about clarithromycin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (854)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: macrolides
- Breastfeeding
- En español