Imbruvica
Pronunciation: im-BRU-vih-kuh
Generic name: ibrutinib
Dosage forms: oral capsules, oral tablets, oral suspension
Drug class: BTK inhibitors
What is Imbruvica?
Imbruvica (ibrutinib) is a targeted therapy used to treat chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma (SLL), Waldenström’s macroglobulinemia (WM), and chronic graft versus host disease (cGVHD) in certain patients. Imbruvica helps slow cancer progression in CLL, SLL, and WM and slow disease progression in cGVHD.
Imbruvica is an oral, once-daily medicine available as a capsule, tablet, or oral suspension.
Imbruvica is a BTK inhibitor, it is a targeted therapy that works differently from chemotherapy drugs.
Imbruvica works by targeting and inhibiting the enzyme Bruton tyrosine kinase (BTK). Bruton tyrosine kinase signals certain cancer cells, telling them to grow and divide uncontrollably. Imbruvica targets and blocks BTK, which stops the cancer cells from multiplying, and triggers cancer cells to die.
Imbruvica FDA approval was first granted on November 13, 2013.
What is Imbruvica used for?
Imbruvica is FDA-approved to be used for:
- chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) in adults
- chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) with 17p deletion in adults
- Waldenström’s macroglobulinemia (WM) in adults
- chronic graft versus host disease (cGVH), after failure of one or more lines of systemic therapy for adult and pediatric patients aged 1 year and older.
Imbruvica is no longer indicated for mantle cell lymphoma (MCL) or marginal zone lymphoma (MZL).
How does Imbruvica work?
Imbruvica's mechanism of action is as a BTK inhibitor by directly inhibiting Bruton’s tyrosine kinase (BTK). It forms a covalent bond with a cysteine residue on the enzyme, preventing its activity. BTK works as a signaling molecule for the B-cell antigen receptor (BCR) and cytokine receptor pathways. Activation of these pathways causes the proliferation of B cells and other interactions, and inhibition has been shown to reduce the growth and spread of malignant B cells.
Imbruvica belongs to the class of medicines known as BTK inhibitors.
Imbruvica side effects
Common side effects of Imbruvica
Common Imbruvica side effects may include:
- Diarrhea 59%
- Bruising 51%
- Upper respiratory tract infection 47%
- Fatigue, tiredness 33%
- Musculoskeletal pain 25%
- Rash 25%
- Fever 24%
- Joint pain 24%
- Constipation 22%
- Sinusitis 22%
- Cough 22%
- Swelling of extremities 22%
- Dizziness 20%
- Nausea 20%
- Mouth ulcers, stomatitis 20%
- Headache 18%
- Muscle spasms 18%
- Vomiting 18%
- High blood pressure 16%
- Low appetitie 16%
- Petechiae 16%
- Skin infection 16%
- Abdominal pain 14%
- Weakness, lack of energy and strength 14%
- Oropharyngeal pain, pain in the middle area or the throat 14%
- Chills 12%
- Difficulty breathing 12%
- Dyspepsia, indigestion 12%
- Pneumonia 12%
- Urinary tract infection 12%
- Second cancers 10%
These common side effects occurred in 10% or more of Imbruvica patients in the CLL/SLL clinical trial called Study 1102.
This medicine also cause blood test abnormalities including decreased platelets, neutrophils and hemoglobin levels. Your HCP will monitor your blood tests regularly.
Serious side effects of Imbruvica
Get emergency medical help if you have signs of an allergic reaction: hives, difficulty breathing, swelling of your face, lips, tongue, or throat.
Imbruvica may cause other serious side effects. Call your doctor at once if you have:
- severe or ongoing diarrhea;
- heart problems - swelling, rapid weight gain, feeling short of breath;
- heart rhythm disorders - dizziness, chest pain, shortness of breath, fast or irregular heart rate, feeling light-headed;
- high blood pressure- severe headache, blurred vision, pounding in your neck or ears;
- low blood cell counts - fever, chills, tiredness, mouth sores, skin sores, easy bruising, unusual bleeding, pale skin, cold hands, and feet, feeling light-headed or short of breath;
- kidney problems - swelling, urinating less, feeling tired or short of breath;
- liver problems - stomach pain or discomfort, dark-colored urine, or yellow skin and eyes;
- signs of tumor cell breakdown - tiredness, weakness, muscle cramps, nausea, vomiting, diarrhea, fast or slow heart rate, tingling in your hands and feet or around your mouth.
Also see the Warning section.
Your cancer treatments may be delayed or permanently discontinued if you have certain side effects.
This is not a complete list of side effects and others may occur. Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Imbruvica for CLL
Imbruvica for CLL/SLL can be used for patients:
- as a first-line treatment or in patients who have previously had treatment for their cancer, and includes patients with or without a deletion in chromosome 17 (17p deletion).
- in combination with Gazyva (obinutuzumab) for the treatment of previously untreated patients
- in combination with rituximab (Rituxan and other brands) for the treatment of previously untreated patients.
In CLL/SLL clinical trial RESONATE-2 (NCT01722487) Imbruvica significantly prolonged CLL/SLL overall survival with a relative risk of death that was 84% lower than chlorambucil at 24 months when used as monotherapy. The estimated CLL/SLL Imbruvica survival rate at 24 months was 98% versus 85% with chlorambucil.
The median progression-free survival (PFS) was not reached for Imbruvica compared to 18.9 months for chlorambucil. Imbruvica had a risk of progression or death that was 84% lower with ibrutinib than that with chlorambucil.
Warnings
Serious hemorrhage, including intracranial or gastrointestinal hemorrhage, hematuria, and post-procedural hemorrhage has occurred in people receiving Imbruvica, 0.4% have been fatal. 39% of people reported bleeding of any grade, including purpura and petechiae. Coadministration with antiplatelet or anticoagulants may increase the risk. Your doctor will monitor for signs and symptoms of bleeding and discontinue if serious bleeding occurs. They may consider withholding Imbruivca for 3 to 7 days pre and post surgery depending on the risk of bleeding. Call your doctor at once if you have signs of bleeding inside your body, such as dizziness, confusion, headache, speech problems, black or bloody stools, pink or brown urine, or coughing up blood or vomit that looks like coffee grounds.
Infections. This medication affects your immune system. Serious bacterial, viral, or fungal infections have been reported with Imbruvica; 21% were Grade 3 or higher. Cases of progressive multifocal leukoencephalopathy (PML) and Pneumocystis jirovecii pneumonia (PJP) have occurred, in addition to reactivation of hepatitis B. Consider prophylaxis for herpes simplex virus, pneumocystis jirovecii pneumonia, and other infections in patients who are at increased risk for infections. Tell your doctor if you have a fever, chills, cough, mouth sores, or other signs of infection.
Progressive multifocal leukoencephalopathy (PML) is a brain infection caused by a virus (polyomavirus JC) that can lead to disability or death. Tell your doctor if you have problems with speech, thought, vision, or muscle movement. These symptoms can get worse quickly. Tell your doctor if you have a fever, chills, cough, mouth sores, or other signs of infection.
High blood pressure (hypertension) Hypertension as a side effect occurred in 19% of 1,476 patients with B-cell malignancies taking Imbruvica in clinical trials. Grade 3 or greater hypertension affects 8% of patients and the rate increases the longer the medicine is taken. BP should be measured regularly and treated as necessary.
Serious cardiac arrhythmias and cardiac disease, including atrial fibrillation, atrial flutter, ventricular arrhythmias, heart failure, and sudden death, have been reported in patients treated with Imbruvica. The risk is more likely in those with cardiac risk factors, high blood pressure, and acute infections. High blood pressure occurred in 19% of people prescribed Imbruvica in clinical trials. Monitor yourself for signs and symptoms of cardiac arrhythmias (such as palpitations, dizziness, dizziness when standing, and shortness of breath) and report these to your doctor immediately. Your doctor will check your blood pressure regularly.
Blood count abnormalities, including neutropenia, thrombocytopenia, and anemia, have occurred in people receiving Imbruvica. Your doctor will perform regular blood counts and interrupt treatment, reduce the dose, or discontinue treatment as warranted.
Second Primary Malignancies. Using Imbruvica may increase your risk of developing other cancers, such as non-melanoma skin cancer. Ask your doctor about this risk and what skin symptoms to watch for. Wear protective clothing and use sunscreen (SPF 30 or higher) when you are outdoors.
Tumor Lysis syndrome has been reported infrequently with Imbruvica. Symptoms include nausea and vomiting, diarrhea, and muscle cramps. If you have any symptoms like these, report them to your doctor.
Imbruvica can cause fetal harm when administered to a pregnant woman, including malformations. Women should use effective contraception and avoid becoming pregnant while taking Imbruivca and for 1 month after the last dose. Men should avoid fathering a child during treatment and for 1 month after the last dose.
Before taking this medicine
To make sure Imbruvica is safe for you, tell your doctor if you have ever had:
- an infection
- bleeding problems
- take a blood thinner such as warfarin
- a heart rhythm disorder
- risk factors for heart disease (such as diabetes, smoking, being overweight, having high blood pressure or high cholesterol)
- low blood cell counts
- recent surgery or plan to have surgery, medical or dental procedure
- liver disease.
Taking Imbruvica may increase your risk of developing other cancers. Ask your doctor about this risk.
Pregnancy
Ibrutinib can harm an unborn baby if the mother or the father is using this medication.
If you are a woman, you may need a pregnancy test to make sure you are not pregnant. Use birth control while using Imbruvica and for at least 1 month after your last dose. If you are a man, use birth control if your sex partner can get pregnant. Keep using birth control for at least 1 month after your last dose. Tell your doctor right away if a pregnancy occurs.
Breastfeeding
Do not breastfeed while using Imbruvica, and for at least 1 week after your last dose.
How should I take Imbruvica?
Take Imbruvica exactly as prescribed by your doctor. Follow all directions on your prescription label and read all medication guides or instruction sheets.
Take this medicine with a full glass of water, at the same time each day. Drink plenty of liquids while you are taking Imbruvica.
- Swallow the Imbruvica tablet or capsule whole and do not crush, chew, break, or open it.
- Shake the oral suspension (liquid). Measure a dose with the supplied measuring device (not a kitchen spoon), then take the medicine.
Tell your healthcare providers if you have a planned surgery.
You may get dehydrated during prolonged illness. Call your doctor if you are sick with vomiting or diarrhea.
You may get infections or bleed more easily. You will need frequent blood and medical tests.
Imbruvica dosing information
The dose of Imbruvica varies depending on the condition being treated:
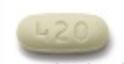
Imbruvica Dosage for Adults with CLL/SLL and WM
- 420mg once daily.
Imbruvica Dosage for cGVHD
- Patients 12 years and older: 420mg once daily
- Patients 1 year old to less than 12 years old: 240mg/m2 once daily (up to a maximum dosage of 420mg once daily).
Imbruvica Dosage forms and strengths
- Capsules: 70 mg and 140 mg
- Tablets: 140 mg, 280 mg, and 420 mg
- Oral suspension: 70 mg/mL
What happens if I miss a dose?
Take the missed dose on the same day you remember it. Take your next dose at the regular time and stay on your once-daily schedule. Do not take 2 doses on the same day.
What happens if I overdose?
Seek emergency medical attention or call the Poison Help line at 1-800-222-1222.
What should I avoid while taking this medicine?
Avoid grapefruit and Seville oranges with Imbruvica, as this may cause side effects. Avoid consuming grapefruit products and orange marmalades.
What other drugs will affect Imbruvica?
Sometimes it is not safe to use certain medicines at the same time. Some drugs can affect your blood levels of other drugs you use, which may increase side effects or make the medicines less effective.
- Moderate to strong CYP3A Inhibitors, such as clarithromycin, nefazodone, itraconazole, ketoconazole, atazanavir, ritonavir, grapefruit juice, erythromycin, or verapamil
- Moderate to strong CYP3A inducers, such as glucocorticoids, rifampin, carbamazepine, phenobarbital, and phenytoin. Avoid coadministration.
Other drugs may interact with ibrutinib, including prescription and over-the-counter medicines, vitamins, and herbal products. Tell your doctor about all other medicines you use.
Imbruvica Package Insert
HCPs and patients often use the Imbruvica Package Insert (PI) for more detailed information about this medicine. The Imbruvica Package Insert (prescribing information) contains more comprehensive information on Indications and Usage, Dosage and Administration, Clinical Pharmacology, Clinical Studies, Drug Interaction, and more. Discuss any medical questions you have with your HCP (health care professional). This is not all the information you need to know about this medicine for safe and effective use, and it does not take the place of talking to your doctor about your treatment.
The Package Insert is sometimes called Imbruvica Prescribing Information (PI) or FDA label.
Imbruvica and Medicare
Because of the prescription drug law, known as the Inflation Reduction Act, Medicare is able to negotiate directly with drug companies to improve access to some of the costliest single-source brand-name Medicare Part B and Part D drugs.
Imbruvica is one of 10 drugs covered under Medicare Part D that were selected in 2024 for the first cycle of negotiation based on Total Expenditures under Part D and other criteria as required by the law. Negotiations with participating drug companies are ongoing, and any negotiated prices for the first cycle of negotiation is effective from 2026.
Ingredients
Active ingredient: ibrutinib.
- Tablets are supplied in three strengths: 140mg, 280mg, 420mg
- Capsules are supplied in two strengths: 70mg and 140mg
- Oral suspension: 70mg/mL. The bottle contains 108mL suspension in a 150mL bottle.
Inactive ingredients:
- Capsules: croscarmellose sodium, magnesium stearate, microcrystalline cellulose, sodium lauryl sulfate. The capsule shell contains gelatin, titanium dioxide, yellow iron oxide (70 mg capsule only), and black ink.
- Tablets: colloidal silicon dioxide, croscarmellose sodium, lactose monohydrate, magnesium stearate, microcrystalline cellulose, povidone, and sodium lauryl sulfate. The film coating for each tablet contains ferrosoferric oxide (140 mg, 280 mg, and 420 mg tablets), polyvinyl alcohol, polyethylene glycol, red iron oxide (280 mg tablets), talc, titanium dioxide, and yellow iron oxide (140 mg and 420 mg tablets).
- Oral suspension: benzyl alcohol, citric acid monohydrate, disodium hydrogen phosphate, hypromellose, microcrystalline cellulose, and carboxymethylcellulose sodium, purified water, and sucralose.
Storage
Store in the original container at room temperature 68°F to 77°F (20°C to 25°C), away from moisture and heat. Store bottles at room temperature. Brief exposure to 59°F to 86°F (15°C to 30°C) permitted. Retain in original package until dispensing.
Store opened oral suspension (liquid) in the refrigerator or at room temperature between 36°F and 77°F (2°C and 25°C). Do not freeze. Throw away after 60 days of the first opening.
Imbruvica capsules and oral suspension come in a bottle with a child-resistant cap.
Manufacturer
Imbruvica manufacturer Janssen Biotech, Inc. 2023 and Pharmacyclics LLC 2023.
Popular FAQ
How much does Imbruvica cost?
According to the Drugs.com price guide which bases its price on the Drugs.com discount card which is accepted at most U.S. pharmacies, the cost for Imbruvica 420mg tablet is around $616 per tablet or $17 269 for a supply of 28 tablets depending on the pharmacy you visit. Prices are for cash paying customers only and are not valid with insurance plans. Continue reading
How long can you stay on Imbruvica (ibrutinib)?
Imbruvica (ibrutinib) is usually continued indefinitely if it is being well tolerated, there is limited disease progression, and toxicity has not occurred. Continue reading
How quickly does Imbruvica (ibrutinib) work?
In some people, very good partial clinical responses to Imbruvica may occur within three to six months. Imbruvica is usually given until disease progression or unacceptable toxicity occurs, or in the case of graft vs host disease, recurrence of an underlying malignancy. The average duration of Imbruvica therapy in clinical trials has been around 41 months (range, 2–51 months).
Continue readingDoes ibrutinib cause hair loss?
Hair loss (alopecia) has not been noted as a side effect of ibrutinib (Imbuvica) in the product label. Textural hair changes (softening, straightening or curliness) and nail changes (brittle fingernails and toenails) were noted in a study evaluating ibrutinib use over the long term for treatment of chronic lymphocytic leukemia (CLL). Continue reading
How to apply for and use the Imbruvica copay card?
You can apply for the Imbruvica copay card by signing up at the Imbruvica website or using the Drugs.com Price Guide. If you are eligible, you may pay as little as $0 for your prescription. Present your card to your pharmacist or other representative to process your prescription and tell you your out-of-pocket costs. Continue reading
More FAQ
References
More about Imbruvica (ibrutinib)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (69)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- FDA approval history
- Drug class: BTK inhibitors
- Breastfeeding
- En español
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.