Ibrutinib Dosage
Medically reviewed by Drugs.com. Last updated on Aug 26, 2025.
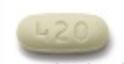
Applies to the following strengths: 70 mg/mL; 140 mg; 70 mg; 280 mg; 420 mg; 560 mg
Usual Adult Dose for:
Usual Pediatric Dose for:
Additional dosage information:
Usual Adult Dose for Chronic Lymphocytic Leukemia
420 mg orally once a day
Duration of therapy: Until disease progression or unacceptable toxicity
Comments:
- This drug can be administered as a single agent, in combination with rituximab or obinutuzumab, or in combination with bendamustine and rituximab.
- If use in combination with rituximab or obinutuzumab: Administration of this drug before rituximab or obinutuzumab should be considered when given on the same day.
Uses:
- For the treatment of patients with chronic lymphocytic leukemia/small lymphocytic lymphoma (CLL/SLL)
- For the treatment of patients with CLL/SLL with 17p deletion
Usual Adult Dose for Waldenstrom's Macroglobulinemia
420 mg orally once a day
Duration of therapy: Until disease progression or unacceptable toxicity
Comments:
- This drug can be administered as a single agent or in combination with rituximab.
- If used in combination with rituximab: Administration of this drug before rituximab should be considered when given on the same day.
- Management of hyperviscosity may include plasmapheresis before and during therapy with this drug; dosing modifications are not needed.
Use: For the treatment of patients with Waldenstrom's macroglobulinemia (WM)
Usual Adult Dose for Graft Versus Host Disease
420 mg orally once a day
Duration of therapy: Until progression of chronic graft-versus-host disease (cGVHD), recurrence of an underlying malignancy, or unacceptable toxicity
Comments:
- When patients no longer require treatment for cGVHD, this drug should be discontinued considering the medical assessment of the individual patient.
Use: For the treatment of patients with cGVHD after failure of 1 or more lines of systemic therapy
Usual Pediatric Dose for Graft Versus Host Disease
1 to less than 12 years: 240 mg/m2 orally once a day
- Maximum dose: 420 mg/dose
Oral Suspension:
Dosage based on BSA (to achieve 240 mg/m2):
- BSA greater than 0.3 to 0.4 m2: 84 mg orally once a day
- BSA greater than 0.4 to 0.5 m2: 105 mg orally once a day
- BSA greater than 0.5 to 0.6 m2: 133 mg orally once a day
- BSA greater than 0.6 to 0.7 m2: 154 mg orally once a day
- BSA greater than 0.7 to 0.8 m2: 182 mg orally once a day
- BSA greater than 0.8 to 0.9 m2: 203 mg orally once a day
- BSA greater than 0.9 to 1 m2: 231 mg orally once a day
- BSA greater than 1 to 1.1 m2: 252 mg orally once a day
- BSA greater than 1.1 to 1.2 m2: 280 mg orally once a day
- BSA greater than 1.2 to 1.3 m2: 301 mg orally once a day
- BSA greater than 1.3 to 1.4 m2: 322 mg orally once a day
- BSA greater than 1.4 to 1.5 m2: 350 mg orally once a day
- BSA greater than 1.5 to 1.6 m2: 371 mg orally once a day
- BSA greater than 1.6 m2: 420 mg orally once a day
Capsules/Tablets:
Dosage based on BSA (to achieve 240 mg/m2):
- BSA greater than 0.7 to 1 m2: 210 mg orally once a day
- BSA greater than 1 to 1.3 m2: 280 mg orally once a day
- BSA greater than 1.3 to 1.6 m2: 350 mg orally once a day
- BSA greater than 1.6 m2: 420 mg orally once a day
12 years and older: 420 mg orally once a day
Duration of Therapy: Until progression of cGVHD, recurrence of an underlying malignancy, or unacceptable toxicity
Comments:
- When patients no longer require treatment for cGVHD, this drug should be discontinued considering the medical assessment of the individual patient.
Use: For the treatment of patients with cGVHD after failure of 1 or more lines of systemic therapy
Renal Dose Adjustments
Mild and moderate renal dysfunction (CrCl greater than 25 mL/min): No adjustment recommended
Severe renal dysfunction (CrCl less than 25 mL/min): Data not available
Comments:
- CrCl as estimated by Cockcroft-Gault equation
Liver Dose Adjustments
Adult patients with B-cell malignancies:
- Mild liver dysfunction (Child-Pugh A): 140 mg orally once a day
- Moderate liver dysfunction (Child-Pugh B): 70 mg orally once a day
- Severe liver dysfunction (Child-Pugh C): Not recommended
Patients with cGVHD:
- Total bilirubin greater than 1.5 to 3 times the upper limit of normal (1.5 to 3 x ULN), unless of nonhepatic origin or due to Gilbert's syndrome:
- Patients 12 years and older: 140 mg orally once a day
- Patients 1 to less than 12 years: 80 mg/m2 orally once a day
- Total bilirubin greater than 3 x ULN, unless of nonhepatic origin or due to Gilbert's syndrome: Not recommended
Comments:
- Adult patients with B-cell malignancies:
- Safety has not been evaluated in patients with mild to severe liver dysfunction by Child-Pugh criteria.
- Patients with mild or moderate liver dysfunction (Child-Pugh A and B) should be monitored more frequently for adverse reactions.
Dose Adjustments
DOSAGE MODIFICATIONS FOR ADVERSE REACTIONS:
This drug should be interrupted for the adverse reactions listed below. Once the adverse reaction has improved to grade 1 or baseline (recovery), the recommended dosage modifications should be followed.
Dose Modification for CLL/SLL, WM, and Patients 12 Years and Older with cGVHD After Recovery (Starting Dose = 420 mg):
Cardiac arrhythmias:
- Grade 3:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 280 mg orally once a day
- Second occurrence: This drug should be discontinued.
- Grade 4: This drug should be discontinued.
Cardiac failure:
- Grade 2:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 280 mg orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 140 mg orally once a day
- Third occurrence: This drug should be discontinued.
- Grade 3 or 4: This drug should be discontinued.
Hematological toxicities:
- Grade 4:
- First occurrence: Should restart at 280 mg orally once a day
- Second occurrence: Should restart at 140 mg orally once a day
- Third occurrence: This drug should be discontinued.
Neutropenia with infection or fever:
- Grade 3 or 4:
- First occurrence: Should restart at 280 mg orally once a day
- Second occurrence: Should restart at 140 mg orally once a day
- Third occurrence: This drug should be discontinued.
Other nonhematological toxicities:
- Grade 3:
- First occurrence: Should restart at 280 mg orally once a day
- Second occurrence: Should restart at 140 mg orally once a day
- Third occurrence: This drug should be discontinued.
- Grade 4:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 280 mg orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 140 mg orally once a day
- Third occurrence: This drug should be discontinued.
Dose Modification for Patients 1 to Less Than 12 Years with cGVHD After Recovery (Starting Dose = 240 mg/m2):
Cardiac arrhythmias:
- Grade 3:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 160 mg/m2 orally once a day
- Second occurrence: This drug should be discontinued.
- Grade 4: This drug should be discontinued.
Cardiac failure:
- Grade 2:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 160 mg/m2 orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 80 mg/m2 orally once a day
- Third occurrence: This drug should be discontinued.
- Grade 3 or 4: This drug should be discontinued.
Hematological toxicities:
- Grade 4:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 160 mg/m2 orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 80 mg/m2 orally once a day
- Third occurrence: This drug should be discontinued.
Neutropenia with infection or fever:
- Grade 3 or 4:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 160 mg/m2 orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 80 mg/m2 orally once a day
- Third occurrence: This drug should be discontinued.
Other nonhematological toxicities:
- Grade 3 or 4:
- First occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 160 mg/m2 orally once a day
- Second occurrence: The benefit-risk should be evaluated before resuming therapy; should restart at 80 mg/m2 orally once a day
- Third occurrence: This drug should be discontinued.
Oral Suspension:
Dosage based on BSA (to achieve 160 mg/m2):
- BSA greater than 0.3 to 0.4 m2: 56 mg orally once a day
- BSA greater than 0.4 to 0.5 m2: 70 mg orally once a day
- BSA greater than 0.5 to 0.6 m2: 91 mg orally once a day
- BSA greater than 0.6 to 0.7 m2: 105 mg orally once a day
- BSA greater than 0.7 to 0.8 m2: 119 mg orally once a day
- BSA greater than 0.8 to 0.9 m2: 133 mg orally once a day
- BSA greater than 0.9 to 1 m2: 154 mg orally once a day
- BSA greater than 1 to 1.1 m2: 168 mg orally once a day
- BSA greater than 1.1 to 1.2 m2: 182 mg orally once a day
- BSA greater than 1.2 to 1.3 m2: 203 mg orally once a day
- BSA greater than 1.3 to 1.4 m2: 217 mg orally once a day
- BSA greater than 1.4 to 1.5 m2: 231 mg orally once a day
- BSA greater than 1.5 to 1.6 m2: 245 mg orally once a day
- BSA greater than 1.6 m2: 280 mg orally once a day
Capsules/Tablets:
Dosage based on BSA (to achieve 160 mg/m2):
- BSA greater than 0.7 to 1.1 m2: 140 mg orally once a day
- BSA greater than 1.1 to 1.5 m2: 210 mg orally once a day
- BSA greater than 1.5 m2: 280 mg orally once a day
Oral Suspension:
Dosage based on BSA (to achieve 80 mg/m2):
- BSA greater than 0.3 to 0.4 m2: 38 mg orally once a day
- BSA greater than 0.4 to 0.5 m2: 35 mg orally once a day
- BSA greater than 0.5 to 0.6 m2: 42 mg orally once a day
- BSA greater than 0.6 to 0.7 m2: 49 mg orally once a day
- BSA greater than 0.7 to 0.8 m2: 63 mg orally once a day
- BSA greater than 0.8 to 0.9 m2: 70 mg orally once a day
- BSA greater than 0.9 to 1 m2: 77 mg orally once a day
- BSA greater than 1 to 1.1 m2: 84 mg orally once a day
- BSA greater than 1.1 to 1.2 m2: 91 mg orally once a day
- BSA greater than 1.2 to 1.3 m2: 98 mg orally once a day
- BSA greater than 1.3 to 1.4 m2: 105 mg orally once a day
- BSA greater than 1.4 to 1.5 m2: 119 mg orally once a day
- BSA greater than 1.5 to 1.6 m2: 126 mg orally once a day
- BSA greater than 1.6 m2: 140 mg orally once a day
Capsules/Tablets:
Dosage based on BSA (to achieve 80 mg/m2):
- BSA greater than 0.7 to 1.1 m2: 70 mg orally once a day
- BSA greater than 1.1 to 1.4 m2: The oral suspension should be used.
- BSA greater than 1.4 m2: 140 mg orally once a day
DOSAGE MODIFICATIONS FOR USE WITH CYP450 3A INHIBITORS:
Patients with B-cell malignancies:
- If coadministered with a moderate CYP450 3A inhibitor: 280 mg orally once a day
- Dose should be modified as recommended for adverse reactions.
- If coadministered with voriconazole (200 mg twice a day) or posaconazole suspension (100 mg once a day, 100 mg twice a day, or 200 mg twice a day): 140 mg orally once a day
- Dose should be modified as recommended for adverse reactions.
- If coadministered with posaconazole suspension (200 mg 3 times a day or 400 mg twice a day), posaconazole IV (300 mg once a day), or posaconazole delayed-release tablets (300 mg once a day): 70 mg orally once a day
- Dose should be interrupted as recommended for adverse reactions.
- If coadministered with other strong CYP450 3A inhibitors: Concomitant use should be avoided.
- If these inhibitors will be used short-term (e.g., anti-infectives for up to 7 days), this drug should be interrupted.
Patients 12 years and older with cGVHD:
- If coadministered with a moderate CYP450 3A inhibitor: 420 mg orally once a day
- Dose should be modified as recommended for adverse reactions.
- If coadministered with voriconazole (200 mg twice a day) or posaconazole suspension (100 mg once a day, 100 mg twice a day, or 200 mg twice a day): 280 mg orally once a day
- Dose should be modified as recommended for adverse reactions.
- If coadministered with posaconazole suspension (200 mg 3 times a day or 400 mg twice a day), posaconazole IV (300 mg once a day), or posaconazole delayed-release tablets (300 mg once a day): 140 mg orally once a day
- Dose should be interrupted as recommended for adverse reactions.
- If coadministered with other strong CYP450 3A inhibitors: Concomitant use should be avoided.
- If these inhibitors will be used short-term (e.g., anti-infectives for up to 7 days), this drug should be interrupted.
Patients 1 to less than 12 years with cGVHD:
- If coadministered with moderate CYP450 3A inhibitors: 240 mg/m2 orally once a day
- Dose should be modified as recommended for adverse reactions.
- If coadministered with voriconazole for suspension (9 mg/kg twice a day; maximum dose: 350 mg): 160 mg/m2 orally once a day
- If coadministered with posaconazole (at any dosage): 80 mg/m2 orally once a day
- If coadministered with other strong CYP450 3A inhibitors: Concomitant use should be avoided.
- If these inhibitors will be used short-term (e.g., anti-infectives for up to 7 days), this drug should be interrupted.
After discontinuation of a CYP450 3A inhibitor, the previous dose of this drug should be resumed.
Precautions
CONTRAINDICATIONS: None
Safety and efficacy have not been established for cGVHD in patients younger than 1 year. Safety and efficacy have not been established in patients younger than 18 years with CLL/SLL, CLL/SLL with 17p deletion, or WM.
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Administer at about the same time each day.
- Swallow capsules or tablets whole with a glass of water.
- Do not open, break, or chew the capsules.
- Do not cut, crush, or chew the tablets.
- Discard any remaining oral suspension 60 days after first opening the bottle.
- Avoid grapefruit and Seville oranges during therapy.
Storage requirements:
- Capsules: Store bottles at 20C to 25C (68F to 77F); brief exposure to 15C to 30C (59F to 86F) permitted. Keep in original package until dispensing.
- Oral suspension: Store bottle at 2C to 25C (36F to 77F); do not freeze. Dispense in original sealed container.
- Tablets: Store in original packaging at 20C to 25C (68F to 77F); brief exposure to 15C to 30C (59F to 86F) permitted.
Reconstitution/preparation techniques:
- Oral suspension: The manufacturer product information (Instructions for Use) should be consulted for further administration details.
Monitoring:
- Cardiovascular: Cardiac history and function (at baseline); for cardiac arrhythmias and cardiac function; blood pressure
- Hematologic: For signs/symptoms of bleeding; CBC (monthly)
- Infections/Infestations: For infections and fever
- Metabolism: For tumor lysis syndrome
Patient advice:
- Read the US FDA-approved patient labeling (Patient Information and Instructions for Use).
- Report any signs/symptoms of bleeding (e.g., severe headache, blood in stools/urine, prolonged/uncontrolled bleeding).
- Report any signs/symptoms suggestive of infection (e.g., fever, chills, weakness, confusion).
- Report any signs of palpitations, lightheadedness, dizziness, fainting, shortness of breath, chest discomfort, or edema.
- Report any signs/symptoms associated with tumor lysis syndrome to your health care provider for evaluation.
- Patients of childbearing potential: Inform health care provider of a known/suspected pregnancy; use effective contraception during therapy and for 1 month after the last dose.
- Male patients with female partners of childbearing potential: Use effective contraception during therapy and for 1 month after the last dose.
- Do not breastfeed during therapy and for 1 week after the last dose.
- Loose stools or diarrhea may occur; contact physician if diarrhea persists. Maintain adequate hydration.
- If a dose is not taken at the scheduled time, take it as soon as possible on the same day and return to the normal schedule the following day; do not take extra doses to make up for the missed dose.
Frequently asked questions
- How much does Imbruvica cost?
- How long can you stay on Imbruvica (ibrutinib)?
- Can ibrutinib be stopped safely?
- How quickly does Imbruvica (ibrutinib) work?
- Acalabrutinib vs. ibrutinib: How do they compare?
- Does ibrutinib cause hair loss?
- Is Imbruvica a chemotherapy drug?
- What are the names of the BTK inhibitors?
- Who makes Imbruvica?
More about ibrutinib
- Check interactions
- Compare alternatives
- Reviews (87)
- Side effects
- Patient tips
- During pregnancy
- Support group
- Drug class: BTK inhibitors
- Breastfeeding
- En español
Patient resources
Other brands
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.