Ibrutinib (Monograph)
Brand name: Imbruvica
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; inhibitor of Bruton's tyrosine kinase (BTK).
Uses for Ibrutinib
Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL)
Used for the treatment of CLL and SLL, including CLL/SLL harboring the 17p13.1 deletion (17p deletion) chromosomal abnormality; designated an orphan drug by FDA for this use.
National Cancer Institute guidelines on CLL in patients with symptomatic or progressive disease include the use of BTK inhibitors, including ibrutinib, among first-line agents.
Waldenstrom's Macroglobulinemia (WM)
Used for the treatment of Waldenstrom's macroglobulinemia (WM); designated an orphan drug by FDA for this use.
Based on consensus statements, first-line therapy options for treatment-naïve, symptomatic patients include chemoimmunotherapy, ibrutinib alone or plus rituximab, or zanubrutinib. For patients with relapsed or refractory disease, selection of therapy depends on initial treatment used and can include chemoimmunotherapy and/or a covalent BTK inhibitor (e.g., acalabrutinib, ibrutinib, or zarubrutinib).
Graft-versus-host Disease (GVHD)
Treatment of chronic GVHD following failure of ≥1 prior systemic therapy in adults and pediatric patients ≥1 year of age; designated an orphan drug by FDA for this use.
Ibrutinib Dosage and Administration
General
Pretreatment Screening
-
Assess cardiac history and cardiac function at baseline.
-
Assess baseline risk for tumor lysis syndrome.
-
Verify pregnancy status in females of reproductive potential.
-
Evaluate bilirubin and transaminases at baseline.
Patient Monitoring
-
Monitor CBCs monthly.
-
Monitor for signs and symptoms of bleeding. Concomitant use of antiplatelet or anticoagulant therapy increases risk of major hemorrhage.
-
Monitor for signs and symptoms of infection, including fever.
-
Monitor patients for symptoms of cardiac arrhythmias and cardiac failure.
-
Monitor blood pressure.
-
Monitor for tumor lysis syndrome.
-
Monitor bilirubin and transaminases. Monitor more frequently for patients who develop abnormal liver tests and clinical signs and symptoms of hepatotoxicity during therapy.
Premedication and Prophylaxis
-
Consider anti-infective prophylaxis in patients at increased risk of opportunistic infections.
Other General Considerations
-
Consider the potential benefits and risks of withholding ibrutinib therapy for ≥3–7 days prior to and following surgery (based on the type of surgery and bleeding risk).
Administration
Oral Administration
Available as immediate-release capsules containing 70 mg or 140 mg; immediate-release tablets containing 140 mg, 280 mg, or 420 mg; and as immediate-release oral suspension containing 70 mg of ibrutinib per mL.
Administer orally once daily at approximately the same time each day.
Swallow capsules whole with a glass of water; do not open, break, or chew.
Swallow tablets whole with a glass of water; do not cut, crush, or chew.
Refer to full instructions for use in the prescribing information for details on administration of the oral suspension.
If a dose is missed, administer missed dose on the same day as soon as it is remembered and resume normal schedule the following day; do not take extra doses on the same day to make up for a missed dose.
Dosage
Pediatric Patients
Chronic Graft-versus-host Disease (GVHD)
<E> Oral
Children ≥12 years of age: 420 mg once daily.
Children 1 to <12 years of age: 240 mg/m2 once daily (up to a dose of 420 mg). Refer to Table 1 for recommended dosage to achieve 240 mg/m2 based on body surface area (BSA).
Continue therapy until progression of chronic GVHD, recurrence of underlying malignancy, or unacceptable toxicity occurs. Discontinue therapy when treatment for chronic GVHD no longer necessary.
|
BSA (m2) range |
Dose (mg) of ibrutinib capsules or tablets to administer |
Volume (mL) of ibrutinib oral suspension to administer |
|---|---|---|
|
>0.3–0.4 |
1.2 mL |
|
|
>0.4–0.5 |
1.5 mL |
|
|
>0.5–0.6 |
1.9 mL |
|
|
>0.6–0.7 |
2.2 mL |
|
|
>0.7–0.8 |
210 mg |
2.6 mL |
|
>0.8–0.9 |
210 mg |
2.9 mL |
|
>0.9–1 |
210 mg |
3.3 mL |
|
>1–1.1 |
280 mg |
3.6 mL |
|
>1.1–1.2 |
280 mg |
4 mL |
|
>1.2–1.3 |
280 mg |
4.3 mL |
|
>1.3–1.4 |
350 mg |
4.6 mL |
|
>1.4–1.5 |
350 mg |
5 mL |
|
>1.5–1.6 |
350 mg |
5.3 mL |
|
>1.6 |
420 mg |
6 mL |
Adults
Chronic Lymphocytic Leukemia (CLL)/Small Lymphocytic Lymphoma (SLL)
Oral
420 mg once daily (as a single agent, in combination with bendamustine and rituximab, or in combination with rituximab or obinutuzumab). Continue therapy until disease progression or unacceptable toxicity occurs.
Consider administering ibrutinib prior to rituximab or obinutuzumab if administration occurs on the same day.
Waldenstrom's Macroglobulinemia (WM)
Oral
420 mg once daily (as a single agent or in combination with rituximab). Continue therapy until disease progression or unacceptable toxicity occurs.
Consider administering ibrutinib prior to rituximab if administration occurs on the same day.
Dosage adjustment not necessary in patients undergoing plasmapheresis.
Chronic GVHD
Oral
420 mg once daily. Continue therapy until progression of chronic GVHD, recurrence of underlying malignancy, or unacceptable toxicity occurs. Discontinue therapy when treatment for chronic GVHD no longer necessary.
Dosage Modification for Toxicity
Withhold ibrutinib therapy for adverse reactions listed in Table 2. Upon improvement to grade 1 or baseline (recovery), follow recommended dosage modifications described in Table 2.
See Table 3 for dosage modifications based on BSA.
Assess the benefit-risk before resuming treatment.
For grade 4 non-hematologic toxicities, assess the benefit-risk before resuming treatment.
|
Adverse Reaction |
Occurrence |
Dosage Modification for CLL/SLL, WM, and Patients ≥12 Years of Age with Chronic GVHD After Recovery Starting Dose = 420 mg |
Dosage Modification for Patients 1 to <12 Years of Age with Chronic GVHD After Recovery Starting Dose =240 mg/m2 |
|---|---|---|---|
|
Grade 2 cardiac failure |
First |
Restart at 280 mg daily |
Restart at 160 mg/m2 daily |
|
Grade 2 cardiac failure |
Second |
Restart at 140 mg daily |
Restart at 80 mg/m2 daily |
|
Grade 2 cardiac failure |
Third |
Discontinue ibrutinib |
Discontinue ibrutinib |
|
Grade 3 cardiac arrhythmias |
First |
Restart at 280 mg daily |
Restart at 160 mg/m2 daily |
|
Grade 3 cardiac arrhythmias |
Second |
Discontinue ibrutinib |
Discontinue ibrutinib |
|
Grade 3 or 4 cardiac failure, OR Grade 4 cardiac arrhythmias |
First |
Discontinue ibrutinib |
Discontinue ibrutinib |
|
Other grade 3 or 4 nonhematological toxicities, OR Grade 3 or 4 neutropenia with infection or fever, OR Grade 4 hematological toxicities |
First |
Restart at 280 mg daily |
Restart at 160 mg/m2 daily |
|
Other grade 3 or 4 nonhematological toxicitiesv, OR Grade 3 or 4 neutropenia with infection or fever, OR Grade 4 hematological toxicities |
Second |
Restart at 140 mg daily |
Restart at 80 mg/m2 daily |
|
Other grade 3 or 4 nonhematological toxicities, OR Grade 3 or 4 neutropenia with infection or fever, OR Grade 4 hematological toxicities |
Third |
Discontinue ibrutinib |
Discontinue ibrutinib |
|
BSA (m2) range |
Dose (mg) of capsules or tablets to administer to achieve 160 mg/m2 |
Volume (mL) of ibrutinib oral suspension to administer to achieve 160 mg/m2 |
Dose (mg) of capsules or tablets to administer to achieve 80 mg/m2 |
Volume (mL) of ibrutinib oral suspension to administer to achieve 80 mg/m2 |
|---|---|---|---|---|
|
>0.3–0.4 |
0.8 mL |
0.4 mL |
||
|
>0.4–0.5 |
1.3 mL |
0.6 mL |
||
|
>0.6–0.7 |
1.5 mL |
0.7 mL |
||
|
>0.7–0.8 |
140 mg |
1.7 mL |
70 mg |
0.9 mL |
|
>0.8–0.9 |
140 mg |
1.9 mL |
70 mg |
1 mL |
|
>0.9–1 |
140 mg |
2.2 mL |
70 mg |
1.1 mL |
|
>1–1.1 |
140 mg |
2.4 mL |
70 mg |
1.2 mL |
|
>1.1–1.2 |
210 mg |
2.6 mL |
1.3 mL |
|
|
>1.2–1.3 |
210 mg |
2.9 mL |
1.4 mL |
|
|
>1.3–1.4 |
210 mg |
3.1 mL |
1.5 mL |
|
|
>1.4–1.5 |
210 mg |
3.3 mL |
140 mg |
1.7 mL |
|
>1.5–1.6 |
280 mg |
3.5 mL |
140 mg |
1.8 mL |
|
>1.6 |
280 mg |
4 mL |
140 mg |
2 mL |
Dosage Modification for Concomitant Use with CYP3A Inhibitors
Refer to Table 4 for recommended dosage modifications for use of ibrutinib with CYP3A inhibitors. After discontinuation of CYP3A inhibitor, resume previous dosage of ibrutinib.
See Table 3 for dosage modifications based on BSA.
|
Patient Population |
Coadministered Drug |
Recommended Ibrutinib Dosage |
|---|---|---|
|
B-cell malignancies (CLL/SLL or WM) |
Moderate CYP3A inhibitor |
280 mg once daily Modify dosage as recommended for adverse reactions |
|
B-cell malignancies (CLL/SLL or WM) |
Voriconazole 200 mg twice daily Posaconazole suspension 100 mg once daily, 100 mg twice daily, or 200 mg twice daily |
140 mg once daily Modify dosage as recommended for adverse reactions |
|
B-cell malignancies (CLL/SLL or WM) |
Posaconazole suspension 200 mg three times daily or 400 mg twice daily Posaconazole IV 300 mg once daily Posaconazole delayed-release tablets 300 mg once daily |
70 mg once daily Interrupt dosage as recommended for adverse reactions |
|
B-cell malignancies (CLL/SLL or WM) |
Other strong CYP3A inhibitors |
Avoid concomitant use If these inhibitors will be used short-term (e.g., anti-infectives for ≤7 days), interrupt ibrutinib |
|
Patients ≥12 years of age with chronic GVHD |
Moderate CYP3A inhibitor |
420 mg once daily Modify dosage as recommended for adverse reactions |
|
Patients ≥12 years of age with chronic GVHD |
Voriconazole 200 mg twice daily Posaconazole suspension 100 mg once daily, 100 mg twice daily, or 200 mg twice daily |
280 mg once daily Modify dosage as recommended for adverse reactions |
|
Patients ≥12 years of age with chronic GVHD |
Posaconazole suspension 200 mg three times daily or 400 mg twice daily Posaconazole IV 300 mg once daily Posaconazole delayed-release tablets 300 mg once daily |
140 mg once daily Interrupt dosage as recommended for adverse reactions |
|
Patients ≥12 years of age with chronic GVHD |
Other strong CYP3A inhibitors |
Avoid concomitant use If these inhibitors will be used short-term (e.g., anti-infectives for ≤7 days), interrupt ibrutinib |
|
Patients 1 to <12 years of age with chronic GVHD |
Moderate CYP3A inhibitor |
240 mg/m2 once daily Modify dosage as recommended for adverse reactions |
|
Patients 1 to <12 years of age with chronic GVHD |
Voriconazole for suspension 9 mg/kg (maximum dose: 350 mg) twice daily |
160 mg/m2 |
|
Patients 1 to <12 years of age with chronic GVHD |
Posaconazole at any dosage |
80 mg/m2 |
|
Patients 1 to <12 years of age with chronic GVHD |
Other strong CYP3A inhibitors |
Avoid concomitant use If these inhibitors will be used short-term (e.g., anti-infectives for ≤7 days), interrupt ibrutinib |
Special Populations
Hepatic Impairment
Adults with B-cell Malignancies (CLL/SLL or WM)
Mild (Child-Pugh class A) hepatic impairment: Reduce dosage to 140 mg once daily.
Moderate (Child-Pugh class B) hepatic impairment: Reduce dosage to 70 mg once daily.
Severe (Child-Pugh class C) hepatic impairment: Avoid use.
Patients with Chronic GVHD
Patients ≥12 years of age with total bilirubin level >1.5–3 times ULN (unless of non-hepatic origin or due to Gilbert’s syndrome): Recommended dosage of 140 mg once daily.
Patients 1 to <12 years of age with total bilirubin level >1.5–3 times ULN (unless of non-hepatic origin or due to Gilbert’s syndrome): Recommended dosage of ibrutinib dosage of 80 mg/m2 daily.
Total bilirubin level >3 times ULN (unless of non-hepatic origin or due to Gilbert’s syndrome): Avoid use.
Renal Impairment
No specific dosage recommendations at this time.
Geriatric Patients
No specific dosage recommendations at this time; however, certain ibrutinib toxicities may be more frequent in geriatric patients.
Cautions for Ibrutinib
Contraindications
-
None.
Warnings/Precautions
Hemorrhage
Hemorrhagic events, sometimes fatal, observed. Serious (grade 3 or higher) bleeding events, including intracranial hemorrhage, subdural hematoma, GI bleeding, hematuria, and postprocedural hemorrhage, observed.
Increased risk of hemorrhagic events with concomitant use of ibrutinib and antiplatelet or anticoagulant therapies; consider potential benefits and risks of concomitant anticoagulant or antiplatelet therapy. Monitor for manifestations of bleeding.
Consider potential benefits and risks of withholding ibrutinib therapy for ≥3–7 days prior to and following surgery.
Infections
Serious infections (bacterial, viral, or fungal), sometimes fatal, observed.
Progressive leukoencephalopathy and Pneumocystis jirovecii (formerly P. carinii) pneumonia also observed.
Monitor for signs and symptoms of infection and initiate appropriate anti-infective treatment as clinically indicated. Consider prophylaxis according to current standard of care in patients at high risk for opportunistic infections.
Cytopenias
Cytopenias, including thrombocytopenia, anemia, and neutropenia, observed. Serious (grade 3 or 4) cytopenias observed in patients with B-cell malignancies receiving single-agent ibrutinib.
Monitor CBC counts monthly. If myelosuppression occurs, reduce dosage or interrupt therapy.
Cardiac Arrhythmias, Cardiac Failure, and Sudden Death
Serious arrhythmias and cardiac failure (sometimes fatal) observed, including (grade 3 or higher) ventricular tachyarrhythmias, atrial fibrillation, and atrial flutter. Events reported in patients with and without preexisting hypertension or cardiac comorbidities; however, increased risk in patients with cardiac risk factors (e.g., hypertension, diabetes), acute infections, or history of arrhythmias.
Increased risk in patients with cardiac risk factors, hypertension, diabetes), acute infections, or history of arrhythmias.
Sudden deaths or deaths due to cardiac causes reported.
Assess cardiac history and function at baseline. Monitor for cardiac arrhythmias and cardiac function. Obtain further evaluation (e.g., ECG, echocardiogram) as indicated for patients who develop symptoms of arrhythmia (e.g., palpitations, lightheadedness, syncope, angina), new-onset dyspnea, or other cardiovascular issues. Manage cardiac arrhythmias and cardiac failure appropriately. Follow dose modification recommendations (refer to "Dosage Modification for Toxicity" section); consider risks and benefits of continued ibrutinib therapy.
Hypertension
Hypertension (including grade 3 or higher) reported.
Monitor blood pressure. If hypertension occurs, initiate or adjust antihypertensive therapy as clinically indicated. Follow dosage modification recommendations for grade 3 or higher hypertension (refer to "Dosage Modification for Toxicity" section).
Second Primary Malignancies
Development of other malignancies, including non-skin carcinomas, reported. Non-melanoma skin cancer was the most frequent second primary malignancy.
Hepatotoxicity, Including Drug-induced Liver Injury
Hepatotoxicity, including severe, life-threatening, and potentially fatal cases of drug-induced liver injury (DILI), reported.
Evaluate bilirubin and transaminases at baseline and throughout treatment. Monitor more frequently for liver test abnormalities and clinical signs and symptoms of hepatic toxicity in patients who develop abnormal liver tests after ibrutinib therapy. Withhold ibrutinib for suspected DILI and discontinue therapy if DILI confirmed.
Tumor Lysis Syndrome
Tumor lysis syndrome reported infrequently.
Assess risk of developing tumor lysis syndrome at baseline and take appropriate precautions. Closely monitor patients and treat as clinically indicated.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm based on findings in animals; embryofetal toxicity and teratogenicity demonstrated in animals.
Verify pregnancy status in females of reproductive potential prior to initiating ibrutinib therapy. Apprise patients of potential fetal hazard. Advise females of reproductive potential, and males with female partners of reproductive potential, to use effective contraception during treatment with ibrutinib and for 1 month after last dose
Specific Populations
Pregnancy
May cause fetal harm based on animal findings.
Verify pregnancy status prior to initiating ibrutinib therapy in females of reproductive potential. If used during pregnancy or if patient becomes pregnant while receiving drug, apprise patient of potential fetal hazard.
Lactation
Not known whether ibrutinib or its metabolites are distributed into human milk or if drug has any effect on milk production or breast-fed infant.
Advise females not to breast-feed during treatment with ibrutinib and for 1 week after discontinuing use, due to the potential for severe adverse events in the breast-fed child.
Females and Males of Reproductive Potential
Verify pregnancy status in females of reproductive potential prior to initiating ibrutinib therapy. Advise females of reproductive potential, and males with female partners of reproductive potential, to use effective contraceptive methods during and for 1 month after discontinuance of ibrutinib.
Pediatric Use
Safety and efficacy established for treatment of chronic GVHD after failure of ≥1 lines of systemic therapy in pediatric patients ≥1 year of age. Safety and efficacy not established for treatment of chronic GVHD in pediatric patients <1 year of age.
Safety and efficacy not established in CLL/SLL, CLL/SLL with 17p deletion, or Waldenström macroglobulinemia.
Geriatric Use
In clinical trials, no differences in efficacy in geriatric patients (≥65 years of age) compared with younger adults, but some adverse effects (e.g., anemia, grade 3 or higher pneumonia, thrombocytopenia, hypertension, atrial fibrillation) occurred more frequently in geriatric patients.
Hepatic Impairment
Adults with B-cell malignancies: Avoid use in patients with severe hepatic impairment (Child-Pugh class C). Safety not evaluated in mild to severe hepatic impairment by Child-Pugh criteria. Reduce recommended dosage in patients with mild or moderate hepatic impairment (Child-Pugh class A or B); monitor more frequently for adverse reactions of ibrutinib.
Patients with chronic GVHD: Avoid use in patients with total bilirubin level >3 times ULN (unless of non-hepatic origin or due to Gilbert’s syndrome). Reduce recommended dosage in patients with total bilirubin level >1.5–3 times ULN (unless of non-hepatic origin or due to Gilbert’s syndrome).
Increased systemic exposure and peak plasma concentrations in patients with mild to severe hepatic impairment.
Renal Impairment
Systemic exposure apparently not affected in patients with mild or moderate renal impairment (Clcr >25 mL/minute).
No experience in patients with severe renal impairment (Clcr <25 mL/minute) or in those undergoing dialysis.
Common Adverse Effects
B-cell malignancies (≥30%): Thrombocytopenia, diarrhea, anemia, neutropenia, musculoskeletal pain, rash, bruising, nausea, fatigue.
Chronic GVHD (≥20%; adults and pediatric patients): Fatigue, anemia, bruising, diarrhea, thrombocytopenia, musculoskeletal pain, pyrexia, muscle spasms, stomatitis, nausea, hemorrhage, abdominal pain, headache, pneumonia.
Drug Interactions
Principally metabolized by CYP3A and, to a lesser extent, by CYP2D6 to several metabolites.
Ibrutinib and PCI-45227 (active metabolite) not expected to inhibit CYP isoenzymes 1A2, 2B6, 2C8, 2C9, 2C19, 2D6, or 3A or induce CYP isoenzymes 1A2, 2B6, or 3A at clinically relevant concentrations in vitro.
Ibrutinib not a substrate of P-glycoprotein (P-gp) or breast cancer resistance protein (BCRP) in vitro; may inhibit P-gp and BCRP transport at clinically relevant concentrations.
Drugs and Foods Affecting Hepatic Microsomal Enzymes
CYP3A Inhibitors
Concomitant use with strong or moderate CYP3A inhibitors may increase ibrutinib plasma concentrations, increasing risk of drug-related toxicity.
If concomitant use of the strong CYP3A inhibitor posaconazole or voriconazole or a moderate CYP3A inhibitor required, reduce daily dosage of ibrutinib as recommended in Table 4 in the "Dosage" section. Avoid concomitant use with other strong CYP3A inhibitors; interrupt ibrutinib therapy if these inhibitors will be used short-term (e.g., anti-infectives for ≤7 days).
Avoid grapefruit products and Seville oranges (known to contain strong or moderate inhibitors of CYP3A) during ibrutinib therapy.
CYP3A Inducers
Concomitant use with strong or moderate CYP3A inducers may decrease ibrutinib plasma concentrations.
Avoid concomitant use with strong CYP3A inducers.
Substrates of Efflux Transport Systems
Concomitant use with oral drugs that are substrates of P-gp or BCRP (e.g., digoxin, methotrexate) may increase concentrations of the substrate drug.
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Anticoagulants |
Possible increased risk of hemorrhagic events |
Monitor for bleeding manifestations |
|
Antiplatelet agents |
Possible increased risk of hemorrhagic events |
Monitor for bleeding manifestations |
|
Efavirenz (moderate CYP3A inducer) |
Simulations suggest will decrease AUC of ibrutinib by 3-fold |
|
|
Erythromycin (moderate CYP3A inhibitor) |
Increased ibrutinib peak plasma concentration and AUC by 3.4- and 3-fold, respectively |
If concomitant use unavoidable, modify ibrutinib dosage to 280 mg once daily in patients with B-cell malignancies, to 420 mg once daily in patients ≥12 years of age with chronic GVHD, and to 240 mg/m2 once daily in patients 1 to <12 years of age with chronic GVHD If concomitant erythromycin discontinued, resume ibrutinib therapy at the dosage used prior to initiation of erythromycin |
|
Grapefruit or grapefruit juice |
Grapefruit products are moderate to strong inhibitors of CYP3A; possible increased ibrutinib concentrations |
Avoid concomitant use |
|
Ketoconazole (strong CYP3A inhibitor) |
Increased ibrutinib peak plasma concentration and AUC by 29- and 24-fold, respectively |
Avoid concomitant use; if concomitant use unavoidable and ketoconazole will be used short-term, interrupt ibrutinib therapy |
|
Posaconazole (strong CYP3A inhibitor) |
Simulations suggest increased ibrutinib AUC by 3-fold to 10-fold |
Posaconazole oral suspension 100 mg once or twice daily or 200 mg twice daily: Reduce ibrutinib dosage to 140 mg once daily in patients with B-cell malignancies, and to 280 mg once daily in patients ≥12 years of age with chronic GVHD Posaconazole oral suspension 200 mg 3 times daily or 400 mg twice daily, posaconazole IV 300 mg once daily, or posaconazole delayed-release tablets 300 mg once daily: Reduce ibrutinib dosage to 70 mg once daily in patients with B-cell malignancies, and to 140 mg once daily in patients ≥12 years of age with chronic GVHD Posaconazole at any dosage in patients 1 to <12 years of age with chronic GVHD: Recommended ibrutinib dosage is 80 mg/m2 once daily If concomitant posaconazole discontinued, resume ibrutinib therapy at the dosage used prior to initiation of posaconazole |
|
Rifampin (strong CYP3A inducer) |
Decreased ibrutinib peak plasma concentration and AUC by more than 13- and 10-fold, respectively |
Avoid concomitant use |
|
Seville oranges or Seville orange juice |
Seville orange products are moderate to strong inhibitors of CYP3A; possibly increased ibrutinib concentrations |
Avoid concomitant use |
|
Voriconazole (strong CYP3A inhibitor) |
Increased ibrutinib peak plasma concentration and AUC by 6.7- and 5.7-fold, respectively |
Voriconazole 200 mg twice daily: Reduce ibrutinib dosage to 140 mg once daily in patients with B-cell malignancies, and to 280 mg once daily in patients ≥12 years of age with chronic GVHD Voriconazole for suspension 9 mg/kg (maximum dose: 350 mg) twice daily in patients 1 to <12 years of age with chronic GVHD: Recommended ibrutinib dosage is 160 mg/m2 once daily If concomitant voriconazole discontinued, resume ibrutinib therapy at the dosage used prior to initiation of voriconazole |
Ibrutinib Pharmacokinetics
Absorption
Bioavailability
Following oral administration in healthy individuals in a fasted condition, absolute bioavailability is 2.9%.
Absorbed after oral administration with a median time to peak plasma concentration of 1–2 hours.
Systemic exposure increases with doses up to 840 mg in patients with B-cell malignancies.
Following repeated doses of 420 mg daily, steady-state concentrations achieved in 1 week with accumulation ratio of 1–1.6.
Food
Oral administration with high-fat, high-calorie meal (800–1000 calories with approximately 50% of calories from fat) increases peak plasma concentration by twofold to fourfold and systemic exposure by twofold, compared with administration following overnight fasting.
Special Populations
Patients with mild hepatic impairment (Child-Pugh class A): Peak plasma concentration or systemic exposure increased by 5.2- or 2.7-fold, respectively.
Patients with moderate hepatic impairment (Child-Pugh class B): Peak plasma concentration or systemic exposure increased by 8.8- or 8.2-fold, respectively.
Patients with severe hepatic impairment (Child-Pugh class C): Peak plasma concentration or systemic exposure increased by 7- or 9.8-fold, respectively.
Systemic exposure apparently not affected in patients with mild or moderate renal impairment (Clcr >25 mL/minute).
Distribution
Extent
Extensive tissue distribution; not known whether distributed into milk.
Plasma Protein Binding
97.3%.
Elimination
Metabolism
Metabolized principally by CYP3A and, to a lesser extent, by CYP2D6 to several metabolites; active metabolite: dihydrodiol metabolite PCI-45227.
Elimination Route
Eliminated in feces (80%) and urine (<10%).
Half-life
4–6 hours.
Special Populations
Age and sex do not substantially affect pharmacokinetics of ibrutinib.
Stability
Storage
Oral
Capsules
20–25°C (brief excursions permitted between 15–30°C). Retain in original packaging until dispensing.
Tablets
20–25°C (brief excursions permitted between 15–30°C). Store in original packaging.
Oral Suspension
2–25°C; do not freeze. Dispense in original sealed container; do not use if carton seal missing or broken. Discard any unused oral suspension remaining 60 days after first opening bottle.
Actions
-
Selectively and irreversibly inhibits BTK, resulting in inhibition of downstream effector activity within the B-cell antigen receptor (BCR) signaling pathway.
-
Inhibits other receptor kinases (e.g., Bmx/Etk, EGFR, Hck, Yes) in vitro.
-
Inhibits proliferation and survival of malignant B-cells in vivo.
-
Demonstrates cell migration and substrate adhesion of CLL cells in vitro; mobilization of cells from tissues to peripheral blood results in a transient increase in absolute lymphocyte count in peripheral blood.
Advice to Patients
-
Advise patients and caregivers to read the FDA-approved patient labeling (patient information and instructions for use).
-
Advise patients to take ibrutinib as directed by their clinician and at approximately the same time each day. If a dose is missed, administer missed dose on the same day as soon as it is remembered, and resume normal schedule the following day. Advise patients not to take extra doses on the same day to make up for a missed dose.
-
Instruct patients or caregivers to read and follow the instructions for use for proper preparation, administration, storage, and disposal of ibrutinib oral suspension.
-
Advise patients to take ibrutinib capsules or tablets orally with a glass of water; do not open, break, or chew capsules or cut, crush, or chew tablets.
-
Advise patients of the risk of bleeding. Inform clinician of any episodes of unusual bleeding (e.g., severe headache, blood in stool or urine, prolonged or uncontrolled bleeding). Notify clinician of any planned surgeries, including dental procedures.
-
Advise patients of the risk of serious infection. Report signs or symptoms of possible infection (e.g., chills, fever, weakness, confusion).
-
Advise patients of the risk of cardiac arrhythmias, cardiac failure, and sudden death. Inform clinician if palpitations, lightheadedness, dizziness, fainting, shortness of breath, edema, or chest discomfort occurs.
-
Advise patients of the risk of hypertension, which may require antihypertensive therapy.
-
Advise patients of the possible risk of developing a second primary malignancy (e.g., skin cancer).
-
Advise patients of the risk of tumor lysis syndrome. Report signs or symptoms of tumor lysis syndrome (e.g., arrhythmia, seizure).
-
Advise patients of the risk of diarrhea. Advise patients to maintain adequate hydration during ibrutinib therapy. Inform clinician if diarrhea persists.
-
Inform patients that liver problems may develop during therapy. Advise patients to contact their clinician immediately if they experience abdominal discomfort, dark urine, or jaundice.
-
Advise patients of the risk of fetal harm. Advise females to inform their clinician if they are or plan to become pregnant or plan to breast-feed. Apprise patients of potential hazard to the fetus if ibrutinib is used during pregnancy. Advise females of reproductive potential, and males with female partners of reproductive potential, to use effective contraception during ibrutinib therapy and for 1 month after discontinuance of therapy.
-
Due to potential adverse events to the breast-fed child, advise females to not breast-feed during ibrutinib treatment and for 1 week after discontinuation of therapy.
-
Inform clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses. Advise patients not to consume grapefruit or Seville oranges.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care. For further information on the handling of antineoplastic agents, see the ASHP Guidelines on Handling Hazardous Drugs at [Web].
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Ibrutinib can only be obtained through designated specialty pharmacies. Contact the manufacturer or consult the Imbruvica website ([Web]) for specific availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
70 mg |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
|
140 mg |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
||
|
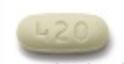
Tablets |
140 mg |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
|
|
280 mg |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
||
|
420 mg |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
||
|
Oral Suspension |
70 mg/mL |
Imbruvica |
Pharmacyclics (comarketed by Janssen Biotech) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- How much does Imbruvica cost?
- How long can you stay on Imbruvica (ibrutinib)?
- Can ibrutinib be stopped safely?
- How quickly does Imbruvica (ibrutinib) work?
- Acalabrutinib vs. ibrutinib: How do they compare?
- Does ibrutinib cause hair loss?
- Is Imbruvica a chemotherapy drug?
- What are the names of the BTK inhibitors?
- Who makes Imbruvica?
More about ibrutinib
- Check interactions
- Compare alternatives
- Reviews (87)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: BTK inhibitors
- Breastfeeding
- En español