Daridorexant (Monograph)
Brand name: Quviviq
Drug class: Orexin Receptor Antagonists
Introduction
Hypnotic; orexin receptor antagonist.
Uses for Daridorexant
Insomnia
Management of insomnia, characterized by difficulty with sleep onset and/or sleep maintenance, in adults.
Improves sleep onset and sleep maintenance.
Daridorexant Dosage and Administration
General
Pretreatment Screening
-
Because sleep disturbances may be a manifestation of a physical and/or psychiatric disorder, symptomatic treatment of insomnia should be initiated only after careful evaluation of the patient.
Patient Monitoring
-
Monitor for somnolence and CNS depressant effects.
Administration
Oral Administration
Administer orally, no more than once per night, within 30 minutes of bedtime.
May administer without regard to meals; however, administration with or immediately after a meal decreases rate of absorption and may delay onset of effect.
Use only if ≥7 hours remain before planned time of awakening.
Dosage
Dosage of daridorexant hydrochloride is expressed in terms of daridorexant.
Adults
Insomnia
Oral
25–50 mg no more than once per night.
When used concomitantly with a moderate CYP3A4 inhibitor, recommended dosage of daridorexant is 25 mg taken no more than once per night. Avoid concomitant use of strong CYP3A4 inhibitors or strong or moderate CYP3A4 inducers.
When used concomitantly with other CNS depressants, dosage adjustment of daridorexant or the other CNS depressant may be necessary because of potential additive effects.
Special Populations
Hepatic Impairment
Moderate hepatic impairment (Child-Pugh score 7–9): Maximum daridorexant dosage of 25 mg no more than once per night.
Severe hepatic impairment (Child-Pugh score ≥10): Use not recommended.
Renal Impairment
Manufacturer makes no specific dosage recommendations.
Geriatric Use
Dosage adjustment not necessary based solely on age.
Cautions for Daridorexant
Contraindications
-
Narcolepsy.
Warnings/Precautions
CNS Depressant Effects and Daytime Impairment
CNS depressant; may impair daytime wakefulness even when used as prescribed. May increase risk of falls, particularly in geriatric patients. May impair ability to drive a motor vehicle. Effects may persist for up to several days after drug discontinuance.
Risk of daytime impairment is increased if administered with less than a full night of sleep remaining, if a higher than recommended dose is administered, or if used concomitantly with other CNS depressants. Caution patients against driving and other activities requiring complete mental alertness the day after use if the drug is taken under these circumstances.
Concomitant use with other CNS depressants (e.g., alcohol, benzodiazepines, opiates, tricyclic antidepressants) increases risk of CNS depression.
Worsening of Depression and Suicidal Ideation
Worsening of depression and suicidal thoughts and actions (including completed suicides) reported in primarily depressed patients receiving sedative and hypnotic agents. Patients with psychiatric disorders, including insomnia, are at increased risk of suicide. Use with caution in patients exhibiting symptoms of depression; monitoring of suicide risk and protective measures may be required.
Sleep Paralysis, Hypnagogic/Hypnopompic Hallucinations, and Cataplexy-like Symptoms
Sleep paralysis (inability to move or speak for up to several minutes during sleep-wake transition) and hypnagogic/hypnopompic hallucinations may occur. Symptoms similar to mild cataplexy (e.g., leg weakness lasting from seconds to a few minutes) may occur at night and/or during the day; may not be associated with an identified triggering event (e.g., laughter or surprise).
Complex Sleep Behaviors
Complex sleep behaviors, including sleep-walking, sleep-driving, and engaging in other activities while not fully awake (e.g., preparing and eating food, making phone calls, having sex) reported.
Can occur in hypnotic agent-naive or -experienced patients, following the first dose or at any time during treatment, and with or without concomitant use of alcohol or other CNS depressants.
Discontinue daridorexant immediately if a complex sleep behavior occurs.
Patients with Compromised Respiratory Function
If used in patients with compromised respiratory function, consider possible effects on respiratory function. Respiratory depressant effects in patients with compromised respiratory function cannot be excluded; not studied in patients with moderate obstructive sleep apnea (OSA) requiring CPAP, severe OSA, or COPD.
Adequate Patient Evaluation
Insomnia may be a manifestation of a physical and/or psychiatric disorder; carefully evaluate patient before providing symptomatic treatment.
Failure of insomnia to remit after 7–10 days of daridorexant therapy, worsening of insomnia, or emergence of new cognitive or behavioral abnormalities may indicate the presence of an underlying psychiatric, physical, and/or medical condition requiring evaluation.
Abuse Potential and Dependence
Abuse potential of high daridorexant doses (100–150 mg) appears to be similar to that of high zolpidem tartrate doses (30 mg) or high suvorexant doses (150 mg). Patients with a history of drug or alcohol abuse or addiction are at increased risk of abuse and addiction; use only with careful surveillance in such patients.
Discontinuance following chronic administration did not produce withdrawal symptoms. Does not appear to produce physical dependence.
Specific Populations
Pregnancy
No adequate data in humans. In animal reproduction studies, no fetal toxicity or malformations observed at dosages higher than recommended human dosage.
Pregnancy registry at 833-400-9611.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Consider benefits of breast-feeding and importance of the drug to the woman; also consider potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
Incidence of somnolence and fatigue increased with patient age.
Geriatric patients particularly at higher risk of falls.
Hepatic Impairment
Moderate hepatic impairment (Child-Pugh score 7–9): Maximum daridorexant dose of 25 mg no more than once per night.
Severe hepatic impairment (Child-Pugh score ≥10): Use not recommended.
Renal Impairment
Mild to severe renal impairment (estimated GFR <30 mL/minute, not on dialysis): No clinically important effect on daridorexant pharmacokinetics.
Common Adverse Effects
Common adverse effects (≥5%): headache, somnolence, fatigue.
Drug Interactions
Metabolized primarily by CYP3A4.
Not a substrate of any major influx or efflux transporters.
Weak inhibitor of CYP3A4 and BCRP.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 Inhibitors: Potential increased plasma concentrations and adverse effects of daridorexant. Avoid concomitant use with strong CYP3A4 inhibitors. If used concomitantly with a moderate CYP3A4 inhibitor, maximum recommended daridorexant dose is 25 mg no more than once per night.
CYP3A4 Inducers: Potential decreased plasma concentrations and efficacy of daridorexant. Avoid concomitant use with strong or moderate CYP3A4 inducers.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Citalopram |
No clinically important effect on pharmacokinetics or pharmacodynamics (psychomotor performance) of daridorexant or pharmacokinetics of citalopram |
No dosage adjustment recommended |
|
CNS Depressants |
Possible additive CNS depression Alcohol: Additive psychomotor impairment |
Alcohol: Avoid concomitant use Other hypnotics: Concomitant use not recommended Other CNS depressants: Dosage reduction of daridorexant and/or other CNS depressants may be necessary |
|
Diltiazem |
Daridorexant AUC and peak concentrations increased by approximately 2.4- and 1.4-fold, respectively |
Maximum daridorexant dose 25 mg no more than once per night |
|
Efavirenz |
Daridorexant AUC and peak concentrations decreased by 61 and 35%, respectively |
Avoid concomitant use |
|
Famotidine |
Famotidine reduced daridorexant peak concentrations by approximately 40%; no effect on daridorexant AUC |
No dosage adjustment recommended |
|
Itraconazole |
Predicted increase in daridorexant AUC of >4-fold |
Avoid concomitant use |
|
Midazolam |
No clinically important effect on midazolam pharmacokinetics |
No dosage adjustment recommended |
|
Rifampin |
Predicted decrease in daridorexant AUC of >50% |
Avoid concomitant use |
|
Rosuvastatin |
Daridorexant decreased rosuvastatin AUC by approximately 10% |
No dosage adjustment recommended |
Daridorexant Pharmacokinetics
Absorption
Bioavailability
Exposure is dose-proportional at oral dosages of 25–50 mg.
Pharmacokinetic profile is similar following multiple-dose and single-dose administration with no accumulation observed.
Peak plasma concentrations attained within 1–2 hours following oral administration.
Absolute oral bioavailability is 62%.
Food
High-fat, high-calorie meal in healthy subjects delays time to maximum plasma concentrations by 1.3 hours and decreases maximum plasma concentrations by 16% but does not substantially affect AUC.
Special Populations
Age, sex, race, body size, and mild to severe renal impairment have no clinically important effect on daridorexant pharmacokinetics.
Pharmacokinetic profile in patients with insomnia similar to that in healthy subjects.
In patients with moderate hepatic impairment (Child-Pugh score 7–9), systemic exposure increased by approximately 60%. Not studied in severe hepatic impairment.
Distribution
Plasma Protein Binding
99.7%.
Elimination
Metabolism
Undergoes extensive metabolism. Primarily metabolized by CYP3A4 (89%); minimal metabolism (<3%) by other CYP isoenzymes.
Metabolites are not pharmacologically active.
Elimination Route
Excreted in feces (approximately 57%) and in urine (approximately 28%), primarily as metabolites; trace amounts of parent drug excreted in feces and urine.
Half-life
Approximately 8 hours.
Special Populations
Dialysis unlikely to effectively remove daridorexant since drug is highly protein bound.
In patients with moderate hepatic impairment (Child-Pugh score 7–9), half-life is increased approximately 2.1-fold.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted to 15–30°C).
Actions
-
Antagonist at orexin-1 and orexin-2 receptors. Blockade of orexin A and B at these receptors is thought to suppress wake drive and promote sleep.
-
The orexin neuropeptide signaling system plays a role in promoting and maintaining wakefulness. Loss of orexin-producing neurons and decreased CSF orexin concentrations are associated with narcolepsy, while increased orexin activity may be associated with insomnia.
Advice to Patients
-
Advise patients to take daridorexant only once per night within 30 minutes of going to bed and only when able to stay in bed for ≥7 hours before being active again. Advise patients that taking daridorexant with or immediately after a meal may delay its effect.
-
Advise patients to not take daridorexant if alcohol has been consumed.
-
Inform patients that daridorexant can cause CNS depressant effects and impair daytime wakefulness even when used as prescribed. CNS depressant effects may increase the risk of falls in some patients. The risk of daytime impairment is increased if daridorexant is taken with less than a full night of sleep remaining or if a higher than recommended dose is taken; patients should be cautioned to avoid driving or other activities requiring complete mental alertness if the drug is taken under these circumstances.
-
Advise patients to be alert to and immediately report worsening depression or suicidal ideation.
-
Inform patients and their families that sleep paralysis, hypnagogic/hypnopompic hallucinations, and mild cataplexy-like symptoms may occur.
-
Advise patients of the risk of complex sleep behaviors, including sleep-walking, sleep-driving, preparing and eating food, making phone calls, or having sex while not being fully awake. Advise patients to discontinue daridorexant and immediately contact a clinician if a complex sleep behavior occurs.
-
Inform patients about the abuse potential of the drug. Advise patients to not increase the dose unless otherwise instructed by a clinician and to inform a clinician if insomnia worsens or does not improve.
-
Advise women to inform their clinicians if they are or plan to become pregnant or plan to breast-feed. Advise patients of the existence of a pregnancy registry that monitors pregnancy outcomes in women exposed to the drug during pregnancy.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant or past illnesses (e.g., depression, substance abuse, sleep apnea).
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Subject to control under the Federal Controlled Substances Act of 1970 as a schedule IV (C-IV) drug.
|
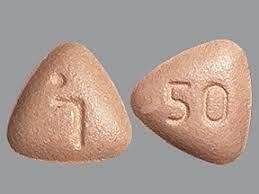
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
25 mg (of daridorexant) |
Quviviq |
Idorsia |
|
50 mg (of daridorexant) |
Quviviq |
Idorsia |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 26, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Quviviq vs. Ambien: How do they compare?
- What is the mechanism of action for Quviviq?
- How do I get and use a Quviviq coupon or savings card?
More about daridorexant
- Check interactions
- Compare alternatives
- Reviews (174)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous anxiolytics, sedatives and hypnotics
- Breastfeeding
- En español