Carboplatin (Monograph)
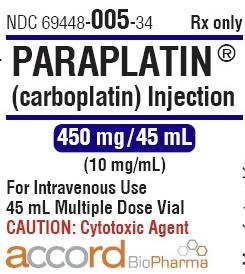
Brand name: Paraplatin
Drug class: Antineoplastic Agents
- Platinum-containing Agents
VA class: AN900
CAS number: 41575-94-4
Warning
-
Use only under the supervision of a qualified clinician experienced in the use of cytotoxic therapy. Use only when adequate treatment facilities for appropriate management of therapy and complications are available.
-
Dose-related bone marrow suppression may result in infection and/or bleeding. Anemia may be cumulative and may require transfusion support.
-
Vomiting is a common adverse effect.
-
Anaphylactic-like reactions may occur within minutes of administration. Administer epinephrine, corticosteroids, and/or antihistamines to relieve symptoms.
Introduction
Antineoplastic agent; platinum-containing compound.
Uses for Carboplatin
Carboplatin and cisplatin appear to have similar efficacy in the treatment of platinum-responsive ovarian tumors, lung cancers† [off-label], and certain head and neck cancers† [off-label]; carboplatin is less effective than cisplatin in certain testicular cancers.
Because carboplatin and cisplatin have different toxicity profiles, carboplatin may be effective in patients with platinum-responsive tumors who are unable to tolerate cisplatin because of renal impairment, refractory nausea, hearing impairment, or neuropathy; cisplatin may be preferred in patients with decreased bone marrow reserve or high risk of sepsis or those requiring anticoagulation therapy.
Ovarian Cancer
Treatment of ovarian cancer (alone and as combination therapy).
Combination therapy with platinum-containing agent (carboplatin or cisplatin) and paclitaxel† [off-label] is the preferred regimen for initial treatment of advanced epithelial ovarian cancer; therapy with platinum-containing agent and paclitaxel is superior to therapy with platinum-containing agent and cyclophosphamide. Carboplatin is as effective as but less toxic than cisplatin when used in combination with paclitaxel or cyclophosphamide.
Carboplatin in combination with docetaxel has been used for the first-line treatment of ovarian cancer† [off-label] and has demonstrated similar efficacy and a different tolerability profile (i.e., more hematologic toxicity but less neurotoxicity) compared with carboplatin in combination with paclitaxel.
Has been used as a single agent in the first-line treatment of advanced ovarian cancer† [off-label]. Role remains to be established, but some clinicians consider single-agent carboplatin a reasonable option.
Used alone as second-line therapy for palliative treatment of recurrent ovarian cancer in patients with platinum-sensitive disease; nonplatinum-based regimens generally preferred for retreatment of patients with platinum-refractory disease.
Being studied for use in combination regimens for second-line treatment of advanced ovarian epithelial cancer†.
Has been used alone or in combination therapy for adjuvant treatment of early-stage ovarian cancer†. Survival benefit may be limited to patients whose disease is associated with poorer prognosis.
Lung Cancer
Treatment of small cell lung cancer† as a component of combination regimens.
An active agent in non-small cell lung cancer†.
Cervical Cancer
Role in the treatment of cervical cancer† remains to be established. Current evidence supports use of cisplatin in chemotherapy regimens given concurrently with radiation therapy in patients with locally advanced cervical cancer; similar benefit from carboplatin-containing chemotherapy cannot be assumed.
An active agent in the treatment of metastatic or recurrent cervical cancer†. May be considered an alternative to cisplatin, particularly in patients with nephrotoxicity or neurotoxicity caused by advanced cervical tumor who are not candidates for cisplatin therapy.
Head and Neck Cancer
May be useful in the treatment of recurrent or metastatic squamous cell carcinoma of the head and neck†.
Wilms’ Tumor
Has shown activity in the management of Wilms’ tumor†.
Brain Tumors
Has been used for palliative treatment of various primary brain tumors†.
Has shown activity in the treatment of progressive or recurrent low-grade gliomas in children†; responses observed in adults with recurrent glioma, including those who had received previous chemotherapy with nitrosoureas.
Has shown activity in the treatment of recurrent medulloblastoma†.
Combination therapy with platinum-containing agent (cisplatin or carboplatin) and etoposide is used for treatment of intracranial germ cell tumors†.
Neuroblastoma
Used (as combination therapy) fortreatment of neuroblastoma†.
Testicular Cancer
Cisplatin-based regimen (i.e., cisplatin/etoposide or cisplatin/etoposide/bleomycin) is more effective than carboplatin-based regimen (i.e., carboplatin/etoposide or carboplatin/etoposide/bleomycin) for initial treatment of good-prognosis metastatic nonseminomatous germ cell tumor; generally reserve use of carboplatin regimen for patients who do not tolerate or who refuse cisplatin.
Limited data suggest that high-dose carboplatin and etoposide may be effective in some patients with relapsed or refractory germ cell tumors†.
Bladder Cancer
Has been substituted as a less toxic alternative to cisplatin in the treatment of advanced bladder cancer† in some patients receiving combination chemotherapy.
Combination therapy with paclitaxel followed by carboplatin is being studied in patients with advanced bladder cancer, including those with abnormal renal function.
Retinoblastoma
Has been used in combination with etoposide in a limited number of children† with recurrent or progressive retinoblastoma†.
Breast Cancer
Has been used in a limited number of patients with metastatic breast cancer†.
Endometrial Cancer
Being studied in the treatment of advanced or recurrent endometrial cancer†.
Carboplatin Dosage and Administration
General
-
Consult specialized references for procedures for proper handling and disposal of antineoplastics.
-
Carboplatin is considered a moderate antiemetic risk antineoplastic (i.e., 30–90% incidence of emesis without antiemetics). Antiemetic therapy (e.g., a 5-HT3 receptor antagonist and dexamethasone) is recommended to prevent nausea and vomiting. (See Emetogenic Effects under Cautions.)
-
Pretreatment and posttreatment hydration and/or diuresis are not necessary. (See Renal Effects under Cautions.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by IV infusion; also has been administered intraperitoneally†.
Needles, syringes, catheters, and IV administration sets that contain aluminum parts which may come in contact with carboplatin should not be used for preparation or administration.
Reconstitution
Reconstitute vial containing 50, 150, or 450 mg of carboplatin powder for injection with 5, 15, or 45 mL, respectively, of sterile water for injection, 5% dextrose injection, or 0.9% sodium chloride injection to provide a solution containing 10 mg/mL.
Resulting solutions can be further diluted to concentrations as low as 0.5 mg/mL with 5% dextrose injection or 0.9% sodium chloride injection.
Reconstituted solutions contain no preservatives; solutions preferably should be prepared immediately before use.
Dilution
May be diluted with 0.9% sodium chloride injection or 5% dextrose injection to a concentration as low as 0.5 mg/mL.
Rate of Administration
Administer by IV infusion over a period of ≥15 minutes; also has been administered by continuous IV infusion over 24 hours.
Dosage
Base dosage on the clinical, renal, and hematologic response and tolerance of the patient in order to obtain optimum therapeutic response with minimum adverse effects.
Initial dosage can be based on body surface area, but dosage may be more accurately calculated using formula dosing methods based on the patient’s renal function. (See Methods for Individualization of Dosage under Dosage and Administration.)
When used as a component of a multiple-drug regimen, consult published protocols for the dosage of each chemotherapeutic agent and the method and sequence of administration.
Adults
Ovarian Cancer
Initial Therapy for Advanced (Stage III and IV) Ovarian Carcinoma
IVInitially, 300 mg/m2 given in combination with cyclophosphamide. Adjust subsequent dosage according to the patient’s hematologic tolerance of the previous dose (see Dosage Adjustment in the Treatment of Ovarian Cancer); do not administer doses until hematologic function is within acceptable limits.
Alternatively, calculate dosage using formula dosing methods (see Methods for Individualization of Dosage).
A course of carboplatin consists of single doses administered once every 4 weeks (or longer if delayed for hematologic toxicity) for a total of 6 cycles.
Secondary Treatment of Advanced Ovarian Cancer
IVInitially, 360 mg/m2 as monotherapy. Administer drug once every 4 weeks (or longer if delayed for hematologic toxicity). Adjust subsequent dosage according to the patient’s hematologic tolerance of the previous dose (see Dosage Adjustment in the Treatment of Ovarian Cancer); do not administer doses until hematologic function is within acceptable limits.
Dosage Adjustment in the Treatment of Ovarian Cancer
|
Hematologic Toxicity |
Recommended Dosage Adjustment |
|---|---|
|
No hematologic toxicity (platelet count >100,000/mm3 and neutrophil count >2000/mm3) |
Increase dosage by 25% |
|
Mild or moderate hematologic toxicity (platelet count 50,000–100,000/mm3 or neutrophil count 500–2000/mm3) |
No adjustment in dosage |
|
Moderate to severe hematologic toxicity (platelet count <50,000/mm3 or neutrophil count <500/mm3) |
Decrease dosage by 25% |
Other Malignant Neoplasms
IV
Consult published protocols for dosages and methods and sequences of administration. In general, escalation of dosages above 400 mg/m2 results in substantial hematologic toxicity, but high-dose carboplatin (900–2000 mg/m2) has been used with colony-stimulating factors, autologous bone marrow rescue, and/or peripheral stem cell rescue.
Methods for Individualization of Dosage
Alternative methods for calculating initial carboplatin dosage have been suggested based on the patient’s pretreatment renal function or pretreatment renal function and desired platelet nadir.
Calvert Formula
Calculation is based on the patient’s GFR (in mL/minute) and the target AUC (in mg/mL per minute). Dosage is calculated in mg, not mg/m2.
|
Calvert Formula for Carboplatin Dosing: |
|---|
|
total dose (mg) = target AUC (in mg/mL per min) × [GFR (in mL/min) + 25] |
A target AUC of 5 (range: 4–6) mg/mL per minute appears to provide the most appropriate dosage range for use of carboplatin alone in patients previously treated with chemotherapeutic agents.
|
AUC (mg/mL x min) |
Percentage of Patients with Grade 3 or 4 Thrombocytopenia |
Percentage of Patients with Grade 3 or 4 Leukopenia |
|---|---|---|
|
4–5 |
16% |
13% |
|
6–7 |
33% |
34% |
For patients who previously did not receive chemotherapy, a target AUC of 7 (range: 6–8) mg/mL per minute has been recommended when carboplatin is used alone. Higher target AUCs (e.g., 7.5 mg/mL) also have been used (e.g., when carboplatin was used as a component of high-intensity dosing with paclitaxel and a hematopoietic agent for non-small cell lung carcinoma). Subsequent carboplatin dosage has been adjusted according to hematologic tolerance to the previous dose (e.g., reducing the dose by 25% for moderate to severe hematologic toxicity).
Formula is not sufficiently accurate to determine dosage for children or for adults with severe renal impairment (i.e., GFR <20 mL/minute); therefore, do not use this formula in such patients. Consult specialized references for an alternative pediatric formula.
Chatelut (French) Formula
Method does not require determination of GFR. Dosage is calculated in mg, not mg/m2.
|
Chatelut (French) Formula for Carboplatin Dosing: |
|---|
|
total dose (mg) = target AUC (in mg/mL per min) × carboplatin clearance (in mL/min) |
When carboplatin clearance is calculated as follows:
|
Carboplatin Clearance: |
|---|
|
Carboplatin clearance (mL/min) = (0.134 × wt) + ([218 × wt × (1 - {0.00457 × age})] × [1 - {0.314 × gender}] / serum creatinine (µmol/L)) (where weight is in kg, age is in years, and gender is 0 for males and 1 for females) |
Do not use this formula for calculating dosage in pediatric patients or those undergoing hemodialysis.
Special Populations
Renal Impairment
Reduce dosage in patients with Clcr <60 mL/minute.
|
Baseline Clcr |
Initial Dose |
|---|---|
|
41–59 mL/min |
250 mg/m2 |
|
16–40 mL/min |
200 mg/m2 |
Incidence of severe leukopenia, neutropenia, or thrombocytopenia at these adjusted initial dosages is about 25%. Adjust subsequent dosage according to the patient’s hematologic tolerance to the previous dose. Experience in patients with Clcr <15 mL/minute is too limited to make dosage recommendations.
Geriatric Patients
Use of dosing formulas incorporating estimates of GFR to determine dosage recommended in geriatric patients.
Cautions for Carboplatin
Contraindications
-
History of sensitivity reactions to carboplatin or other platinum-containing compounds (e.g., cisplatin).
-
Severe bone marrow depression or significant bleeding.
Warnings/Precautions
Warnings
Highly toxic drug with a low therapeutic index; therapeutic response is not likely to occur without some evidence of toxicity.
Hematologic Effects
The major and dose-limiting adverse effects are dose-related hematologic toxicity (thrombocytopenia, leukopenia, neutropenia, and/or anemia).
Myelosuppression appears to be most common and more severe in patients who received prior antineoplastic therapy (especially cisplatin-containing regimens), those concurrently receiving or having recently received other myelosuppressive drugs or radiation therapy, and those with renal impairment. Patients with poor performance status also appear to be at increased risk for severe leukopenia and thrombocytopenia. (See Interactions.)
At usual dosages, thrombocytopenia is more common and pronounced than leukopenia. Thrombocytopenia may be cumulative and occasionally require transfusions. Potential for infection.
Anemia may be severe or symptomatic (e.g., accompanied by asthenia). Incidence appears to be cumulative. Transfusions may be required, particularly in patients receiving prolonged (>6 cycles) therapy.
Monitor hematologic status carefully; perform peripheral blood counts at frequent intervals.
Do not administer to patients with severe bone marrow depression or substantial bleeding. In patients who experience myelosuppression, withhold subsequent cycles until neutrophil counts are >2000/mm3 and platelet counts are >100,000/mm3.
Treatment of severe hematologic toxicity may consist of supportive care, anti-infective agents for complicating infections, blood product transfusions, autologous bone marrow rescue, peripheral stem cell transplantation, and hematopoietic agents (colony-stimulating factors).
Emetogenic Effects
Carboplatin is classified as an antineoplastic agent of moderate emetic risk (i.e., 30–90% incidence of emesis without antiemetics). Acute vomiting episodes are most common in patients who received prior emetogenic antineoplastic regimens (especially cisplatin-containing regimens) and in those receiving other emetogenic agents concurrently.
Possible reduction in the incidence of nausea and vomiting when given as a 24-hour continuous IV infusion or IV in divided doses over 5 consecutive days rather than as a single IV infusion; however, efficacy of these schedules not established.
Pretreatment with antiemetics may reduce incidence and severity of emesis; rarely, nausea and vomiting may be refractory to antiemetic therapy. For prevention of acute emesis, ASCO recommends a 2-drug antiemetic regimen consisting of a type 3 serotonin (5-HT3) receptor antagonist and dexamethasone given before carboplatin.
For the prevention of delayed emesis following administration of carboplatin, ASCO recommends single-agent therapy with dexamethasone or a 5-HT3 receptor antagonist.
Optimal use of antiemetics for prevention of acute and delayed emesis during early courses of therapy is the most important means for preventing anticipatory vomiting; behavioral modification, hypnosis, and drug therapy (e.g., benzodiazepine with or without conventional antiemetics) also may be useful.
Peripheral Neuropathies
Possible peripheral neuropathies, generally sensory (e.g., paresthesia). Increased incidence in patients >65 years of age, those receiving prolonged therapy, and/or those who have received prior cisplatin therapy.
Preexisting cisplatin-induced peripheral neurotoxicity generally does not worsen during carboplatin therapy.
Otic Effects
Possible ototoxicity in patients receiving usual dosages of carboplatin in conjunction with cyclophosphamide.
Concomitant use of ototoxic drugs (e.g., aminoglycosides, furosemide, ifosfamide) may increase risk. (See Interactions.)
Ocular Effects
Loss of vision (sometimes complete for light and colors) reported in patients receiving higher than usually recommended dosages; improvement and/or total recovery of vision has occurred within weeks following drug discontinuance.
Hepatic Effects
Possible substantial abnormalities in liver function test results in patients receiving high doses (>4 times usual recommended dose) and autologous bone marrow transplantation.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; avoid pregnancy during therapy. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.
Embryotoxic and teratogenic in rats.
Sensitivity Reactions
Hypersensitivity Reactions
Prior exposure to other platinum-containing agents increases the risk for carboplatin-induced allergic reactions, including anaphylaxis.
Exposure (e.g., industrial) to platinum-containing compounds can cause asthma and immediate and delayed hypersensitivity reactions; consider the possibility that patients with a history of such exposure may be cross-sensitive to carboplatin.
Observe closely for possible hypersensitivity reactions. Appropriate equipment for maintenance of an adequate airway and other supportive measures and agents for the treatment of such reactions (e.g., antihistamines, epinephrine, oxygen, corticosteroids) should be readily available when carboplatin is administered.
General Precautions
Mutagenicity and Carcinogenicity
Mutagenic in vitro and in vivo.
Carcinogenic potential not fully studied; however, drugs with similar mechanisms of action and evidence of mutagenic effects have been reported to be carcinogenic. Secondary malignancies reported in patients receiving carboplatin in combination with other agents.
Renal Effects
Nephrotoxicity is less common and severe than that associated with cisplatin; concomitant IV hydration and diuresis generally not necessary. However, consider the possibility that nephrotoxicity may be potentiated by other nephrotoxic drugs. (See Interactions.)
Specific Populations
Pregnancy
Category D. (See Fetal/Neonatal Morbidity and Mortality under Cautions.)
Lactation
Not known whether carboplatin or its platinum-containing products are distributed into milk. Discontinue nursing during therapy.
Pediatric Use
Safety and efficacy not established.
Limited experience in the treatment of germ cell tumors in adolescents ≥16 years of age, various brain tumors or neuroblastoma in children 6 months to 19 years of age, and Wilms’ tumor in children 2–15 years of age.
Adverse effects reported to date in children are similar to those reported in adults and include hematologic toxicity (principally thrombocytopenia), adverse GI effects (e.g., nausea, vomiting), hypersensitivity reactions (e.g., urticaria, facial swelling, abdominal pain, coryza, cough), and hearing loss (particularly at higher than recommended doses in combination with other ototoxic agents).
Geriatric Use
In clinical trials evaluating carboplatin as combination therapy for ovarian cancer, age was not found to be a factor for survival in patients ≥65 years of age relative to younger adults.
Possible increased incidence of severe thrombocytopenia and carboplatin-induced peripheral neuropathy in adults ≥65 years of age compared with younger patients.
Consider increased incidence of decreased renal function in geriatric population (see Geriatric Patients under Dosage and Administration).
Renal Impairment
Increased risk of severe bone marrow depression in patients with renal impairment; monitor renal function carefully. Clcr appears to most accurately reflect kidney function in patients receiving carboplatin.
Reduce dosage in patients with renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
Thrombocytopenia, neutropenia, leukopenia, anemia, nausea, vomiting, electrolyte abnormalities (hypocalcemia, hypokalemia, hypomagnesemia, hyponatremia), alkaline phosphatase elevations.
Drug Interactions
Ototoxic Drugs
Hearing loss reported in children receiving carboplatin at higher than recommended doses in combination with other ototoxic drugs.
Nephrotoxic Drugs
Possible potentiation of renal effects.
Emetogenic Drugs
Concomitant use with emetogenic drugs or use in individuals who previously received emetogenic therapy is associated with an increased incidence of emesis.
Specific Drugs and Therapies
|
Drug or Therapy |
Interaction |
Comments |
|---|---|---|
|
Aminoglycosides |
Increased risk of nephrotoxicity and/or ototoxicity |
Use with caution |
|
Antineoplastic agents |
Prior antineoplastic therapy may increase risk of bone marrow suppression |
|
|
Myelosuppressive agents |
Possible potentiation of hematologic toxicity |
Monitor carefully; manage dosage and time of administration to minimize additive toxic effects |
|
Radiation therapy |
Possible potentiation of hematologic toxicity |
Monitor carefully; manage dosage and time of administration to minimize additive toxic effects |
Carboplatin Pharmacokinetics
Complex pharmacokinetics involve the parent compound as well as total platinum (protein-bound and nonprotein-bound platinum) and ultrafilterable platinum (carboplatin and nonprotein-bound carboplatin metabolites).
Absorption
Bioavailability
Following IV infusion, peak plasma concentrations of carboplatin, total platinum, and ultrafilterable platinum occur immediately.
Following intraperitoneal administration†, peak plasma concentrations of total platinum, free platinum, and carboplatin are attained within 2–4 hours following instillation.
Distribution
Extent
Widely distributed into body tissues and fluids, with highest concentrations in the kidney, liver, skin, and tumor tissue; lower concentrations found in fat and brain. Also distributed into erythrocytes.
Not known whether carboplatin or its platinum-containing products cross the placenta or are distributed into milk.
Plasma Protein Binding
Carboplatin is not bound to plasma proteins, but degrades to platinum-containing products which rapidly bind to protein.
<24% of platinum is bound to plasma proteins during the first 4 hours after IV administration of carboplatin; within 24 hours, 87% is protein bound.
Elimination
Metabolism
Metabolic fate has not been completely elucidated. No evidence to date that the drug undergoes enzymatic biotransformation; the bidentate dicarboxylate ligands of carboplatin are believed to be displaced by water, forming positively charged platinum complexes that react with nucleophilic sites on DNA.
Elimination Route
Carboplatin and its platinum-containing product(s) are excreted principally in urine (predominantly via glomerular filtration).
Carboplatin (as ultrafilterable carboplatin) is removed extensively by hemodialysis.
Half-life
Plasma elimination half-lives (t½β) for carboplatin and ultrafilterable platinum: 2–3 hours.
Terminal elimination half-life (t½γ) for total platinum: 4–6 days.
Special Populations
In patients with impaired renal function, renal clearance and total body clearance of platinum are reduced. In patients undergoing hemodialysis, t½β values for total and ultrafilterable platinum are increased compared with values in individuals with normal renal function.
Stability
Storage
Parenteral
Injection Concentrate
25°C (may be exposed to 15–30°C). Protect from light.
Discard unused solution 14 days after initial entry into vial.
Discard diluted solutions 8 hours after preparation.
Powder for Injection
20–25°C; protect from light.
Reconstituted solutions are stable for 8 hours at room temperature (25°C). Reconstituted solutions contain no preservatives; discard after 8 hours.
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|---|
|
Dextrose 5% in sodium chloride 0.2, 0.45, or 0.9% |
|
Dextrose 5% in water |
|
Sodium chloride 0.9% |
|
Incompatible |
|
Sodium bicarbonate 200 mM/L |
Drug Compatibility
|
Compatible |
|---|
|
Cisplatin |
|
Etoposide |
|
Floxuridine |
|
Ifosfamide |
|
Paclitaxel |
|
Incompatible |
|
Fluorouracil |
|
Mesna |
|
Compatible |
|---|
|
Allopurinol sodium |
|
Amifostine |
|
Anidulafungin |
|
Aztreonam |
|
Caspofungin acetate |
|
Cladribine |
|
Doripenem |
|
Doxorubicin HCl liposome injection |
|
Etoposide phosphate |
|
Filgrastim |
|
Fludarabine phosphate |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Linezolid |
|
Melphalan HCl |
|
Micafungin sodium |
|
Ondansetron HCl |
|
Oxaliplatin |
|
Paclitaxel |
|
Palonosetron HCI |
|
Pemetrexed disodium |
|
Piperacillin sodium–tazobactam sodium |
|
Propofol |
|
Sargramostim |
|
Teniposide |
|
Thiotepa |
|
Topotecan HCl |
|
Vinorelbine tartrate |
|
Incompatible |
|
Amphotericin B cholesteryl sulfate complex |
Actions
-
Appears to exert effects by binding to DNA, thereby inhibiting DNA synthesis; effects are cycle-phase nonspecific. Antineoplastic activity may also involve other mechanisms.
-
Must undergo activation before antineoplastic activity occurs. Both carboplatin and cisplatin are activated by an initial aquation reaction, but carboplatin is a more stable compound and is activated more slowly than cisplatin.
Higher concentrations of carboplatin than cisplatin are required to produce equivalent levels of DNA binding. At concentrations that produce equivalent levels of DNA binding, both drugs induce equal numbers of drug-DNA cross-links, resulting in equivalent lesions and biologic activity. Antitumor activity of carboplatin in mice is comparable to or slightly less than that of cisplatin.
-
Further study needed to fully elucidate the extent of cross-resistance between cisplatin and carboplatin. Although some cisplatin-refractory tumors may respond to carboplatin, a high degree of cross-resistance appears to occur between the drugs.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed; necessity for clinicians to advise women to avoid pregnancy during therapy. Advise pregnant women of risk to the fetus.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection, concentrate, for IV infusion |
10 mg/mL (50, 150, 450, or 600 mg)* |
CARBOplatin for Injection |
|
|
Paraplatin |
Bristol-Myers Squibb |
|||
|
For injection, for IV infusion |
50 mg* |
CARBOplatin for Injection |
||
|
Paraplatin |
Bristol-Myers Squibb |
|||
|
150 mg* |
CARBOplatin for Injection |
|||
|
Paraplatin |
Bristol-Myers Squibb |
|||
|
450 mg* |
CARBOplatin for Injection |
|||
|
Paraplatin |
Bristol-Myers Squibb |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 18, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Why give Taxol (Paxel) before carboplatin?
- How soon can you start chemo after port placement?
- Radiation vs. Chemo: Which cancer treatment is right for you?
- What is chemo brain and how long does it last?
- What is TCHP chemotherapy and how is it used?
- How does carboplatin stop cancer?
- Does carboplatin cause neuropathy?
More about carboplatin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: alkylating agents
- Breastfeeding
- En español