Ampicillin (Monograph)
Drug class: Aminopenicillins
Chemical name: [2S-[2α,5α,6β(S*)]]-6-[(Aminophenylacetyl)amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0]heptane-2-carboxylic acid
Molecular formula: C16H19N3O4SC16H19N3O4S•NaC16H19N3O4S•3H2O
CAS number: 69-53-4
Introduction
Antibacterial; β-lactam antibiotic; aminopenicillin.
Uses for Ampicillin
Endocarditis
Treatment of enterococcal endocarditis; used in conjunction with an aminoglycoside.
Treatment of endocarditis caused by susceptible staphylococci, streptococci, E. coli, P. mirabilis, or Salmonella.
For treatment of endocarditis caused by Enterococcus faecalis, E. faecium, or other enterococci susceptible to penicillin and gentamicin, AHA states IV penicillin G (or IV ampicillin) in conjunction with gentamicin is a regimen of choice; streptomycin can be substituted for gentamicin if enterococci are susceptible to penicillin and streptomycin, but resistant to gentamicin.
For treatment of endocarditis caused by viridans group streptococci† [off-label] or nonenterococcal group D streptococci† [off-label], including Streptococcus gallolyticus† [off-label] (formerly S. bovis), AHA states that IV ampicillin is a reasonable alternative to IV penicillin G. May be used alone if caused by highly penicillin-susceptible strains (penicillin MIC ≤0.12 mcg/mL); use in conjunction with gentamicin if strains are relatively resistant (penicillin MIC >0.12 mcg/mL but <0.5 mcg/mL).
Because fastidious gram-negative bacilli of the HACEK group† [off-label] (i.e., Haemophilus, Aggregatibacter, Cardiobacterium hominis, Eikenella corrodens, Kingella) resistant to penicillins are being reported with increasing frequency, AHA states that IV ampicillin (with or without an aminoglycoside) should be used for the treatment of endocarditis caused by these organisms only if in vitro susceptibility is confirmed.
Consult current guidelines from AHA for information on management of endocarditis.
Prevention of α-hemolytic (viridans group) streptococcal bacterial endocarditis† [off-label] in patients undergoing certain dental procedures (i.e., procedures that involve manipulation of gingival tissue or periapical region of teeth or perforation of oral mucosa) or certain invasive respiratory tract procedures (i.e., procedures involving incision or biopsy of respiratory mucosa) who have certain cardiac conditions that put them at highest risk of adverse outcomes from endocarditis. AHA recommends oral amoxicillin as drug of choice; ampicillin is an alternative in those unable to take oral medication.
Consult most recent AHA recommendations for information on which cardiac conditions are associated with highest risk of adverse outcomes from endocarditis and specific recommendations regarding use of prophylaxis to prevent endocarditis in these patients.
Meningitis and Other CNS Infections
Treatment of meningitis caused by susceptible Neisseria meningitidis, Streptococcus agalactiae (group B streptococci; GBS), Listeria monocytogenes, E. coli, or H. influenzae†.
A drug of choice for empiric treatment of neonatal S. agalactiae meningitis; consider concomitant use of an aminoglycoside.
A drug of choice for L. monocytogenes meningitis; used alone or in conjunction with an aminoglycoside (e.g., gentamicin).
Respiratory Tract Infections
Treatment of respiratory tract infections caused by susceptible Staphylococcus aureus (including penicillinase-producing strains), Streptococcus (including S. pneumoniae), S. pyogenes (group A β-hemolytic streptococci), or H. influenzae (nonpenicillinase-producing strains only).
Generally should not be used for the treatment of streptococcal or staphylococcal infections when a natural penicillin would be effective. Should not be used alone for empiric treatment of respiratory tract infections when ampicillin-resistant H. influenzae may be involved.
Septicemia
Treatment of septicemia caused by susceptible staphylococci, streptococci, enterococci, E. coli, P. mirabilis, or Salmonella.
Urinary Tract Infections (UTIs)
Treatment of UTIs caused by susceptible enterococci, E. coli, or Proteus mirabilis.
A drug of choice for enterococcal UTIs. Because of high urinary concentrations, may be effective when used alone, but consider that enterococci resistant to ampicillin have been reported.
Eikenella Infections
Treatment of infections caused by Eikenella corrodens†; drug of choice.
Listeria Infections
Treatment of infections caused by Listeria monocytogenes; used alone or in conjunction with an aminoglycoside.
A drug of choice for Listeria infections occurring during pregnancy, granulomatosis infantiseptica, sepsis, endocarditis, meningitis, and foodborne infections. (See Meningitis and Other CNS Infections under Uses.)
Pertussis
Has been used to treat and prevent secondary pulmonary infections in patients with pertussis†. Erythromycin generally considered drug of choice for treatment of catarrhal stage of pertussis and to shorten the period of communicability of the disease. Ampicillin, like most other anti-infectives, does not shorten clinical course of pertussis.
Typhoid Fever and Other Salmonella Infections
Alternative for treatment of typhoid fever (enteric fever) caused by susceptible Salmonella typhi. Drugs of choice are third generation cephalosporins (e.g., ceftriaxone, cefotaxime) or fluoroquinolones (e.g., ciprofloxacin, ofloxacin); consider that multidrug-resistant strains of S. typhi (strains resistant to ampicillin, amoxicillin, chloramphenicol, and/or co-trimoxazole) reported with increasing frequency.
Treatment of chronic carriers of S. typhi†; drugs of choice are fluoroquinolones (e.g., ciprofloxacin), ampicillin, or amoxicillin (with probenecid).
Treatment of gastroenteritis caused by susceptible Salmonella.
Shigella Infections
Treatment of GI infections caused by susceptible Shigella.
Anti-infectives generally indicated in addition to fluid and electrolyte replacement for severe shigellosis. Previously considered a drug of choice for shigellosis (especially in children), but strains of S. flexneri and S. sonnei resistant to ampicillin reported with increasing frequency. Fluoroquinolones, ceftriaxone, or co-trimoxazole now considered drugs of choice for empiric treatment, especially in areas where ampicillin-resistant strains of Shigella have been reported.
Prevention of Perinatal Group B Streptococcal Disease
Prevention of early-onset neonatal group B streptococcal (GBS) disease†.
ACOG, AAP, and others recommend routine universal prenatal screening for GBS colonization (e.g., vaginal and rectal cultures) in all pregnant women at 36 through 37 weeks of gestation (i.e., performed within the time period of 36 weeks 0 days to 37 weeks 6 days of gestation), unless intrapartum anti-infective prophylaxis already planned because the woman had known GBS bacteriuria during any trimester of current pregnancy or has history of a previous infant with GBS disease. Anti-infective prophylaxis for prevention of early-onset perinatal GBS indicated in all women identified as having positive GBS cultures during routine prenatal GBS screening during current pregnancy, unless a cesarean delivery is performed before onset of labor in the setting of intact membranes. Also indicated in women with unknown GBS status at time of onset of labor (cultures not performed or results unknown) who have risk factors for perinatal GBS infection (e.g., preterm birth at <37 weeks’ gestation, duration of membrane rupture ≥18 hours, intrapartum fever ≥38°C).
IV penicillin G is drug of choice and IV ampicillin is preferred alternative for intrapartum GBS anti-infective prophylaxis. Penicillin G has a narrower spectrum of activity and is less likely to select for antibiotic-resistant organisms.
Regardless of whether the mother received anti-infective prophylaxis, initiate appropriate diagnostic evaluations and anti-infective therapy in the neonate if signs or symptoms of active infection develop.
Consult current ACOG guidelines available at [Web] for additional information regarding prevention of neonatal early-onset GBS disease.
Ampicillin Dosage and Administration
Administration
Administer orally, by slow IV injection or infusion, or by IM injection.
Oral Administration
Administer orally with a full glass of water 1 hour before or 2 hours after meals.
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Reconstitution
Reconstitute vials containing 125, 250, or 500 mg with 5 mL of sterile or bacteriostatic water for injection. Alternatively, reconstitute vials containing 1 or 2 g with 7.4 or 14.8 mL, respectively, of sterile or bacteriostatic water for injection.
Rate of Administration
Solutions reconstituted from 125-, 250-, or 500-mg vials may be given by IV injection over a period of 3–5 minutes. Solutions reconstituted from 1- or 2-g vials should be given IV over a period of ≥10–15 minutes.
For IV infusion, concentration and rate of administration should be adjusted so that the total dose is administered before the drug is inactivated in the IV solution.
IM Administration
Reconstitution
Reconstitute with sterile or bacteriostatic water for injection according to manufacturer’s directions to provide solutions containing 125 or 250 mg/mL.
Dosage
Available as ampicillin trihydrate and ampicillin sodium ; dosage expressed in terms of ampicillin.
Duration of therapy depends on type and severity of infection and should be determined by clinical and bacteriologic response of the patient. For most infections, therapy should be continued for ≥48–72 hours after patient becomes asymptomatic or evidence of eradication of the infection has been obtained. More prolonged therapy may be necessary for some infections.
Pediatric Patients
General Pediatric Dosage
Oral
Children beyond neonatal age with mild to moderate infections: AAP recommends 50–100 mg/kg daily given in 4 divided doses.
Children beyond neonatal age with severe infections: AAP states oral route inappropriate.
IV or IM
Neonates <7 days of age: AAP recommends 50 mg/kg every 12 hours in those weighing ≤2 kg or 50 mg/kg every 8 hours in those weighing >2 kg. Higher dosage may be needed for treatment of meningitis.
Neonates 8–28 days of age: AAP recommends 50 mg/kg every 8 hours in those weighing ≤2 kg or 50 mg/kg every 6 hours in those weighing >2 kg. Higher dosage may be needed for treatment of meningitis.
Children beyond neonatal age: AAP recommends 100–150 mg/kg daily given in 4 divided doses for mild to moderate infections or 200–400 mg/kg daily given in 4 divided doses for severe infections. Use highest dosage for treatment of CNS infections.
Endocarditis
Treatment of Endocarditis Caused by Viridans Streptococci or S. bovis
IV200–300 mg/kg daily (up to 12 g daily) given in 4–6 divided doses for 4 weeks. Used in conjunction with IM or IV gentamicin.
Treatment of Enterococcal Endocarditis
IV200–300 mg/kg daily (up to 12 g daily) given in 4–6 divided doses for 4–6 weeks. Used in conjunction with IM or IV gentamicin.
Prevention of Bacterial Endocarditis in Patients Undergoing Certain Dental or Respiratory Tract Procedures†
IV or IM50 mg/kg as a single dose given 30–60 minutes prior to the procedure.
GI Infections
Oral
Children weighing ≤20 kg: 100 mg/kg daily in 4 divided doses.
Children weighing >20 kg: 500 mg 4 times daily. Severe or chronic infections may require higher dosage.
IV or IM
Children weighing <40 kg: 50 mg/kg daily in divided doses every 6–8 hours.
Children weighing ≥40 kg: 500 mg every 6 hours. Severe or chronic infections may require higher dosage.
Meningitis and Other CNS Infections
Empiric Treatment of Meningitis
IVNeonates and children <2 months of age: 100–300 mg/kg daily given in divided doses; with or without gentamicin.
Children 2 months to 12 years of age: 200–400 mg/kg daily given in divided doses every 4–6 hours; used in conjunction with IV chloramphenicol.
Treatment of Meningitis Caused by S. agalactiae (GBS)
IVNeonates: AAP recommends 200–300 mg/kg daily given in 3 divided doses in those ≤7 days of age or 300 mg/kg daily given in 4 divided doses in those >7 days of age.
Neonates ≤28 days of age: Some experts recommend 75 mg/kg every 6 hours, regardless of weight.
Respiratory Tract Infections
Oral
Children weighing ≤20 kg: 50 mg/kg daily in 3 or 4 divided doses.
Children weighing >20 kg: 250 mg 4 times daily.
IV or IM
Children weighing <40 kg: 25–50 mg/kg daily in divided doses every 6–8 hours.
Children weighing ≥40 kg: 250–500 mg every 6 hours.
Septicemia
IV or IM
150–200 mg/kg daily.
Skin and Skin Structure Infections
IV or IM
Children weighing <40 kg: 25–50 mg/kg daily in divided doses every 6–8 hours.
Children weighing ≥40 kg: 250–500 mg every 6 hours.
Urinary Tract Infections (UTIs)
Oral
Children weighing ≤20 kg: 100 mg/kg daily in 4 divided doses.
Children weighing >20 kg: 500 mg 4 times daily. Severe or chronic infections may require higher dosage.
IV or IM
Children weighing <40 kg: 50 mg/kg daily in divided doses every 6–8 hours.
Children weighing ≥40 kg: 500 mg every 6 hours. Severe or chronic infections may require higher dosage.
Adults
Endocarditis
Treatment of Enterococcal Endocarditis
IV2 g every 4 hours in conjunction with IM or IV gentamicin. Treatment with both drugs generally should be continued for 4–6 weeks, but patients who had symptoms of infection for >3 months before treatment was initiated and patients with prosthetic heart valves require ≥6 weeks of therapy with both drugs.
Treatment of Endocarditis Caused by HACEK group (i.e., Haemophilus, Aggregatibacter, Cardiobacterium hominis, Eikenella corrodens, Kingella)†
IV2 g every 12 hours.
Prevention of Bacterial Endocarditis in Patients Undergoing Certain Dental or Respiratory Tract Procedures†
IV or IM2 g as a single dose given 30–60 minutes prior to the procedure.
GI Infections
Oral
500 mg 4 times daily.
IV or IM
Adults weighing <40 kg: 50 mg/kg daily in divided doses every 6–8 hours.
Adults weighing ≥40 kg: 500 mg every 6 hours.
Meningitis and Other CNS Infections
IV, then IM
150–200 mg/kg daily in divided doses every 3–4 hours. Use IV initially, may switch to IM after 3 days.
Respiratory Tract Infections
Oral
250 mg 4 times daily.
IV or IM
Adults weighing <40 kg: 25–50 mg/kg daily in divided doses every 6–8 hours.
Adults weighing ≥40 kg: 250–500 mg every 6 hours.
Septicemia
IV or IM
150–200 mg/kg daily.
Skin and Skin Structure Infections
IV or IM
Adults weighing <40 kg: 25–50 mg/kg daily in divided doses every 6–8 hours.
Adults weighing ≥40 kg: 250–500 mg every 6 hours.
Urinary Tract Infections (UTIs)
Oral
500 mg 4 times daily.
IV or IM
Adults weighing <40 kg: 50 mg/kg daily in divided doses every 6–8 hours.
Adults weighing ≥40 kg: 500 mg every 6 hours.
Prevention of Perinatal Group B Streptococcal (GBS) Disease†
IV
An initial 2-g dose (at time of labor or rupture of membranes) followed by 1 g every 4 hours until delivery.
Prescribing Limits
Pediatric Patients
Pediatric dosage should not exceed adult dosage.
Special Populations
Renal Impairment
Dosage adjustments necessary in patients with renal impairment.
Some clinicians suggest that adults with GFR 10–50 mL/minute receive the usual dose every 6–12 hours and that adults with GFR <10 mL/minute receive the usual dose every 12–16 hours. Alternatively, some clinicians suggest that modification of usual dosage is unnecessary in adults with Clcr ≥ 30 mL/minute, but that adults with Clcr ≤10 mL/minute should receive the usual dose every 8 hours.
Patients undergoing hemodialysis should receive a supplemental dose after each dialysis period.
Geriatric Patients
No dosage adjustments except those related to renal impairment. (See Renal Impairment under Dosage and Administration.)
Cautions for Ampicillin
Contraindications
-
Known hypersensitivity to any penicillin.
Warnings/Precautions
Warnings
Superinfection/Clostridioides difficile-associated Colitis
Possible emergence and overgrowth of nonsusceptible bacteria or fungi. Discontinue and institute appropriate therapy if superinfection occurs.
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of C. difficile. C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives and may range in severity from mild diarrhea to fatal colitis. Consider CDAD if diarrhea develops during or after therapy and manage accordingly.
If CDAD suspected or confirmed, discontinue anti-infectives not directed against C. difficile as soon as possible. Initiate appropriate anti-infective therapy directed against C. difficile (e.g., fidaxomicin, vancomycin, metronidazole), appropriate supportive therapy (e.g., fluid and electrolyte management, protein supplementation), and surgical evaluation as clinically indicated.
Sensitivity Reactions
Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity reactions, including anaphylaxis, reported with penicillins.
Prior to initiation of therapy, make careful inquiry regarding previous hypersensitivity reactions to penicillins, cephalosporins, or other drugs. Partial cross-allergenicity occurs among penicillins and other β-lactam antibiotics including cephalosporins and cephamycins.
If a severe hypersensitivity reaction occurs, discontinue immediately and institute appropriate therapy as indicated (e.g., epinephrine, corticosteroids, maintenance of an adequate airway and oxygen).
General Precautions
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of ampicillin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing. In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.
Mononucleosis
Possible increased risk of rash in patients with mononucleosis; use in these patients not recommended.
Ampicillin-resistant Haemophilus influenzae
Because of increasing prevalence of ampicillin-resistant H. influenzae, the drug should not be used alone for empiric treatment of serious infections (e.g., meningitis, pneumonia) when H. influenzae may be involved.
Laboratory Monitoring
Periodically assess organ system functions, including renal, hepatic, and hematopoietic, during prolonged therapy.
Sodium Content
Powder for injection contains 2.9 mEq of sodium per g of ampicillin.
Specific Populations
Pregnancy
Category B.
Lactation
Distributed into milk. Use with caution.
Pediatric Use
Renal clearance of ampicillin may be delayed in neonates and young infants because of incompletely developed renal function. Use lowest effective dosage.
Renal Impairment
Dosage adjustments necessary in renal impairment. (See Renal Impairment under Dosage and Administration.)
Common Adverse Effects
GI effects (diarrhea, nausea), rash.
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Allopurinol |
Possible increased incidence of rash |
Clinical importance has not been determined; some clinicians suggest that concomitant use of the drugs should be avoided if possible |
|
Aminoglycosides |
In vitro evidence of synergistic antibacterial effects against enterococci; used to therapeutic advantage in treatment of endocarditis and other severe enterococcal infections Potential in vitro and in vivo inactivation of aminoglycosides |
|
|
Chloramphenicol |
In vitro evidence of antagonism |
Clinical importance unclear |
|
Hormonal contraceptives |
Possible decreased efficacy of estrogen-containing oral contraceptives and increased incidence of breakthrough bleeding |
Some clinicians suggest that a supplemental method of contraception be used in patients receiving oral contraceptives and ampicillin concomitantly, other clinicians state that most women taking oral contraceptives probably do not need to use alternative contraceptive precautions while receiving ampicillin |
|
Methotrexate |
Possible decreased renal clearance of methotrexate with penicillins; possible increased methotrexate concentrations and hematologic and GI toxicity |
Monitor closely if used concomitantly |
|
Probenecid |
Decreased renal tubular secretion of ampicillin; increased and prolonged ampicillin concentrations may occur |
|
|
Sulbactam |
Synergistic bactericidal effect against many strains of β-lactamase-producing bacteria |
|
|
Sulfonamides |
In vitro evidence of antagonism |
Clinical importance unclear |
|
Tests for glucose |
Possible false-positive reactions in urine glucose tests using Clinitest, Benedict’s solution, or Fehling’s solution |
Use glucose tests based on enzymatic glucose oxidase reactions (e.g., Clinistix, Tes-Tape) |
|
Tests for uric acid |
Possible falsely increased serum uric acid concentrations when copper-chelate method is used; phosphotungstate and uricase methods appear to be unaffected by the ampicillin |
Ampicillin Pharmacokinetics
Absorption
Bioavailability
30–55% of an oral dose absorbed from the GI tract in fasting adults; peak serum concentrations attained within 1–2 hours.
Following IM administration, peak serum concentrations generally attained more quickly and are higher than following equivalent oral doses.
Food
Food generally decreases rate and extent of absorption.
Distribution
Extent
Distributed into ascitic, synovial, and pleural fluids. Also distributed into liver, lungs, gallbladder, prostate, muscle, middle ear effusions, bronchial secretions, maxillary sinus secretions. and tonsils.
Distributed into CSF in concentrations 11–65% of simultaneous serum concentrations; highest CSF concentrations occur 3–7 hours after an IV dose.
Readily crosses the placenta. Distributed into milk in low concentrations.
Plasma Protein Binding
15–25%.
Protein binding is lower in neonates than in children or adults; ampicillin reportedly 8–12% bound to serum proteins in neonates.
Elimination
Metabolism
Partially metabolized by hydrolysis of the β-lactam ring to penicilloic acid which is microbiologically inactive.
Elimination Route
Eliminated in urine by renal tubular secretion and to a lesser extent by glomerular filtration. Small amounts also excreted in feces and bile.
In adults with normal renal function, approximately 20–64% of a single oral dose excreted unchanged in urine within 6–8 hours. Approximately 60–70% of a single IM dose or 73–90% of a single IV dose excreted unchanged in urine.
Half-life
0.7–1.5 hours in adults with normal renal function.
Half-life is 4 hours in neonates 2–7 days of age, 2.8 hours in neonates 8–14 days of age, and 1.7 hours in neonates 15–30 days of age.
Special Populations
Serum concentrations higher and more prolonged in premature or full-term neonates <6 days of age than in full-term neonates ≥6 days of age.
Renal clearance decreased in geriatric patients because of diminished tubular secretory ability; serum concentrations may be higher and half-life prolonged. In those 67–76 years of age, half-life ranges from 1.4–6.2 hours.
Serum concentrations are higher and half-life prolonged in patients with impaired renal function. Half-life may range from 7.4–21 hours in patients with Clcr <10 mL/minute.
Stability
Storage
Oral
Capsules
Tight container at 15–30°C; avoid excessive heat.
For Suspension
Tight container at 15–30°C. After reconstitution, discard after 7 days if stored at room temperature or after 14 days if refrigerated.
Parenteral
Powder for Injection or Infusion
Solutions for IM injection or IV injection or infusion should be used within 1 hour after reconstitution and should not be frozen.
Compatibility
Parenteral
Solution CompatibilityHID
|
Compatible |
|---|
|
Isolyte M or P with dextrose 5% |
|
Incompatible |
|
Amino acids 4.25%, dextrose 25% |
|
Dextran 40 10% in sodium chloride 0.9% |
|
Dextran 40 10% in dextrose 5% in water |
|
Dextrose 5% in sodium chloride 0.45 or 0.9% |
|
Dextrose 5 or 10% in water |
|
Fat emulsion 10%, IV |
|
Fructose 5.25% |
|
Hetastarch 6% in sodium chloride 0.9% |
|
Ringer’s injection, lactated |
|
Sodium bicarbonate 1.4% |
|
Sodium lactate (1/6) M |
|
Variable |
|
Ringer’s injection |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Clindamycin phosphate |
|
Erythromycin lactobionate |
|
Furosemide |
|
Lincomycin HCl |
|
Metronidazole |
|
Incompatible |
|
Amikacin sulfate |
|
Chlorpromazine HCl |
|
Dopamine HCl |
|
Gentamicin sulfate |
|
Hetastarch in sodium chloride 0.9% |
|
Hydralazine HCl |
|
Prochlorperazine mesylate |
|
Variable |
|
Aztreonam |
|
Cefepime HCl |
|
Heparin sodium |
|
Hydrocortisone sodium succinate |
|
Ranitidine HCl |
|
Verapamil HCl |
|
Compatible |
|---|
|
Acyclovir sodium |
|
Alprostadil |
|
Amifostine |
|
Anidulafungin |
|
Aztreonam |
|
Bivalirudin |
|
Cyclophosphamide |
|
Dexmedetomidine HCl |
|
Docetaxel |
|
Doxapram HCl |
|
Doxorubicin HCl liposome injection |
|
Enalaprilat |
|
Esmolol HCl |
|
Etoposide phosphate |
|
Famotidine |
|
Filgrastim |
|
Fludarabine phosphate |
|
Foscarnet sodium |
|
Gemcitabine HCl |
|
Granisetron HCl |
|
Heparin sodium |
|
Heparin sodium with hydrocortisone sodium succinate |
|
Hetastarch in lactated electrolyte injection (Hextend) |
|
Hydroxyethyl starch 130/0.4 in sodium chloride 0.9% |
|
Insulin, regular |
|
Labetalol HCl |
|
Levofloxacin |
|
Linezolid |
|
Magnesium sulfate |
|
Melphalan HCl |
|
Meperidine HCl |
|
Milrinone lactate |
|
Morphine sulfate |
|
Multivitamins |
|
Pantoprazole sodium |
|
Pemetrexed disodium |
|
Phytonadione |
|
Potassium chloride |
|
Propofol |
|
Remifentanil HCl |
|
Tacrolimus |
|
Teniposide |
|
Theophylline |
|
Thiotepa |
|
Incompatible |
|
Amphotericin B cholesteryl sulfate complex |
|
Caspofungin acetate |
|
Epinephrine HCl |
|
Fenoldopam mesylate |
|
Fluconazole |
|
Hydralazine HCl |
|
Midazolam HCl |
|
Nicardipine HCl |
|
Ondansetron HCl |
|
Sargramostim |
|
Verapamil HCl |
|
Vinorelbine tartrate |
|
Variable |
|
Calcium gluconate |
|
Cisatracurium besylate |
|
Diltiazem HCl |
|
Hetastarch in sodium chloride 0.9% |
|
Hydromorphone HCl |
|
Vancomycin HCl |
Actions and Spectrum
-
Based on spectrum of activity, classified as an aminopenicillin. Aminopenicillins have enhanced activity against gram-negative bacteria compared with natural and penicillinase-resistant penicillins.
-
Usually bactericidal.
-
Like other β-lactam antibiotics, antibacterial activity results from inhibition of bacterial cell wall synthesis.
-
Spectrum of activity includes many gram-positive and -negative aerobes and some anaerobes.
-
Gram-positive aerobes: active in vitro and in clinical infections against Staphylococcus (β-lactamase-negative strains only), Streptococcus pneumoniae, other Streptococcus (α- and β-hemolytic strains only), and Enterococcus faecalis. Also active against Corynebacteriun and Listeria monocytogenes.
-
Gram-negative aerobes: active in vitro and in clinical infections against H. influenzae, N. gonorrhoeae, E. coli, Proteus mirabilis, Salmonella, and Shigella. Also active in vitro against Bordetella pertussis, Eikenella corrodens, and Neisseria meningitidis. Inactive against Citrobacter, Enterobacter, Klebsiella, Providencia, and Serratia.
-
Gram-positive and gram-negative bacteria that produce β-lactamases, including β-lactamase-producing S. aureus and E. faecalis, are resistant.
-
Complete cross-resistance generally occurs between ampicillin and amoxicillin.
Advice to Patients
-
Advise patients that antibacterials (including ampicillin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).
-
Importance of completing the entire prescribed course of treatment, even if feeling better after a few days.
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with ampicillin or other antibacterials in the future.
-
Importance of taking oral ampicillin with a full glass of water 1 hour before or 2 hours after a meal.
-
Importance of discontinuing therapy and informing clinician if an allergic reaction occurs.
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
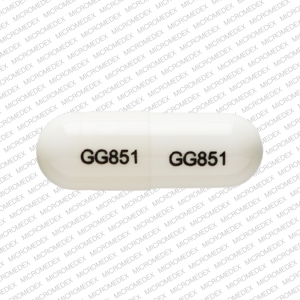
Oral |
Capsules |
250 mg (of ampicillin)* |
Ampicillin Capsules |
|
|
500 mg (of ampicillin)* |
Ampicillin Capsules |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Parenteral |
For injection |
125 mg (of ampicillin)* |
Ampicillin Sodium for Injection |
|
|
250 mg (of ampicillin)* |
Ampicillin Sodium for Injection |
|||
|
500 mg (of ampicillin)* |
Ampicillin Sodium for Injection |
|||
|
1 g (of ampicillin)* |
Ampicillin Sodium for Injection |
|||
|
2 g (of ampicillin)* |
Ampicillin Sodium for Injection |
|||
|
10 g (of ampicillin) pharmacy bulk package* |
Ampicillin Sodium for Injection |
|||
|
For injection, for IV infusion |
1 g (of ampicillin)* |
Ampicillin Sodium ADD-Vantage |
||
|
Ampicillin Sodium Piggyback |
||||
|
2 g (of ampicillin)* |
Ampicillin Sodium ADD-Vantage |
|||
|
Ampicillin Sodium Piggyback |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 2, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about ampicillin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: aminopenicillins
- Breastfeeding