Clarithromycin (Monograph)
Brand name: Biaxin
Drug class: Other Macrolides
- Antimycobacterial Agents
Introduction
Antibacterial; macrolide antibiotic.1
Uses for Clarithromycin
Acute Otitis Media (AOM)
Treatment of AOM caused by H. influenzae, M. catarrhalis, or S. pneumoniae.1 431
Not a drug of first choice; considered an alternative for patients with a history of type I penicillin hypersensitivity.396 431 May not be effective for AOM that fails to respond to amoxicillin since S. pneumoniae resistant to amoxicillin also may be resistant to clarithromycin.423
Pharyngitis and Tonsillitis
Treatment of pharyngitis or tonsillitis caused by susceptible Streptococcus pyogenes (group A β-hemolytic streptococci).1 2 19 24 25 62 63 143 Generally effective in eradicating S. pyogenes from the nasopharynx, but efficacy in the prevention of subsequent rheumatic fever has not been established to date.1
CDC, AAP, IDSA, AHA, and others recommend oral penicillin V or IM penicillin G benzathine as treatments of choice;107 109 110 396 oral cephalosporins and oral macrolides considered alternatives.107 109 110 396 Amoxicillin sometimes used instead of penicillin V, especially for young children.109 396
Consider that strains of S. pyogenes resistant to macrolides are common in some areas of the world (e.g., Japan, Finland) and clarithromycin-resistant strains have been reported in the US.396 446 461 (See Selection and Use of Anti-infectives under Cautions.)
Respiratory Tract Infections
Treatment of acute maxillary sinusitis caused by Haemophilus influenzae, Moraxella catarrhalis, or S. pneumoniae.1 2 26 144
Treatment of acute bacterial exacerbations of chronic bronchitis caused by H. influenzae, H. parainfluenzae, M. catarrhalis, or S. pneumoniae.1 56
Treatment of mild to moderate community-acquired pneumonia (CAP) caused by H. influenzae, Mycoplasma pneumoniae, Chlamydophila pneumoniae (Chlamydia pneumoniae), S. pneumoniae,1 29 30 46 47 56 96 121 130 131 132 133 H. parainfluenzae, or M. catarrhalis.1
Treatment of Legionnaires’ disease† [off-label] caused by Legionella pneumophila.13 447 448 Drugs of choice are macrolides (usually azithromycin) or fluoroquinolones with or without rifampin.13 447 448 449 450 450
Treatment of pertussis† [off-label] caused by Bordetella pertussis.393 396 452 454 Erythromycin traditionally has been drug of choice for treatment and postexposure prophylaxis of pertussis,396 452 454 but other macrolides (azithromycin, clarithromycin) appear to be as effective and may be associated with better compliance because they are better tolerated.396 452 454
Skin and Skin Structure Infections
Treatment of uncomplicated skin or skin structure infections caused by Staphylococcus aureus or S. pyogenes.1 56 57 136 137 138 139 140
Helicobacter pylori Infection and Duodenal Ulcer Disease
Treatment of Helicobacter pylori infection and duodenal ulcer disease (active or 1-year history of duodenal ulcer);1 335 353 377 378 eradication of H. pylori has been shown to reduce the risk of duodenal ulcer recurrence.1 335 353 377 378
Used in a multidrug regimen that includes amoxicillin, clarithromycin, and either lansoprazole or omeprazole (triple therapy).1 335 353 377 378 393 Also used with omeprazole (dual therapy) or ranitidine bismuth citrate (dual therapy).1 324
Bartonella Infections
Treatment of infections caused by B. henselae † [off-label] (e.g., cat scratch disease, bacillary angiomatosis, peliosis hepatitis).444 465
Cat scratch disease generally self-limited in immunocompetent individuals and may resolve spontaneously in 2–4 months; some clinicians suggest that anti-infectives be considered for acutely or severely ill patients with systemic symptoms, particularly those with hepatosplenomegaly or painful lymphadenopathy, and such therapy probably is indicated in immunocompromised patients.396 465
Anti-infectives also indicated in patients with B. henselae infections who develop bacillary angiomatosis, neuroretinitis, or Parinaud’s oculoglandular syndrome.396
Optimum regimens have not been identified; some clinicians recommend azithromycin, clarithromycin, ciprofloxacin, erythromycin, doxycycline, rifampin, co-trimoxazole, gentamicin, or third generation cephalosporins.393 396 444
Cryptosporidiosis
May decrease incidence of cryptosporidiosis† [off-label] in HIV-infected adults.105 111 204 Anti-infectives may suppress the infection, but none has been found to reliably eradicate Cryptosporidium.105 106 444 445 CDC, NIH, IDSA, and others state that the most appropriate treatment for cryptosporidiosis in HIV-infected individuals is the use of potent antiretroviral agents (to restore immune function) and symptomatic treatment of diarrhea.105 106 444 445
Lyme Disease
Alternate for treatment of early Lyme disease† [off-label].290 388 389 387 390 391 392 394 395 396 397 398 427 428 IDSA, AAP, and others recommend doxycycline, amoxicillin, or cefuroxime;345 393 396 427 428 429 macrolides may be less effective than these first-line agents.290 345 388 389 390 391 392 393 394 395 396 397 398 427 428
Mycobacterial Infections
Primary prevention (primary prophylaxis) of Mycobacterium avium complex (MAC) bacteremia or disseminated infections in adults, adolescents, and children with advanced HIV infection.1 201 203 204 210 293 350 Recommended by USPHS/IDSA as a drug of choice for primary prevention of MAC in HIV-infected patients.204
Treatment of disseminated MAC infection in HIV-infected adults, adolescents, and children.1 7 172 173 175 176 177 178 185 187 211 293 350 444 445 ATS, CDC, NIH, IDSA, and others recommend a regimen of clarithromycin (or azithromycin) and ethambutol and state that consideration may be given to adding a third drug (preferably rifabutin).201 215 221 350 369 393 444 445 Clarithromycin usually the preferred macrolide for initial treatment; azithromycin can be substituted if clarithromycin cannot be used because of drug interactions or intolerance and is preferred in pregnant women.444 445
Prevention of recurrence (secondary prophylaxis) of disseminated MAC infection in HIV-infected adults, adolescents, and children.1 175 177 185 204 350 444 445 USPHS/IDSA, CDC, NIH, IDSA, and others recommend a macrolide (clarithromycin or azithromycin) given with ethambutol (with or without rifabutin).204 444 445 Azithromycin usually the preferred macrolide for use in conjunction with ethambutol for secondary prophylaxis in pregnant women.204 444
Treatment of pulmonary MAC infections in HIV-negative patients†.350 451 A multiple-drug regimen of clarithromycin (or azithromycin), ethambutol, and either rifabutin or rifampin usually recommended.350
Treatment of M. kansasii infections†; an alternative agent.350 393
Treatment of cutaneous infections caused by M. abscessus or Mycobacterium chelonae †.188 350 393 462
Treatment of cutaneous M. marinum infection†.189 350 393
Toxoplasmosis
Has been used in conjunction with pyrimethamine for treatment of encephalitis caused by Toxoplasma gondii † in HIV-infected patients;2 48 444 not a preferred or alternative agent.444 445 464 CDC, NIH, IDSA, and others usually recommend pyrimethamine in conjunction with sulfadiazine and leucovorin for treatment of toxoplasmosis in adults and children, especially immunocompromised patients (e.g., HIV-infected individuals).444 445 464
Prevention of Bacterial Endocarditis
Alternative for prevention of α-hemolytic (viridans group) streptococcal endocarditis† in penicillin-allergic patients undergoing certain dental, oral, respiratory tract, or esophageal procedures who have cardiac conditions that put them at high or moderate risk.345
Consult most recent AHA recommendations for specific information on which cardiac conditions are associated with high or moderate risk of endocarditis and which procedures require prophylaxis.345
Clarithromycin Dosage and Administration
Administration
Oral Administration
Conventional tablets and oral suspension: Administer orally without regard to meals.1 2 3 Oral suspension may be administered with milk.1 2 3
Extended-release tablets: Administer orally with food.1 2 3 Should be swallowed whole and not chewed, broken, or crushed.1
Reconstitution
Reconstitute granules for oral suspension at the time of dispensing by adding the amount of water specified on the bottle in two portions; agitate well after each addition.1 Agitate well just prior to use.1
Dosage
Extended-release tablets may be used only for treatment of acute maxillary sinusitis, acute bacterial exacerbations of chronic bronchitis, and CAP in adults; safety and efficacy not established for treatment of other infections in adults or for use in pediatric patients.1
Pediatric Patients
Acute Otitis Media (AOM)
Oral
7.5 mg/kg every 12 hours for 10 days.1 431
Pharyngitis and Tonsillitis
Oral
7.5 mg/kg every 12 hours for 10 days.1
Respiratory Tract Infections
Acute Bacterial Sinusitis
Oral7.5 mg/kg every 12 hours for 10 days.1
Community-acquired Pneumonia (CAP)
Oral7.5 mg/kg every 12 hours for 10 days.1
Pertussis†
Oral15–20 mg/kg daily in 2 divided doses (up to 1 g daily) for 7 days.396 7.5 mg/kg twice daily for 7 days has been used in children 1 month to 16 years of age.454
Skin and Skin Structure Infections
Oral
7.5 mg/kg every 12 hours for 10 days.1
Bartonella Infections†
Cat Scratch Disease Caused by Bartonella henselae†
Oral500 mg daily for 4 weeks.465
Bartonella Infections in HIV-infected Individuals†
OralAdolescents: 500 mg twice daily for ≥3 months recommended by CDC, NIH, and IDSA.444 If relapse occurs, consider lifelong secondary prophylaxis (chronic maintenance therapy) with erythromycin or doxycycline.444
Lyme Disease†
Oral
7.5 mg/kg (up to 500 mg) twice daily for 14–21 days for treatment of early localized or early disseminated disease.428
Mycobacterium avium Complex (MAC) Infections
Primary Prevention of MAC in Children with Advanced HIV Infection
Oral7.5 mg/kg (up to 500 mg) every 12 hours.1 204
USPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <750/mm3 in those <1 year, <500/mm3 in those 1–2 years, <75/mm3 in those 2–6 years, or <50/mm3 in those ≥6 years of age.204
Primary Prevention of MAC in Adolescents with Advanced HIV Infection
OralUSPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <50/mm3.204 May be discontinued if there is immune recovery in response to antiretroviral therapy and an increase in CD4+ T-cell count to >100/mm3 sustained for ≥3 months.204 Reinitiate prophylaxis if CD4+ T-cell count decreases to <50–100/mm3.204
Treatment of Disseminated MAC in HIV-infected Children
OralManufacturer recommends 7.5 mg/kg (up to 500 mg) every 12 hours.1
CDC, NIH, and IDSA recommend 7.5–15 mg/kg (maximum 500 mg) twice daily in conjunction with ethambutol (15–25 mg/kg once daily [up to 1 g daily]) with or without rifabutin (10–20 mg/kg once daily [up to 300 mg daily]).445
Treatment of Disseminated MAC in HIV-infected Adolescents
Oral500 mg every 12 hours444 in conjunction with ethambutol (15 mg/kg daily) with or without a third drug (e.g., rifabutin 300 mg once daily) recommended by CDC, NIH, and IDSA.444 Higher dosage not recommended since such dosage has been associated with reduced survival in clinical studies.171 201 204 211 214 223 224 351
Prevention of MAC Recurrence in HIV-infected Children
Oral7.5 mg/kg (maximum 500 mg) twice daily1 204 in conjunction with ethambutol (15 mg/kg [maximum 900 mg] once daily) with or without rifabutin (5 mg/kg [maximum 300 mg] once daily).204
Secondary prophylaxis to prevent MAC recurrence in HIV-infected children usually continued for life.204 445 The safety of discontinuing secondary MAC prophylaxis in children whose CD4+ T-cell count increases in response to antiretroviral therapy has not been studied.204 445
Prevention of MAC Recurrence in HIV-infected Adolescents
Oral500 mg every 12 hours1 204 444 in conjunction with ethambutol (15 mg/kg once daily) with or without rifabutin (300 mg once daily).204 444
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adolescents.204 USPHS/IDSA states that consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 sustained for ≥6 months.204 444
Treatment of Cutaneous Mycobacterium abscessus Infections†
Oral15 mg/kg daily (with or without incision and drainage of lesions) has been used in children 1–15 years of age.462
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental, Oral, Respiratory Tract, or Esophageal Procedures
Oral15 mg/kg as a single dose given 1 hour prior to the procedure.345
Adults
Pharyngitis and Tonsillitis
Oral
250 mg every 12 hours for 10 days.1
Respiratory Tract Infections
Acute Bacterial Sinusitis
OralConventional tablets or oral suspension: 500 mg every 12 hours for 14 days.1
Extended-release tablets: 1 g (two 500-mg extended release tablets) once daily for 14 days.1
Acute Exacerbations of Chronic Bronchitis
OralConventional tablets or oral suspension: 500 mg every 12 hours for 7–14 days for H. influenzae,1 500 mg every 12 hours for 7 days for H. parainfluenzae,1 or 250 mg every 12 hours for 7–14 days for M. catarrhalis or S. pneumoniae.1
Extended-release tablets: 1 g (two 500-mg extended-release tablets) once daily for 7 days.1
Community-acquired Pneumonia (CAP)
OralConventional tablets or oral suspension: 250 mg every 12 hours for 7 days for H. influenzae or for 7–14 days for S. pneumoniae, C. pneumoniae, or M. pneumoniae.1
Extended-release tablets: 1 g (two 500-mg extended-release tablets) once daily for 7 days.1
Legionnaires’ Disease†
OralConventional tablets or oral suspension: 500 mg twice daily.447 448 Usual duration is 10 days for mild to moderate infections in immunocompetent patients;447 longer duration of treatment (3 weeks) may be necessary to prevent relapse, especially in those with more severe infections or with underlying comorbidity or immunodeficiency.447 448
Skin and Skin Structure Infections
Oral
Conventional tablets or oral suspension: 250 mg every 12 hours for 7–14 days.1
Helicobacter pylori Infection and Duodenal Ulcer Disease
Oral
Conventional tablets or oral suspension: 500 mg twice daily for 10 or 14 days given in conjunction with amoxicillin and lansoprazole (triple therapy);1 353 378 500 mg twice daily for 10 days given in conjunction with amoxicillin and omeprazole (triple therapy);377 500 mg 3 times daily for 14 days given in conjunction with omeprazole or ranitidine bismuth citrate (dual therapy).1 377
Bartonella Infections†
Cat Scratch Disease Caused by Bartonella henselae†
OralConventional tablets or oral suspension: 500 mg daily for 4 weeks.465
Bartonella Infections in HIV-infected Individuals†
OralConventional tablets or oral suspension: 500 mg twice daily for ≥3 months recommended by CDC, NIH, and IDSA.444 If relapse occurs, consider lifelong secondary prophylaxis (chronic maintenance therapy) with erythromycin or doxycycline.444
Lyme Disease†
Oral
Conventional tablets or oral suspension: 500 mg twice daily for 14–21 days for treatment of early localized or early disseminated disease.428
Mycobacterial Infections
Primary Prevention of MAC in Adults with Advanced HIV Infection
OralConventional tablets or oral suspension: 500 mg every 12 hours.1 204
USPHS/IDSA recommends initiation of primary prophylaxis if CD4+ T-cell count is <50/mm3.204 May be discontinued if there is immune recovery in response to antiretroviral therapy and an increase in CD4+ T-cell count to >100/mm3 sustained for ≥3 months.204 Reinitiate prophylaxis if CD4+ T-cell count decreases to <50–100/mm3.204
Treatment of Disseminated MAC in HIV-infected Adults
OralConventional tablets or oral suspension: 500 mg every 12 hours1 444 in conjunction with ethambutol (15 mg/kg daily) with or without a third drug (e.g., rifabutin 300 mg once daily).444 Higher dosage not recommended since such dosage has been associated with reduced survival in clinical studies.171 201 204 211 214 223 224 351
Prevention of MAC Recurrence in HIV-infected Adults
OralConventional tablets or oral suspension: 500 mg every 12 hours1 204 444 in conjunction with ethambutol (15 mg/kg once daily) with or without rifabutin (300 mg once daily).204 444
Secondary prophylaxis to prevent MAC recurrence usually continued for life in HIV-infected adults.204 USPHS/IDSA states that consideration can be given to discontinuing such prophylaxis after ≥12 months in those who remain asymptomatic with respect to MAC and have an increase in CD4+ T-cell count to >100/mm3 sustained for ≥6 months.204 444
Treatment of MAC in HIV-negative Adults†
OralConventional tablets or oral suspension: 500 mg every 12 hours in conjunction with ethambutol and rifabutin or rifampin.350
Mycobacterium abscessus or M. chelonae Infections†
OralConventional tablets or oral suspension: 0.5–1 g twice daily for 6 months.188 462
M. marinum Infections†
OralConventional tablets or oral suspension: 500 mg twice daily for at least 3 months.350
Prevention of Bacterial Endocarditis†
Patients Undergoing Certain Dental, Oral, Respiratory Tract, or Esophageal Procedures
OralConventional tablets or oral suspension: 500 mg as a single dose given 1 hour prior to the procedure.345
Special Populations
Hepatic Impairment
No dosage adjustment required.1 56 97 98
Renal Impairment
If Clcr <30 mL/minute, reduce dose by 50% or double dosing interval.1 2 126 Alternatively (for conventional tablets or oral suspension), 500 mg initially followed by 250 mg twice daily (if the usual dosage in adults with normal renal function is 500 mg twice daily) or 250 mg daily (if the usual dosage in adults with normal renal function is 250 mg twice daily).97 121
Geriatric Patients
No dosage adjustments except those related to renal impairment.1 97 121 126 128 (See Renal Impairment under Dosage and Administration.)
Cautions for Clarithromycin
Contraindications
-
Known hypersensitivity to clarithromycin, erythromycin, any macrolide, or any ingredient in the formulation.1 353
Warnings/Precautions
Warnings
Increased Mortality
Increased risk of all-cause mortality reported during long-term follow-up of patients with coronary heart disease who received a 2-week course of clarithromycin in a randomized, placebo-controlled study.467 468 469 470 Variable results regarding effect of clarithromycin on risk of death or other heart-related adverse effects reported in other limited observational studies.467 468 470 A possible mechanism by which clarithromycin may increase the risk of death in patients with cardiovascular disease unknown.467 468 470
Consider risk of all-cause mortality when weighing risks and potential benefits of the drug in all patients, particularly those with cardiovascular disease.467 468 Even if only a short course of clarithromycin is indicated, consider other available antibiotics in those with heart disease.468 Not indicated for the treatment of coronary artery disease.467
Fetal/Neonatal Morbidity
Animal studies indicate adverse effects on pregnancy outcome and/or embryofetal development.1 Use during pregnancy only when safer drugs cannot be used or are ineffective.1
Superinfection/Clostridium difficile-associated Colitis
Possible emergence and overgrowth of nonsusceptible bacteria or fungi with prolonged therapy.1 Institute appropriate therapy if superinfection occurs.1
Treatment with anti-infectives may permit overgrowth of clostridia.1 Consider Clostridium difficile-associated diarrhea and colitis (antibiotic-associated pseudomembranous colitis) if diarrhea develops and manage accordingly.1 400 401 402 403 404
Sensitivity Reactions
Hypersensitivity and Dermatologic Reactions
Possible allergic reactions (e.g., mild urticaria and skin eruptions).1 2 29 47 370 371 Severe reactions (e.g., anaphylaxis, Stevens-Johnson syndrome, toxic epidermal necrolysis) reported rarely.1 370 371
General Precautions
Hepatic Effects
Severe, reversible hepatic dysfunction (including cholestasis, with or without jaundice)1 and hepatomegaly2 29 47 reported.1
Fatal hepatic failure occurred in association with serious underlying disease and/or concomitant drugs.1
Resistance in Helicobacter pylori
Increased risk of developing clarithromycin resistance if used as the sole anti-infective agent in regimens for treatment of H. pylori infection.1 If therapy fails, perform in vitro susceptibility testing.1 197 377 378 Do not use clarithromycin if H. pylori is resistant.1 197 377 378
Cardiac Effects
Ventricular tachycardia and torsades de pointes reported rarely in patients with prolonged QT intervals.1
History of Acute Porphyria
Concomitant therapy with ranitidine bismuth citrate not recommended.1
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of clarithromycin and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.1
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing.1 In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.1
Consider that S. pyogenes (group A β-hemolytic streptococci) resistant to clarithromycin have been reported.396 446 461
Specific Populations
Pregnancy
Category C.1 (See Fetal/Neonatal Morbidity under Cautions.)
Lactation
Distributed into milk following oral administration.460 Use with caution.1
Pediatric Use
Safety and efficacy not established in children <6 months of age.1
Manufacturer states safety not established in children <20 months of age with MAC infection,1 but USPHS/IDSA recommends use of the drug for HIV-infected infants and children.204
Geriatric Use
Adverse effect profile similar to that in younger adults.1 121 126
Dosage adjustment based solely on age not required.1 97 121 126 128
Clearance may be reduced due to age-related decreases in renal function.97 98 Consider need for dosage adjustment in those with severe renal impairment. (See Renal Impairment under Dosage and Administration.)
Renal Impairment
Increased half-life.1 2 56 97 98 Dosage adjustment may be necessary.1 2 126 (See Renal Impairment under Dosage and Administration.)
Concomitant therapy with ranitidine bismuth citrate not recommended if Clcr <25 mL/minute.1
Common Adverse Effects
GI adverse effects (diarrhea, nausea, abnormal taste, dyspepsia, abdominal pain) and headache.1
Drug Interactions
Clarithromycin is metabolized by and inhibits CYP3A4.1
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with substrates, inhibitors, or inducers of CYP3A4 are likely.1
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amprenavir |
Increased amprenavir concentrations and AUC;437 438 439 possible decreased clarithromycin concentrations and decreased 14-hydroxyclarithromycin concentrations and AUC439 |
|
|
Anticoagulants, oral |
Increased anticoagulant effect1 |
Monitor PT carefully1 |
|
Antihistamines (astemizole, terfenadine) |
Increased plasma concentrations of astemizole or terfenadine; prolonged QT interval and serious cardiac arrhythmias 1 150 154 155 157 158 159 161 162 163 164 166 167 352 |
|
|
Antimycobacterials (rifabutin) |
Potential inhibition of rifabutin metabolism373 and induction of clarithromycin metabolism;227 373 possible increased incidence of uveitis with concomitant rifabutin and clarithromycin 373 374 375 376 |
|
|
Atazanavir |
Increased atazanavir plasma concentrations;430 increased clarithromycin plasma concentrations and decreased 14-hydroxyclarithromycin plasma concentrations;430 437 increased clarithromycin concentrations may cause QTc prolongation430 437 |
Consider reducing clarithromycin dosage by 50%;430 437 consider alternative to clarithromycin430 437 for indications other than Mycobacterium avium complex (MAC)430 |
|
Benzodiazepines (alprazolam, midazolam, triazolam) |
Potential decreased clearance of midazolam or triazolam and increased pharmacologic effects of the benzodiazepines1 Somnolence and confusion reported with clarithromycin and triazolam1 |
|
|
Carbamazepine |
Increased carbamazepine plasma concentrations and carbamazepine toxicity (i.e., drowsiness, dizziness, ataxia)2 51 338 |
Use with caution; consider reducing carbamazepine dosage and/or monitoring plasma carbamazepine concentrations1 338 |
|
Cisapride |
Increased cisapride plasma concentrations;339 prolonged QT interval and serious cardiac arrhythmias; some fatalities1 |
Contraindicated1 |
|
Colchicine |
Possible increased risk of colchicine toxicity when used concomitantly with clarithromycin, especially in elderly patients and/or patients with renal impairment1 463 |
Some clinicians state colchicine and clarithromycin should not be used concomitantly463 |
|
Darifenacin |
Possible pharmacokinetic interaction455 |
Manufacturer of darifenacin states darifenacin dosage should not exceed 7.5 mg daily in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin)455 |
|
Delavirdine |
Increased clarithromycin concentrations and AUC;112 437 increased delavirdine concentrations437 |
Dosage adjustment not needed in those with normal renal function;112 437 reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute112 |
|
Didanosine |
No clinically important pharmacokinetic interactions 1 |
|
|
Digoxin |
Increased serum digoxin concentrations and digoxin toxicity (including potentially fatal arrhythmias)1 |
Monitor serum digoxin concentrations carefully1 |
|
Disopyramide |
Potential increased half-life of disopyramide340 and risk of prolonged QT interval and serious cardiac arrhythmias1 340 |
Monitor ECGs and serum disopyramide concentrations1 |
|
Efavirenz |
Decreased clarithromycin AUC and peak plasma concentrations;435 437 increased 14-hydroxyclarithromycin AUC and peak plasma concentrations;435 no effect on AUC of efavirenz;435 rash reported with concomitant administration435 |
Dosage adjustment of efavirenz not recommended; monitor for efficacy of the macrolide437 or consider use of an alternative anti-infective435 437 |
|
Ergot alkaloids (ergotamine, dihydroergotamine) |
Acute ergot toxicity (vasospasm and ischemia of extremities and other tissues, including CNS)1 225 |
Concomitant use contraindicated1 |
|
Erlotinib |
Possible pharmacokinetic interaction456 |
Manufacturer of erlotinib recommends caution in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin);456 consider reducing erlotinib dosage if severe adverse effects occur456 |
|
Eszopiclone |
Possible pharmacokinetic interaction457 |
Manufacturer of eszopiclone recommends eszopiclone dosage be reduced in patients receiving a potent CYP3A4 inhibitor (e.g., clarithromycin);457 initial eszopiclone dosage should be <1 mg, but may be increased to 2 mg if clinically indicated457 |
|
Fluconazole |
Increased clarithromycin plasma concentrations1 |
|
|
Fosamprenavir |
Studies using amprenavir indicate possible increased amprenavir concentrations and AUC437 440 |
Not considered clinically important;441 dosage adjustments not recommended437 |
|
Hydroxymethylglutaryl-CoA (HMG-CoA) reductase inhibitors |
Increased HMG-CoA reductase inhibitor plasma concentrations and potential for rhabdomyolysis1 |
|
|
Indinavir |
Increased indinavir and clarithromycin concentrations437 443 |
Indinavir manufacturer states appropriate dosages for concomitant use with respect to safety and efficacy not established;443 some experts state dosage adjustments not needed437 |
|
Lopinavir |
Reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute433 |
|
|
Nevirapine |
Decreased clarithromycin AUC and peak plasma concentration;436 437 increased 14-hydroxyclarithromycin AUC and peak plasma concentration;436 increased nevirapine concentrations437 |
Monitor for efficacy of the macrolide or use an alternative anti-infective436 437 |
|
Omeprazole |
Increased concentrations of clarithromycin, 14-hydroxyclarithromycin, and omeprazole194 196 |
|
|
Pimozide |
Potential increased pimozide plasma concentrations and risk of prolonged QT interval and serious cardiac arrhythmias1 271 272 |
|
|
Quinidine |
Risk of prolonged QT interval and serious cardiac arrhythmias1 |
Monitor ECGs and serum quinidine concentrations1 |
|
Ranitidine |
Increased plasma ranitidine concentrations and increased 14-hydroxyclarithromycin concentrations;1 not considered clinically important1 |
|
|
Ritonavir |
Increased AUC and peak plasma concentration of ritonavir and of clarithromycin;1 434 decreased AUC and peak plasma concentration of 14-hydroxyclarithromycin1 434 |
Dosage adjustment not needed in patients with normal renal function; reduce clarithromycin dosage by 50% if Clcr is 30–60 mL/minute; reduce clarithromycin dosage by 75% if Clcr is <30 mL/minute1 434 |
|
Saquinavir |
Increased clarithromycin AUC and plasma concentrations; decreased 14-hydroxyclarithromycin AUC; increased AUC and plasma concentrations of saquinavir432 437 442 |
Dosage adjustments may not be needed437 if used concomitantly for a limited time432 442 For those receiving ritonavir-boosted saquinavir, manufacturer of saquinavir states modification of dosage not necessary in those with normal renal function but clarithromycin dosage should be reduced 50% in those with Clcr 30–60 mL/minute and reduced 75% in those with Clcr <30 mL/minute432 442 |
|
Sildenafil |
Potential increased exposure to sildenafil1 |
Consider reducing sildenafil dosage1 |
|
Theophylline |
Monitor serum theophylline concentrations in those receiving high theophylline dosage or with baseline in the upper therapeutic range;1 adjust theophylline dosage as needed when clarithromycin is initiated or discontinued121 126 |
|
|
Zidovudine |
Clarithromycin Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed from GI tract.1 2 56 97 98 With conventional tablets or oral suspension, peak serum concentrations within 1–4 hours.2 56 With extended-release tablets, peak serum concentrations within 5–8 hours.1
Absolute bioavailability of conventional tablets is about 50–55%;1 2 53 56 98 absolute bioavailability may be an underestimate of systemic activity because of rapid first-pass metabolism and an active metabolite (14-hydroxyclarithromycin).98
Food
With conventional tablets, food causes a slight delay in onset of clarithromycin absorption but extent of absorption is unaffected.1 56 With extended-release tablets, food increases the extent of absorption by 30%.1
Distribution
Extent
Clarithromycin and 14-hydroxyclarithromycin distributed into most body tissues and fluids1 2 54 55 56 68 in concentrations greater than serum concentrations.1 56 68
Distributed into CSF following oral administration.458
Not known whether clarithromycin is distributed into milk.1
Plasma Protein Binding
Elimination
Metabolism
Extensively metabolized in the liver, principally by oxidative N-demethylation and hydroxylation.98 At least 7 metabolites identified; 14-hydroxyclarithromycin is the principal metabolite in serum and the only one with substantial antibacterial activity.1 2 3 4 56 97
Elimination Route
Eliminated by both renal and nonrenal mechanisms;1 2 3 56 97 98 approximately 38% of a dose excreted in urine and 40% in feces.1 2 4 126
Half-life
Special Populations
Renal impairment decreases clearance of clarithromycin and 14-hydroxyclarithromycin.1 2 56 70 97 98
Hepatic impairment reduces formation of the active metabolite; however, an increase in renal clearance of the parent drug obviates the need for a dosage reduction unless renal impairment also is present.1 56 97 98
Stability
Storage
Oral
For Suspension
Granules for oral suspension: Tight container at 15–30°C.1 Following reconstitution, do not refrigerate.1
Tablets
Conventional 250-mg tablets: Tight, light-resistant container at 15–30°C and protect from light.1
Conventional 500-mg tablets: Tight container at 20–25°C.1
Extended-release tablets: 20–25°C (may be exposed to 15–30°C).1
Clarithromycin Combinations
Kit containing clarithromycin, amoxicillin, and lansoprazole: 20–25°C.353
Actions and Spectrum
-
Usually bacteriostatic,2 12 83 84 85 but may be bactericidal against highly susceptible organisms or when present in high concentrations.2 12 84 92 94
-
Like other macrolides, inhibits protein synthesis in susceptible organisms by binding to 50S ribosomal subunits.1 2 56
-
Spectrum of activity includes many gram-positive1 2 80 83 84 85 86 92 94 95 and -negative1 2 12 16 18 56 80 83 84 85 86 92 96 aerobic bacteria, many anaerobic bacteria,1 83 121 some mycobacteria,2 32 34 35 36 77 86 87 88 and some other organisms including Mycoplasma,2 37 47 76 93 Ureaplasma,2 37 76 93 Chlamydia,1 2 17 38 39 56 61 91 96 Toxoplasma,2 41 42 43 and Borrelia.97 104
-
In vitro activity similar to75 84 86 92 or greater than that of erythromycin against erythromycin-susceptible organisms.2 56 83 94
-
The principal metabolite (14-hydroxyclarithromycin) has clinically important antimicrobial activity.1
-
Gram-positive aerobes: Active in vitro and in clinical infections against Staphylococcus aureus,1 S. pneumoniae,1 and S. pyogenes (group A β-hemolytic streptococci),1 Enterococci (e.g., Enterococcus faecalis) and oxacillin-resistant (methicillin-resistant) staphylococci are resistant.1
-
Gram-negative aerobes: Active in vitro and in clinical infections against Haemophilus influenzae,1 H. parainfluenzae,1 and Moraxella catarrhalis.1
-
Other organisms: Active in vitro and in clinical infections against C. pneumoniae and 1 M. pneumoniae.1 Also active against MAC.1
-
Organisms resistant to erythromycin generally resistant to clarithromycin.2 45
-
Complete cross-resistance occurs between azithromycin and clarithromycin in MAC.350
Advice to Patients
-
Advise patients that antibacterials (including clarithromycin) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).1
-
Importance of completing full course of therapy, even if feeling better after a few days.1
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with clarithromycin or other antibacterials in the future.1
-
Importance of taking clarithromycin extended-release tablets with food;1 clarithromycin immediate-release tablets and oral suspension can be taken without regard to meals.1
-
Advise patients of the importance of informing clinician if they have heart disease, especially when an anti-infective is being prescribed, and the importance of seeking medical attention if they experience symptoms of a heart attack or stroke (e.g., chest pain, shortness of breath, pain or weakness in one part or side of the body, slurred speech).468
-
Importance of reporting persistent or worsening symptoms of infection.1
-
Importance of not refrigerating oral suspension.1
-
Importance of discontinuing therapy and informing clinician if an allergic reaction occurs.1
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of advising patients of other important precautionary information.1 (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension |
125 mg/5 mL* |
Clarithromycin for Suspension |
|
|
250 mg/5 mL* |
Clarithromycin for Suspension |
|||
|
Tablets, film-coated |
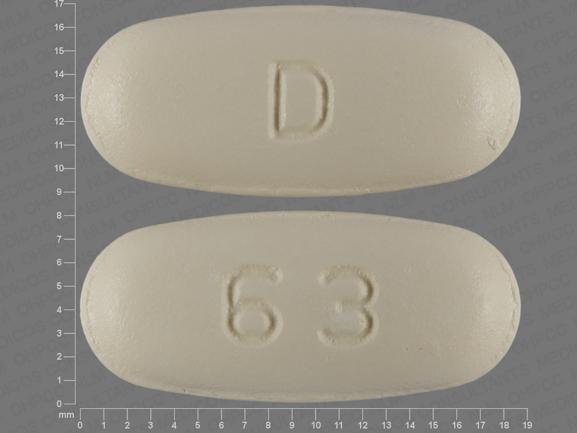
250 mg* |
Biaxin Filmtab |
AbbVie |
|
|
Clarithromycin Tablets |
||||
|
500 mg* |
Biaxin Filmtab |
AbbVie |
||
|
Clarithromycin Tablets |
||||
|
Tablets, extended-release, film-coated |
500 mg* |
Clarithromycin Tablets Extended-release |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Kit |
4 Capsules, Amoxicillin (trihydrate) 500 mg (of amoxicillin) (Trimox) 2 Capsules, delayed-release (containing enteric-coated granules), Lansoprazole, 30 mg (Prevacid) 2 Tablets, film-coated, Clarithromycin, 500 mg (Biaxin Filmtab) 4 Capsules, Amoxicillin (trihydrate) 500 mg (of amoxicillin) 2 Capsules, delayed-release (containing enteric-coated granules), Lansoprazole, 30 mg 2 Tablets, film-coated, Clarithromycin, 500 mg |
Prevpac |
Takeda Pharmaceuticals |
|
Amoxicillin, Clarithromycin, and Lansoprazole |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions December 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Abbott Laboratories. Biaxin (clarithromycin) Filmtab tablets, XL Filmtab extended-release tablets, and granules for oral suspension prescribing information. North Chicago, IL; 2005 Jan.
2. Piscitelli SC, Danziger LH, Rodvold KA. Clarithromycin and azithromycin: new macrolide antibiotics. Clin Pharm. 1992; 11:137-52. https://pubmed.ncbi.nlm.nih.gov/1312921
3. Abbott Laboratories. Biaxin (clarithromycin) product information. North Chicago, IL; 1992 Feb.
4. Ferrero JL, Bopp BA, Marsh KC et al. Metabolism and disposition of clarithromycin in man. Drug Metab Dispos. 1990; 18:441-6. https://pubmed.ncbi.nlm.nih.gov/1976065
5. Hanson CW, Bailer R, Gade E et al. Regression analysis, proposed interpretative zone size standards, and quality control guidelines for a new macrolide antimicrobial agent, A-56268 (TE-031). J Clin Microbiol. 1987; 25:1079-82. https://pubmed.ncbi.nlm.nih.gov/2954995 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC269140/
6. American Thoracic Society. Guidelines for the management of adults with community-acquired pneumonia. Diagnosis, assessment of severity, antimicrobial therapy, and prevention. Am J Resp Crit Care Med. 2001; 163:1730-54. https://pubmed.ncbi.nlm.nih.gov/11401897
7. Dautzenberg B, Truffot C, Legris S et al. Activity of clarithromycin against Mycobacterium avium infection in patients with the acquired immune deficiency syndrome: a controlled clinical trial. Am Rev Respir Dis. 1991; 144(3 Part 1):564-9. https://pubmed.ncbi.nlm.nih.gov/1832527
8. Saint-Marc T, Touraine JL. Clinical experience with a combination of clarithromycin and clofazimine in the treatment of disseminated M. avium infections in AIDS patients. Proceedings of ICAAC Chicago 1991. Abstract No. 237.
9. Dautzenberg B, St. Marc T, Averous V et al. Clarithromycin-containing regimens in the treatment of 54 AIDS patients with disseminated Mycobacterium avium intracellulare infection. Proceedings of ICAAC Chicago 1991. Abstract No. 293.
10. Kirst HA, Sides GD. New directions for macrolide antibiotics: structural modifications and in vitro activity. Antimicrob Agents Chemother. 1989; 33:1413-8. https://pubmed.ncbi.nlm.nih.gov/2684004 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172675/
11. Omura S, Tsuzuki K, Sunazuka T et al. Macrolides with gastrointestinal motor stimulating activity. J Med Chem. 1987; 30:1941-3. https://pubmed.ncbi.nlm.nih.gov/3669001
12. Fernandes PB, Bailer R, Swanson R et al. In vitro and in vivo evaluation of A-56268 (TE-031), a new macrolide. Antimicrob Agents Chemother. 1986; 30:865-73. https://pubmed.ncbi.nlm.nih.gov/2949695 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC180609/
13. Bartlett JG, Dowell SF, Mandell LA et al. Practice guidelines for the management of community-acquired pneumonia in adults. Clin Infect Dis. 2000; 31:347-82. https://pubmed.ncbi.nlm.nih.gov/10987697
14. Steigbigel NH. Erythromycin, lincomycin, and clindamycin. In: Mandell GL, Douglas RG Jr, Bennett JE, eds. Principles and practice of infectious diseases. 3rd ed. New York: Churchill Livingstone Inc; 1991:308-17.
15. Benson CA, Segreti J, Beaudette FE et al. In vitro activity of A-56268 (TE-031), a new macrolide, compared with that of erythromycin and clindamycin against selected gram-positive and gram-negative organisms. Antimicrob Agents Chemother. 1987; 31:328-30. https://pubmed.ncbi.nlm.nih.gov/2952063 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174717/
16. Hardy DJ, Hensey DM, Beyer JM et al. Comparative in vitro activities of new 14-, 15-, and 16-membered macrolides. Antimicrob Agents Chemother. 1988; 32:1710-9. https://pubmed.ncbi.nlm.nih.gov/3252753 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175956/
17. Chin NX, Neu NM, Labthavikul P et al. Activity of A-56268 compared with that of erythromycin and other oral agents against aerobic and anaerobic bacteria. Antimicrob Agents Chemother. 1987; 31:463-6. https://pubmed.ncbi.nlm.nih.gov/2953303 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174754/
18. Barry AL, Jones RN, Thornsberry C. In vitro activities of azithromycin (CP 62,993), clarithromycin (A-56268; TE-031), erythromycin, roxithromycin, and clindamycin. Antimicrob Agents Chemother. 1988; 32:752-4. https://pubmed.ncbi.nlm.nih.gov/2840016 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172265/
19. Scaglione F. Comparison of the clinical and bacteriological efficacy of clarithromycin and erythromycin in the treatment of streptococcal pharyngitis. Curr Med Res Opin. 1990; 12:25-33. https://pubmed.ncbi.nlm.nih.gov/2140547
20. Marchi E. Comparative efficacy and tolerability of clarithromycin and amoxycillin in the treatment of out-patients with acute maxillary sinusitis. Curr Med Res Opin. 1990; 12:19-24. https://pubmed.ncbi.nlm.nih.gov/2140546
21. Fraschini F. Clinical efficacy and tolerance of two new macrolides, clarithromycin and josamycin, in the treatment of patients with acute exacerbations of chronic bronchitis. J Int Med Res. 1990; 18:171-6. https://pubmed.ncbi.nlm.nih.gov/2140331
22. Straneo G, Scarpazza G. Efficacy and safety of clarithromycin versus josamycin in the treatment of hospitalized patients with bacterial pneumonia. J Int Med Res. 1990; 18:164-70. https://pubmed.ncbi.nlm.nih.gov/2140330
23. Hamedani P, Ali J, Hafeez S et al. The safety and efficacy of clarithromycin in patients with Legionella pneumonia. Chest. 1991; 100:1503-6. https://pubmed.ncbi.nlm.nih.gov/1835689
24. Levenstein JH. Clarithromycin versus penicillin in the treatment of streptococcal pharyngitis. J Antimicrob Chemother. 1991; 27(Suppl A):67-74. https://pubmed.ncbi.nlm.nih.gov/1827104
25. Bachand RT Jr. A comparative study of clarithromycin and penicillin VK in the treatment of outpatients with streptococcal pharyngitis. J Antimicrob Chemother. 1991; 27(Suppl A):75-82. https://pubmed.ncbi.nlm.nih.gov/1827105
26. Karma P, Pukander J, Penttila M et al. The comparative efficacy and safety of clarithromycin and amoxycillin in the treatment of outpatients with acute maxillary sinusitis. J Antimicrob Chemother. 1991; 27(Suppl A):83-90. https://pubmed.ncbi.nlm.nih.gov/1827106
27. Bachand RT Jr. Comparative study of clarithromycin and ampicillin in the treatment of patients with acute bacterial exacerbations of chronic bronchitis. J Antimicrob Chemother. 1991; 27(Suppl A):91-100. https://pubmed.ncbi.nlm.nih.gov/1827107
28. Aldons PM. A comparison of clarithromycin with ampicillin in the treatment of outpatients with acute bacterial exacerbation of chronic bronchitis. J Antimicrob Chemother. 1991; 27(Suppl A):101-8. https://pubmed.ncbi.nlm.nih.gov/1827095
29. Poirier R. Comparative study of clarithromycin and roxithromycin in the treatment of community-acquired pneumonia. J Antimicrob Chemother. 1991; 27(Suppl A):109-16. https://pubmed.ncbi.nlm.nih.gov/1827096
30. Anderson G, Esmonde TS, Coles S et al. A comparative safety and efficacy study of clarithromycin and erythromycin stearate in community-acquired pneumonia. J Antimicrob Chemother. 1991; 27(Suppl A):117-24. https://pubmed.ncbi.nlm.nih.gov/1827098
31. Hardy DJ, Swanson RN, Rode RA et al. Enhancement of the in vitro and in vivo activities of clarithromycin against Haemophilus influenzae by 14-hydroxy-clarithromycin, its major metabolite in humans. Antimicrob Agents Chemother. 1990; 34:1407-13. https://pubmed.ncbi.nlm.nih.gov/2143642 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175991/
32. Gelber RH, Siu P, Tsang M et al. Activities of various macrolide antibiotics against Mycobacterium leprae infection in mice. Antimicrob Agents Chemother. 1991; 35:760-3. https://pubmed.ncbi.nlm.nih.gov/1648889 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245094/
33. Franzblau SG, Hastings RC. In vitro and in vivo activities of macrolides against Mycobacterium leprae . Antimicrob Agents Chemother. 1988; 32:1758-62. https://pubmed.ncbi.nlm.nih.gov/3072920 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC176013/
34. Ji B, Perani EG, Grosset JH. Effectiveness of clarithromycin and minocycline alone and in combination against experimental Mycobacterium leprae infection in mice. Antimicrob Agents Chemother. 1991; 35:579-81. https://pubmed.ncbi.nlm.nih.gov/1828136 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245054/
35. Fernandes PB, Hardy DJ, McDaniel D et al. In vitro and in vivo activities of clarithromycin against Mycobacterium avium . Antimicrob Agents Chemother. 1989; 33: 1531-4. https://pubmed.ncbi.nlm.nih.gov/2530933 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172696/
36. Naik S, Ruck R. In vitro activities of several new macrolide antibiotics against Mycobacterium avium complex. Antimicrob Agents Chemother. 1989; 33:1614-6. https://pubmed.ncbi.nlm.nih.gov/2817858 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172713/
37. Waites KB, Cassell GH, Canupp KC et al. In vitro susceptibilities of mycoplasmas and ureaplasmas to new macrolides and aryl-fluoroquinolones. Antimicrob Agents Chemother. 1988; 32:1500-2. https://pubmed.ncbi.nlm.nih.gov/2973283 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175906/
38. Bowie WR, Shaw CE, Chan DG et al. In vitro activity of Ro 15-8074, Ro 19-5247, A-56268, and roxithromycin (RU 28965) against Neisseria gonorrhoeae and Chlamydia trachomatis . Antimicrob Agents Chemother. 1987; 31:470-2. https://pubmed.ncbi.nlm.nih.gov/2953304 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174756/
39. Segreti J, Kessler HA, Kapell KS et al. In vitro activity of A-56268 (TE-031) and four other antimicrobial agents against Chlamydia trachomatis . Antimicrob Agents Chemother. 1987; 31:100-1. https://pubmed.ncbi.nlm.nih.gov/2952061 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174660/
40. Hardy DJ, Hanson CW, Hensey DM et al. Susceptibility of Campylobacter pylori to macrolides and fluoroquinolones. J Antimicrob Chemother. 1988; 22: 631-6. https://pubmed.ncbi.nlm.nih.gov/3209524
41. Derouin F, Chastang C. Activity in vitro against Toxoplasma gondii of azithromycin and clarithromycin alone and with pyrimethamine. J Antimicrob Chemother. 1990; 25:708-11. https://pubmed.ncbi.nlm.nih.gov/2161824
42. Chamberland S, Kirst HA, Current WL. Comparative activity of macrolides against Toxoplasma gondii demonstrating utility of an in vitro microassay. Antimicrob Agents Chemother. 1991; 35:903-9. https://pubmed.ncbi.nlm.nih.gov/1854172 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245127/
43. Chang HR, Pecherè JC. In vitro effects of four macrolides (roxithromycin, spiramycin, azithromycin [CP-62,993], and A-56268) on Toxoplasma gondii . Antimicrob Agents Chemother. 1988; 32:524-9. https://pubmed.ncbi.nlm.nih.gov/2837140 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172214/
44. Leclercq R, Courvalin P. Intrinsic and unusual resistance to macrolide, lincosamide, and streptogrammin antibiotics in bacteria. Antimicrob Agents Chemother. 1991; 35:1273-6. https://pubmed.ncbi.nlm.nih.gov/1929281 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245157/
45. Leclercq R, Courvalin P. Bacterial resistance to macrolide, lincosamide, and streptogrammin antibiotics by target modification. Antimicrob Agents Chemother. 1991; 35:1267-72. https://pubmed.ncbi.nlm.nih.gov/1929280 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245156/
46. Chien SM, Pichotta P, Siepman N et al. Treatment of community acquired pneumonia: a randomized, controlled trial comparing clarithromycin and erythromycin. Proceedings of ICAAC Chicago 1991. Abstract No. 872.
47. Cassell GH, Drnec J, Waites KB et al. Efficacy of clarithromycin against Mycoplasma pneumoniae . J Antimicrob Chemother. 1991; 27(Suppl A):47-59. https://pubmed.ncbi.nlm.nih.gov/1827102
48. Fernandez-Martin J, Leport C, Morlat P et al. Pyrimethamine-clarithromycin combination for therapy of acute toxoplasma encephalitis in patients with AIDS. Antimicrob Agents Chemother. 1991; 35:2049-52. https://pubmed.ncbi.nlm.nih.gov/1836943 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245324/
49. Nellans HN, Petersen AC, Peeters TL. Gastrointestinal side effects: clarithromycin superior to azithromycin in reduced smooth muscle contraction and binding. Proceedings of ICAAC Chicago 1991. Abstract No. 518.
50. Ruff F, Chu SY, Sonders RC et al. Effect of multiple doses of clarithromycin on the pharmacokinetics of theophylline. Proceedings of ICAAC Atlanta 1990. Abstract 761.
51. Richens A, Chu SY, Sennello LT et al. Effect of multiple doses of clarithromycin on the pharmacokinetics of carbamazepine. Proceedings of ICAAC Atlanta 1990. Abstract 760.
52. Polis MA, Haneiwich S, Kovacs JA et al. Dose escalation study to determine the safety, maximally tolerated dose, and pharmacokinetics of clarithromycin with zidovudine in HIV-infected persons. Proceedings of ICAAC Chicago 1991. Abstract 238.
53. Chu SY, Wilson DS, Eason C et al. Single- and multi-dose pharmacokinetics of clarithromycin. Proceedings of ICAAC Atlanta 1990. Abstract 759.
54. Fraschini F, Scaglione F, Pintucci G et al. The diffusion of clarithromycin and roxithromycin into nasal mucosa, tonsil and lung in humans. J Antimicrob Chemother. 1991; 27(Suppl A):61-5. https://pubmed.ncbi.nlm.nih.gov/1827103
55. Kohno Y, Ohta K, Suwa T et al. Autobacteriographic studies of clarithromycin and erythromycin in mice. Antimicrob Agents Chemother. 1990; 34:562-7. https://pubmed.ncbi.nlm.nih.gov/2140497 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC171644/
56. Neu HC. The development of macrolides: clarithromycin in perspective. J Antimicrob Chemother. 1991; 27(Suppl A):1-9. https://pubmed.ncbi.nlm.nih.gov/1827094
57. Janousky S, Northcutt VJ, Craft JC. Comparative safety and efficacy of clarithromycin and reference suspensions in the treatment of children with mild to moderate skin or skin structure infections. Proceedings of ICAAC Chicago 1991. Abstract No. 870.
58. Olsson-Liljequist B, Hoffman BM. In-vitro activity of clarithromycin combined with its 14-hydroxy metabolite A-62671 against Haemophilus influenzae . J Antimicrob Chemother. 1991; 27(Suppl A):11-7. https://pubmed.ncbi.nlm.nih.gov/1827097
59. Dabernat H, Delmas C, Seguy M et al. The activity of clarithromycin and its 14-hydroxy metabolite against Haemophilus influenzae, determined by in-vitro and serum bactericidal tests. J Antimicrob Chemother. 1991; 27(Suppl A):19-30. https://pubmed.ncbi.nlm.nih.gov/1827099
60. Valleé E, Azoulay-Dupuis E, Swanson R et al. Individual and combined activities of clarithromycin and its 14-hydroxy metabolite in a murine model of Haemophilus influenzae infection. J Antimicrob Chemother. 1991; 27(Suppl A):31-41. https://pubmed.ncbi.nlm.nih.gov/1827100
61. Ridgway GL, Mumtaz G, Fenelon L. The in-vitro activity of clarithromycin and other macrolides against the type strain of Chlamydia pneumoniae (TWAR). J Antimicrob Chemother. 1991; 27(Suppl A):43-5. https://pubmed.ncbi.nlm.nih.gov/1827101
62. Janousky S, Northcutt VJ, Craft JC. Comparative safety and efficacy of clarithromycin and penicillin V suspensions in the treatment of children with streptococcal pharyngitis. Proceedings of ICAAC Chicago 1991. Abstract No. 871.
63. Still JG, Hubbard WC, Poole JM et al. Randomized comparison of clarithromycin and penicillin V suspensions in the treatment of children with streptococcal pharyngitis and/or tonsillitis. Proceedings of ICAAC Chicago 1991. Abstract No. 873.
64. Wood MJ. More macrolides: some may be improvement on erythromycin. BMJ. 1991; 303:594-5. https://pubmed.ncbi.nlm.nih.gov/1932896 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1671102/
65. Chu SY, Park Y, Wilson DS et al. Pharmacokinetics of clarithromycin after 250 mg BID dosing of a suspension formulation. Proceedings of ICAAC Chicago 1991. Abstract No. 516.
66. Moellering RC Jr. Principles of anti-infective therapy. In: Mandell GL, Douglas RG Jr, Bennett JE, eds. Principles and practice of infectious diseases. 3rd ed. New York: Churchill Livingstone Inc; 1991:206-18.
67. Fraschini F, Scaglione F, Pintucci JP et al. Clarithromycin and its 14-OH-metabolite. Pharmacokinetics and tissues distribution in humans. Proceedings of ICAAC Chicago 1991. Abstract No. 512.
68. Kohno Y, Yoshida H, Suwa T et al. Comparative pharmacokinetics of clarithromycin (TE-031), a new macrolide antibiotic, and erythromycin in rats. Antimicrob Agents Chemother. 1989; 33:751-6. https://pubmed.ncbi.nlm.nih.gov/2526615 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172527/
69. Chu SY, Cavanaugh J, Guay D. Pharmacokinetics of clarithromycin and 14-OH-clarithromycin following oral administration of clarithromycin 500 mg tablet. Proceedings of ICAAC Chicago 1991. Abstract No. 513.
70. Chu SY, Sunnello LT, Bunnell ST. Pharmacokinetics of clarithromycin in subjects with varying renal function. Proceedings of ICAAC Chicago 1991. Abstract No. 514.
71. Gan VN, Chu SY, Kusmiesz HT et al. Single & multi-dose pharmacokinetics in children of clarithromycin granules for suspension. Proceedings of ICAAC Chicago 1991. Abstract No. 517.
72. Zundörf H, Wishchmann L, Fassender M et al. Pharmacokinetics of clarithromycin and possible with H2 blocker and antacids. Proceedings of ICAAC Chicago 1991. Abstract No. 515.
73. Kohno Y, Yoshida H, Suwa T et al. Uptake of clarithromycin by rat lung cells. J Antimicrob Chemother. 1990; 26:503-13. https://pubmed.ncbi.nlm.nih.gov/2147673
74. Fernandes PB, Ramer N, Rode RA et al. Bioassay for A-56268 (TE-031) and identification of its major metabolite, 14-hydroxy-6-O-methyl erythromycin. Eur J Clin Microbiol Infect Dis. 1988; 7:73-6. https://pubmed.ncbi.nlm.nih.gov/2967754
75. Sefton AM, Maskell JP, Yong FJ et al. Comparative in vitro activity of A-56268. Eur J Clin Microbiol Infect Dis. 1988; 7:798-802. https://pubmed.ncbi.nlm.nih.gov/2975218
76. Renaudin H, Bebéar C. Comparative in vitro activity of azithromycin, clarithromycin, erythromycin and lomefloxacin against Mycoplasma pneumoniae, Mycoplasma hominis and Ureaplasma urealyticum . Eur J Clin Microbiol Infect Dis. 1990; 9:838-41. https://pubmed.ncbi.nlm.nih.gov/1964899
77. Rastogi N, Labrousse V. Extracellular and intracellular activities of clarithromycin used alone and in association with ethambutol and rifampin against Mycobacterium avium complex. Antimicrob Agents Chemother. 1991; 35:462-70. https://pubmed.ncbi.nlm.nih.gov/1828135 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245033/
78. Powell M, Chen HY, Weinhardt B et al. In-vitro cidal activity of clarithromycin and its 14-hydroxy metabolite (A-62671) against Haemophilus influenzae . J Antimicrob Chemother. 1991; 27:694-6. https://pubmed.ncbi.nlm.nih.gov/1832146
79. Barry AL, Fernandes PB, Jorgensen JH et al. Variability of clarithromycin and erythromycin susceptibility tests with Haemophilus influenzae in four different broth media and correlation with the standard disk diffusion test. J Clin Microbiol. 1988; 26:2415-20. https://pubmed.ncbi.nlm.nih.gov/2976773 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC266903/
80. Logan MN, Ashby JP, Andrews JM et al. The in-vitro and disc susceptibility testing of clarithromycin and its 14-hydroxy metabolite. J Antimicrob Chemother. 1991; 27:161-70. https://pubmed.ncbi.nlm.nih.gov/1829073
81. Jorgensen JH, Maher LA, Howell AW. Activity of clarithromycin and its principal human metabolite against Haemophilus influenzae . Antimicrob Agents Chemother. 1991; 35:1524-6. https://pubmed.ncbi.nlm.nih.gov/1834012 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC245208/
82. Barry AL, Thornsberry C, Jones RN. In vitro activity of a new macrolide, A-56268, compared with that of roxithromycin, erythromycin, and clindamycin. Antimicrob Agents Chemother. 1987; 31:343-5. https://pubmed.ncbi.nlm.nih.gov/2952064 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174723/
83. Fernandes PB, Hardy DJ. Comparative in vitro potencies of nine new macrolides. Drugs Exp Clin Res. 1988; 14: 445-51.
84. Eliopoulos GM, Reiszner E, Ferraro MJ et al. Comparative in-vitro activity of A-56268 (TE-031), a new macrolide antibiotic. J Antimicrob Chemother. 1988; 20:671-5.
85. Hodinka RL, Jack-Wait K, Gilligan PH. Comparative in vitro activity of A-56268 (TE-031), a new macrolide antibiotic. Eur J Clin Microbiol. 1987; 6:103-8. https://pubmed.ncbi.nlm.nih.gov/2952499
86. Floyd-Reising S, Hindler JA, Young LS. In vitro activity of A-56268 (TE-031), a new macrolide antibiotic, compared with that of erythromycin and other antimicrobial agents. Antimicrob Agents Chemother. 1987; 31:640-2. https://pubmed.ncbi.nlm.nih.gov/2955742 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC174797/
87. Berlin OG, Young LS, Floyd-Reising SA et al. Comparative in vitro activity of the new macrolide A-56268 against mycobacteria. Eur J Clin Microbiol. 1987; 6:486-7. https://pubmed.ncbi.nlm.nih.gov/2959472
88. Brown BA, Wallace RJ, Onyi GO et al. Activities of four macrolides, including clarithromycin, against Mycobacterium fortuitum, Mycobacterium chelonae, and M. chelonae-like organisms. Antimicrob Agents Chemother. 1992; 36(1):180-4. https://pubmed.ncbi.nlm.nih.gov/1317144 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC189249/
89. Jones RN, Erwin ME, Barrett MS. In vitro activity of clarithromycin (TE-031, A-67268) and 14OH-clarithromycin alone and in combination against Legionella species. Eur J Clin Microbiol Infect Dis. 1990; 9:846-8. https://pubmed.ncbi.nlm.nih.gov/2150817
90. Kohno S, Koga H, Yamaguchi K et al. A new macrolide, TE-031 (A-56268), in treatment of experimental Legionnaires’ disease. J Antimicrob Chemother. 1989; 24:397-405. https://pubmed.ncbi.nlm.nih.gov/2530201
91. Chirgwin K, Roblin PM, Hammerschlag MR. In vitro susceptibilities of Chlamydia pneumoniae (Chlamydia sp. strain TWAR). Antimicrob Agents Chemother. 1989; 33:1634-5. https://pubmed.ncbi.nlm.nih.gov/2817862 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC172720/
92. Benson C, Segreti J, Kessler H et al. Comparative in vitro activity of A-56268 (TE-031) against gram-positive and gram-negative bacteria and Chlamydia trachomatis . Eur J Clin Microbiol. 1987; 6:173-8. https://pubmed.ncbi.nlm.nih.gov/2954818
93. Felmingham D, Robbins MJ, Sanghrajka M et al. The in vitro activity of some 14-, 15- and 16-membered macrolides against Staphylococcus spp., Legionella spp., Mycoplasma spp. and Ureaplasma urealyticum . Drugs Exp Clin Res. 1991; 17:91-9. https://pubmed.ncbi.nlm.nih.gov/1650694
94. Morimoto S, Nagate T, Sugita K et al. Chemical modification of erythromycins. III. In vitro and in vivo antibacterial activities of new semisynthetic 6-O-methylerythromycins A, TE-031 (clarithromycin) and TE-032. J Antibiot (Tokyo). 1990; 43(3):295-305. https://pubmed.ncbi.nlm.nih.gov/2139023
95. Rolston K, Gooch G, Ho DH. In vitro activity of clarithromycin against Gram-positive bacteria. J Antimicrob Chemother. 1989; 23:455-7. https://pubmed.ncbi.nlm.nih.gov/2525120
96. Neu HC. New macrolide antibiotics: azithromycin and clarithromycin. Ann Intern Med. 1992; 116:517-9. https://pubmed.ncbi.nlm.nih.gov/1310839
97. Hardy DJ, Guay DR, Jones RN. Clarithromycin, a unique macrolide: a pharmacokinetic, microbiological, and clinical overview. Diagn Microbiol Infect Dis. 1992; 15:39-53. https://pubmed.ncbi.nlm.nih.gov/1530914
98. Davey PG. The pharmacokinetics of clarithromycin and its 14-OH metabolite. J Hosp Infect. 1991; 19(Suppl A): 29-37. https://pubmed.ncbi.nlm.nih.gov/1684980
99. Wood MJ. The tolerance and toxicity of clarithromycin. J Hosp Infect. 1991; 19(Suppl A):39-46. https://pubmed.ncbi.nlm.nih.gov/1684982
100. Ball P. The future role and importance of macrolides. J Hosp Infect. 1991; 19(Suppl A):47-59. https://pubmed.ncbi.nlm.nih.gov/1684983
101. Anderson G. Clarithromycin in the treatment of community-acquired lower respiratory tract infections. J Hosp Infect. 1991; 19(Suppl A):21-7. https://pubmed.ncbi.nlm.nih.gov/1684979
102. Chu SY, Park Y, Locke C et al. Drug-food interaction potential of clarithromycin, a new macrolide antimicrobial. J Clin Pharmacol. 1992; 32:32-6. https://pubmed.ncbi.nlm.nih.gov/1531484
103. Adachi T, Morimoto S, Kondoh H et al. 14-Hydroxy -6-O-methylerythromycins A, active metabolites of 6-O-methylerythromycin A in human. J Antibiot (Tokyo). 1988; 41:966-75. https://pubmed.ncbi.nlm.nih.gov/2971033
104. Preac-Mursic V, Wilske B, Schierz G et al. Comparative antimicrobial activity of the new macrolides against Borrelia burgdorferi . Eur J Clin Microbiol Infect Dis. 1989; 8:651-3. https://pubmed.ncbi.nlm.nih.gov/2550233
105. Kosek M, Alcantara C, Lima AAM et al. Cryptosporidiosis: an update. Lanc Infect Dis. 2001; 1:262-9.
106. Chen XM, Keithly JS, Paya CV et al. Cryptosporidiosis. N Engl J Med. 2002; 346:1723-31. https://pubmed.ncbi.nlm.nih.gov/12037153
107. Dajani A, Taubert K, Ferrieri P et al and the American Heart Association Committee on Rheumatic Fever et al. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: a statement for health professionals. Pediatrics. 1995; 96:758-64. https://pubmed.ncbi.nlm.nih.gov/7567345
108. National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing; twelfth informational supplement. NCCLS document M100-S12. NCCLS: Wayne, PA; 2002 Jan.
109. Bisno AL, Gerber MA, Gwaltney JM et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin Infect Dis. 2002; 35:113-25. https://pubmed.ncbi.nlm.nih.gov/12087516
110. Cooper RJ, Hoffman JR, Bartlett JG et al. Principles of appropriate antibiotic use for acute pharyngitis in adults: background. Ann Intern Med. 2001; 134:509-17. https://pubmed.ncbi.nlm.nih.gov/11255530
111. Holmberg SD, Moorman AC, Von Bargen JC et al. Possible effectiveness of clarithromycin and rifabutin for cryptosporidiosis chemoprophylaxis in HIV disease. HIV outpatient study (HOPS) investigators. JAMA. 1998; 279:384-6. https://pubmed.ncbi.nlm.nih.gov/9459473
112. Agouron Pharmaceuticals Inc. Rescriptor (delavirdine mesylate) tablets prescribing information. La Jolla, CA; 2001 Jun 8.
113. Heffelfinger JD, Dowell SF, Jorgensen JH et al. Management of community-acquired pneumonia in the era of pneumococcal resistance. A report from the drug-resistant Streptococcus pneumoniae therapeutic working group. Arch Intern Med. 2000; 160:1399-1408. https://pubmed.ncbi.nlm.nih.gov/10826451
114. Centers for Disease Control and Prevention. Update: investigation of bioterrorism-related anthrax and interim guidelines for exposure management and antimicrobial therapy, October 2001. MMWR Morb Mortal Wkly Rep. 2001; 50:909-19. https://pubmed.ncbi.nlm.nih.gov/11699843
115. Dworkin MS, Hanson DL, Kaplan JE et al. Risk for preventable opportunistic infections in persons with AIDS after antiretroviral therapy increases CD4+ T lymphocyte counts above prophylaxis thresholds. J Infect Dis. 2000; 182:611-5. https://pubmed.ncbi.nlm.nih.gov/10915098
116. Currier JS, Williams PL, Koletar SL et al. Discontinuation of Mycobacterium avium complex prophylaxis in patients with antiretroviral therapy-induced increases in CD4+ cell count. A randomized, double-blind, placebo-controlled trial. Ann Intern Med. 2000; 133:493-503. https://pubmed.ncbi.nlm.nih.gov/11015162
117. El-Sadr WM, Burman WJ, Grant LB et al. Discontinuation of prophylaxis against Mycobacterium avium complex disease in HIV-infected patients who have a response to antiretroviral therapy. N Engl J Med. 2000; 342:1085-92. https://pubmed.ncbi.nlm.nih.gov/10766581
118. Rossi M, Flepp M, Telenti A et al. Disseminated M. avium complex infection in the Swiss HIV cohort study: declining incidence, improved prognosis and discontinuation of maintenance therapy. Swiss Med Wkly. 2001; 131:471-7. https://pubmed.ncbi.nlm.nih.gov/11641970
119. Soriano V, Dona C, Rodriguez-Rosado R et al. Discontinuation of secondary prophylaxis for opportunistic infections in HIV-infected patients receiving highly active antiretroviral therapy. AIDS. 2000; 14:383-6. https://pubmed.ncbi.nlm.nih.gov/10770540
121. Reviewers’ comments (personal observations).
122. Alder J, Mitten M, Hernandez L et al. Synergy between clarithromycin and sulfamethoxazole in the treatment of Pneumocystis carinii in rats. First International Conference on the Macrolides, Azalides and Streptogramins. Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 179.
123. Hughes WT, Killmar JT. Synergistic anti-Pneumocystis carinii effects of clarithromycin and sulfamethoxazole. First International Conference on the Macrolides, Azalides and Streptogramins. Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 180.
124. Cama VA, Marshall MM, Sterling CR. Synergy between clarithromycin and sulfamethoxazole in the treatment of Pneumocystis carinii in rats. First International Conference on the Macrolides, Azalides and Streptogramins. Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 181.
125. Rehg JE. Anticryptosporidial activity of macrolides in immunosuppressed rats. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 182.
126. Abbott Laboratories, Abbott Park, IL: Personal communication.
127. Suwa T, Yoshida H, Kohno Y et al. Metabolic fate of TE-031 (A-56268) (III). Absorption, distribution and excretion of 14C-TE-031 in rats, mice and dogs. Chemotherapy (Tokyo). 1988; 36(Suppl 3):223-6.
128. Pichotta P, Janousky S, Prokocimer P. Safety of clarithromycin in elderly patients. 17th International Congress of Chemotherapy, Berlin, Germany, June 1991. Abstract No. 1252.
129. Neu H, Craft JC. Clarithromycin vs cephalosporin therapy for the treatment of H. influenzae bronchitis. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 237.
130. Dubois J, St. Pierre C, Prokocimer P. Treatment of community-acquired pneumonia: a comparison of clarithromycin and erythromycin. Proceedings of ICAAC Atlanta 1990. Abstract.
131. Futterman M, Drnec J. Safety and efficacy of clarithromycin compared with erythromycin in the treatment of community-acquired pneumonia. Proceedings of ICAAC Atlanta 1990. Abstract.
132. Prokocimer P, Siepman N. Treatment of community-acquired pneumonia: a comparison of clarithromycin and erythromycin. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 244.
133. Nicotra MB, Northcutt VJ. Results of comparative trials of clarithromycin and erythromycin in the treatment of community-acquired pneumonia. 17th International Congress of Chemotherapy, Berlin, Germany, June 1991. Abstract.
134. Block S, Hedrick J, Hammerschlag MR et al. Mycoplasma pneumoniae and Chlamydia pneumoniae in pediatric community-acquired pneumonia: comparative efficacy and safety of clarithromycin vs.erythromycin ethylsuccinate. Pediatr Infect Dis J. 1995; 14:471-7. https://pubmed.ncbi.nlm.nih.gov/7667050
135. Prokocimer P. An evaluation of clarithromycin and cefixime for lower respiratory tract infections. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 243.
136. Gupta S, Siepman N. Comparative safety and efficacy of clarithromycin versus reference agents in the treatment of mild to moderate bacterial skin or skin structure infections. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 254.
137. Millikan L. Safety and efficacy of clarithromycin compared to cefadroxil in the treatment of children with mild to moderate bacterial skin or skin structure infections. Proceedings of ICAAC Atlanta 1990. Abstract.
138. Carey WD, Yanofsky H. Safety and efficacy of clarithromycin compared to erythromycin in the treatment of bacterial skin or skin structure infections. 7th Mediterranean Congress of Chemotherapy, Barcelona, Spain, May 1990. Abstract.
139. Mikell OL. Treatment of bacterial skin or skin structure infections: a comparison of clarithromycin and cefadroxil. 7th Mediterranean Congress of Chemotherapy, Barcelona, Spain, May 1990. Abstract.
140. Northcutt VJ, Craft JC, Pichotta P. Safety and efficacy of clarithromycin compared to erythromycin in the treatment of bacterial skin or skin structure infections. Proceedings of ICAAC Atlanta 1990. Abstract.
141. Chan GP, Garcia-Ignacio BY, Chavez VE et al. Clinical trial of clarithromycin for lepromatous leprosy. Antimicrob Agents Chemother. 1994; 38:515-7. https://pubmed.ncbi.nlm.nih.gov/8203847 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC284490/
142. Ji B, Jamet P, Perani EG et al. Clarithromycin, a promising component of new combined regimens for the treatment of multibacillary leprosy. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 266.
143. Stein GE, Christensen S, Mummaw N. Comparative study of clarithromycin and penicillin V in the treatment of streptococcal pharyngitis. Eur J Clin Microbiol Infect Dis. 1991; 10:949-53. https://pubmed.ncbi.nlm.nih.gov/1838978
144. St. Pierre C, Dubois J, Prokocimer P et al. An evaluation of clarithromycin and amoxicillin/clavulanate for the treatment of acute maxillary sinusitis. First International Conference on the Macrolides, Azalides and Streptogramins, Santa Fe, New Mexico, January 22-25, 1992. Abstract No. 229.
145. Tinel M, Descatoire V, Larrey D et al. Effects of clarithromycin on cytochrome P-450. Comparison with other macrolides. J Pharmacol Exp Ther. 1989; 250:746-51. https://pubmed.ncbi.nlm.nih.gov/2527301
147. Johnson M, Mattson L, Bopp B et al. The in vitro protein binding of 14-hydroxy clarithromycin in human plasma. Proceedings of ICAAC Chicago 1991. Abstract.
148. Niki Y, Nakajima M, Tsukiyama K et al. [Effect of TE-031 (A-56268), a new oral macrolide antibiotic, on serum theophylline concentration.] (Japanese; with English abstract.) Chemotherapy (Tokyo). 1988; 36(Suppl 3):515-20.
150. Marion Merrell Dow. Seldane (terfenadine) tablets prescribing information. Kansas City, MO; 1993 Jan.
151. Marion Merrell Dow, Kansas City, MO: Personal communication.
152. Marion Merrell Dow. Dear health care professional letter regarding appropriate use of Seldane. Kansas City, MO: 1992 Jul 7.
153. Mathews DR, McNutt B, Okerholm R et al. Torsades de pointes occurring in association with terfenadine use. JAMA. 1991; 266:2375-6. https://pubmed.ncbi.nlm.nih.gov/1920744
154. Honig PK, Zamani K, Woosley RL et al. Erythromycin changes terfenadine pharmacokinetics & electrocardiographic pharmacodynamics. Clin Pharmacol Ther. 1992; 51:156.
155. Honig PK, Woosley RL, Zamani K et al. Changes in the pharmacokinetics and electrocardiographic pharmacodynamics of terfenadine with concomitant administration of erythromycin. Clin Pharmacol Ther. 1992; 52:231-8. https://pubmed.ncbi.nlm.nih.gov/1526078
156. Peck CC, Temple R, Collins JM. Understanding consequences of concurrent therapies. JAMA. 1993; 269:1550-2. https://pubmed.ncbi.nlm.nih.gov/8445821
157. Antihistamines, nonsedating/macrolide antibiotics. In: Tatro DS, Olin BR, Hebel SK, eds. Drug interaction facts. St. Louis: JB Lippincott Co; 1996(July):110d.
158. Anon. Safety of terfenadine and astemizole. Med Lett Drugs Ther. 1992; 34:9-10. https://pubmed.ncbi.nlm.nih.gov/1732711
159. Monahan BP, Ferguson CL, Killeary ES et al. Torsades de pointes occurring in association with terfenadine use. JAMA. 1990; 264:2788-90. https://pubmed.ncbi.nlm.nih.gov/1977935
160. Cruzan S (US Food and Drug Administration). HHS News. Press release No. P92-22. 1992 Jul 7.
161. Cortese LM, Bjornson DC. Comment: the new macrolide antibiotics and terfenadine. Ann Pharmacother. 1992; 26:1019. https://pubmed.ncbi.nlm.nih.gov/1504390
162. Nightingale SL. Warnings issued on nonsedating antihistamines terfenadine and astemizole. JAMA. 1992; 268:705. https://pubmed.ncbi.nlm.nih.gov/1322467
163. Anon. New boxed warnings added for Seldane, Hismanal. FDA Med Bull. 1992; 22(Sep):2-3.
164. Marion Merrell Dow. Seldane-D (terfenadine and pseudoephedrine hydrochloride) extended-release tablets prescribing information. (dated 1993 May). In: Physicians’ desk reference. 50th ed. Montvale, NJ: Medical Economics Company Inc; 1996:1538-40.
166. Woosley RL, Chen Y, Freiman JP et al. Mechanism of the cardiotoxic actions of terfenadine. JAMA. 1993; 269:1532-6. https://pubmed.ncbi.nlm.nih.gov/8445816
167. Anon. Labeling change to reflect drug interaction between terfenadine and ketoconazole. FDA Med Bull. 1991; 21(Jul):4-5.
168. Rolf CN. Dear doctor letter regarding important drug warning of Seldane. Cincinnati, OH: Marion Merrell Dow; 1990 Aug 6.
169. Cortese LM, Bjornson DC. Potential interaction between terfenadine and macrolide antibiotics. Clin Pharm. 1992; 11:675. https://pubmed.ncbi.nlm.nih.gov/1511540
170. Price TA, Tuazon CU. Clarithromycin-induced thrombocytopenia. Clin Infect Dis. 1992; 15:563-4. https://pubmed.ncbi.nlm.nih.gov/1387810
171. US Public Health Service Task Force on Prophylaxis and Therapy for Mycobacterium avium complex. Recommendations on prophylaxis and therapy for disseminated Mycobacterium avium complex for adults and adolescents infected with human immunodeficiency virus. MMWR Morb Mortal Wkly Rep. 1993; 42(No. RR-9):1-20. https://pubmed.ncbi.nlm.nih.gov/8418395 https://www.cdc.gov/mmwr/PDF/rr/rr4209.pdf
172. de Lalla F, Maserati R, Scarpellini P et al. Clarithromycin-ciprofloxacin-amikacin for therapy of Mycobacterium avium-Mycobacterium intracellulare bacteremia in patients with AIDS. Antimicrob Agents Chemother. 1992; 36:1567-9. https://pubmed.ncbi.nlm.nih.gov/1387303 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC191622/
173. Dautzenberg B, Saint Marc T, Meyohas MC et al. Clarithromycin and other antimicrobial agents in the treatment of disseminated Mycobacterium avium infections in patients with acquired immunodeficiency syndrome. Arch Intern Med. 1993; 153:368-72. https://pubmed.ncbi.nlm.nih.gov/8427539
174. Young LS, Wiviott L, Wu M et al. Azithromycin for treatment of Mycobacterium avium-intracellulare complex infection in patients with AIDS. Lancet. 1991; 338:1107-8. https://pubmed.ncbi.nlm.nih.gov/1682544
175. Young LS. Mycobacterial diseases and the compromised host. Clin Infect Dis. 1993; 17(Suppl 2):S436-41. https://pubmed.ncbi.nlm.nih.gov/8274609
176. Wallace RJ Jr, Brown BA, Griffith DE et al. Initial clarithromycin monotherapy for Mycobacterium avium-intracellulare complex lung disease. Am J Respir Crit Care Med. 1994; 149:1335-41. https://pubmed.ncbi.nlm.nih.gov/8173775
177. Benson CA, Ellner JJ. Mycobacterium avium complex infection and AIDS: advances in theory and practice. Clin Infect Dis. 1993; 17:7-20. https://pubmed.ncbi.nlm.nih.gov/8353249
178. Benson CA. Treatment of disseminated disease due to the Mycobacterium avium complex in patients with AIDS. Clin Infect Dis. 1994; 18(Suppl 3):S237-42.
179. Mor N, Heifets L. MICs and MBCs of clarithromycin against Mycobacterium avium within human macrophages. Antimicrob Agents Chemother. 1993; 37(1):111-4. https://pubmed.ncbi.nlm.nih.gov/8431006 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC187614/
180. De Wit S, D’Abraccio M, De Mol P et al. Acquired resistance to clarithromycin as combined therapy in Mycobacterium avium intracellulare infection. Lancet. 1993; 341:53-4. https://pubmed.ncbi.nlm.nih.gov/8093299
181. Ruf B, Schurmann D, Mauch H. Acquired resistance of MAI to clarithromycin. Am Rev Respir Dis. 1992; 145:1241-2. https://pubmed.ncbi.nlm.nih.gov/1533999
182. Heifets L, Mor N, Vanderkolk J. Mycobacterium avium strains resistant to clarithromycin and azithromycin. Antimicrob Agents Chemother. 1993; 37:2364-70. https://pubmed.ncbi.nlm.nih.gov/8031351 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC192393/
183. Wolinsky E. Mycobacterium avium strains resistant to clarithromycin and azithromycin. Antimicrob Agents Chemother. 1994; 38:635. https://pubmed.ncbi.nlm.nih.gov/8031406 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC284513/
184. Heifets L, Mor N, Vanderkolk J. Mycobacterium avium strains resistant to clarithromycin and azithromycin. Antimicrob Agents Chemother. 1994; 38:635. https://pubmed.ncbi.nlm.nih.gov/8031406 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC284513/
185. Barradell LB, Plosker GL, McTavish D. Clarithromycin: a review of its pharmacological properties and therapeutic use in Mycobacterium avium-intracellulare complex infection in patients with acquired immunodeficiency syndrome. Drugs. 1993; 46(2):289-312. https://pubmed.ncbi.nlm.nih.gov/7691518
186. Guay DR, Craft JC. Overview of the pharmacology of clarithromycin suspension in children and a comparison with that in adults. Pediatr Infect Dis J. 1993; 12(12 Suppl 3):S106-11.
187. Husson RN, Ross LA, Sandelli S et al. Orally administered clarithromycin for the treatment of systemic Mycobacterium avium complex infection in children with acquired immunodeficiency syndrome. J Pediatr. 1994; 124:807-14. https://pubmed.ncbi.nlm.nih.gov/8176574
188. Wallace RJ Jr, Tanner D, Brennan PJ et al. Clinical trial of clarithromycin for cutaneous (disseminated) infection due to Mycobacterium chelonae . Ann Intern Med. 1993; 119:482-6. https://pubmed.ncbi.nlm.nih.gov/8357113
189. Bonnet E, Debat-Zouguereh D, Petit N et al. Clarithromycin: a potent agent against infections due to Mycobacterium marinum . Clin Infect Dis. 1994; 18:664-6. https://pubmed.ncbi.nlm.nih.gov/8038339
190. Sundberg L, Cederberg A. Penetration of clarithromycin and its 14-hydroxy metabolite into middle ear infusion in children with secretory otitis media. J Antimicrob Chemother. 1994; 33:299-307. https://pubmed.ncbi.nlm.nih.gov/8182011
191. Janssen Pharmaceutica. Hismanal (astemizole) tablets prescribing information. Titusville, NJ; 1998 Feb.
192. Peck CC, Temple R, Collins JM. Understanding consequences of concurrent therapies. JAMA. 1993; 269:1550-2. https://pubmed.ncbi.nlm.nih.gov/8445821
193. Hachem CY, Clarridge JE, Reddy R et al. Antimicrobial susceptibility testing of Helicobacter pylori: comparison of E-test, broth microdilution, and disk dffusion for ampicillin, clarithromycin, and metronidazole. Diagnost Microbiol Infect Dis. 1996; 24:37-41.
194. Astra Merck. Prilosec (omeprazole) delayed-release capsules prescribing information. Wayne, PA; 1996 Apr.
195. Gustavson LE, Kaiser JF, Edmonds AL et al. Effect of omeprazole on concentrations of clarithromycin in plasma and gastric tissue at steady state. Antimicrob Agents Chemother. 1995; 39:2078-83. https://pubmed.ncbi.nlm.nih.gov/8540719 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC162884/
196. Markham A, McTavish D. Clarithromycin and omeprazole: as Helicobacter pylori eradication therapy in patients with H. pylori-associated gastric disorders. Drugs. 1996; 51:161-78. https://pubmed.ncbi.nlm.nih.gov/8741237
197. Abbott Laboratories, North Chicago, IL: personal communication.
198. Liviu L, Yair L, Yehuda S. Pancreatitis induced by clarithromycin. Ann Intern Med. 1996; 125:701. https://pubmed.ncbi.nlm.nih.gov/8849171
199. Sung JJY, Chung SCS, Ling TKW et al. Dual therapy versus triple therapy for Helicobacter pylori-associated duodenal ulcers. Dig Dis Sci. 1996; 41:453-7. https://pubmed.ncbi.nlm.nih.gov/8617114
201. Horsburgh CR Jr. Advances in the prevention and treatment of Mycobacterium avium disease. N Engl J Med. 1996; 335:428-30. https://pubmed.ncbi.nlm.nih.gov/8663875
202. Havlir DV, Dube MP, Sattler FR et al. Prophylaxis against disseminated Mycobacterium avium complex with weekly azithromycin, daily rifabutin, or both. N Engl J Med. 1996; 335:392-8. https://pubmed.ncbi.nlm.nih.gov/8676932
203. Pierce M, Crampton S, Henry D et al. A randomized trial of clarithromycin as prophylaxis against disseminated Mycobacterium avium complex infection in patients with advanced acquired immunodeficiency syndrome. N Engl J Med. 1996; 335:384-91. https://pubmed.ncbi.nlm.nih.gov/8663871
204. US Public Health Service (USPHS) and Infectious Diseases Society of America (IDSA) Prevention of Opportunistic Infections Working Group. 2001 USPHS/IDSA guidelines for the prevention of opportunistic infections in persons with human immunodeficiency virus. From the US Department of Health and Human Services HIV/AIDS Information Services (HIV.gov) website. http://HIV.gov.nih.gov
206. Wallace RJ Jr, Griffith DE, Brown BA et al. Clarithromycin treatment for Mycobacterium avium-intracellulare complex lung disease. Am J Respir Crit Care Med. 1996; 153:1990-1. https://pubmed.ncbi.nlm.nih.gov/8665069
208. Moore RD, Chaisson RE. Survival analysis of two controlled trials of rifabutin prophylaxis against Mycobacterium avium complex in AIDS. AIDS. 1995; 9:1337-42. https://pubmed.ncbi.nlm.nih.gov/8605053
209. Centers for Disease Control and Prevention. Infection with Mycobacterium abscessus associated with intramuscular injection of adrenal cortex extract—Colorado and Wyoming, 1995–1996. MMWR Morb Mortal Wkly Rep. 1996; 45:713-5. https://pubmed.ncbi.nlm.nih.gov/8769652
210. Archange YR, Carrey Z, Zanlungo PG. Clarithromycin prophylaxis against disseminated Mycobacterium avium complex in patients with AIDS. J Int Assoc Physicians AIDS Care. 1995; 1:20-2. https://pubmed.ncbi.nlm.nih.gov/11362747
211. Chaisson RE, Benson CA, Dube MP et al. Clarithromycin therapy for bacteremic Mycobacterium avium complex disease. Ann Intern Med. 1994; 121:905-11. https://pubmed.ncbi.nlm.nih.gov/7978715
212. Flegg PJ, Laing RB, Lee C et al. Disseminated disease due to Mycobacterium avium complex in AIDS. QJM. 1995; 88:617-26. https://pubmed.ncbi.nlm.nih.gov/7583075
213. Chin DP, Reingold AL, Stone EN et al. The impact of Mycobacterium avium complex bacteremia and its treatment on survival of AIDS patients—a prospective study. J Infect Dis. 1994; 170:578-84. https://pubmed.ncbi.nlm.nih.gov/7915749
214. Chin DP, Hopewell PC. How to treat bacteraemic Mycobacterium avium complex disease. Lancet. 1995; 346:920-1. https://pubmed.ncbi.nlm.nih.gov/7564723
215. Shafran SD, Singer J, Zarowny DP et al. A comparison of two regimens for the treatment of Mycobacterium avium complex bacteremia in AIDS: rifabutin, ethambutol, and clarithromycin versus rifampin, ethambutol, clofazimine, and ciprofloxacin. N Engl J Med. 1996; 335:377-83. https://pubmed.ncbi.nlm.nih.gov/8676931
216. Horsburgh CR Jr, Havlik JA, Ellis DA et al. Survival of patients with acquired immune dieficiency syndrome and disseminated Mycobacterium avium complex infection with and without antimycobacterial chemotherapy. Am Rev Respir Dis. 1991; 144:557-9. https://pubmed.ncbi.nlm.nih.gov/1892294
217. May T, Brel F, Beuscart C et al. Comparison of combination therapy regimens for treatment of human immunodeficiency virus-infected patients with disseminated bacteremia due to Mycobacterium avium . Clin Infect Dis. 1997; 25:621-9. https://pubmed.ncbi.nlm.nih.gov/9314450
218. Chaisson RE, Keiser P, Pierce M et al. Controlled trial of clarithromycin/ethambutol with or without clofazimine for Mycobacterium avium complex bacteremia in AIDS. In: Abstracts of the 3rd Conference on Retroviruses and Opportunistic Infections, Washington, DC, 1996 Jan 28-Feb 1. Washington, DC: American Society for Microbiology, 1996:164. Abstract.
219. Burman W, Reves R, Rietmeijer C et al. Relapse of disseminated mycobacteriun avium complex disease and emergence of resistance to clarithromycin despite treatment with a multidrug regimen. In: Abstracts of the 3rd Conference on Retroviruses and Opportunistic Infections, Washington, DC, 1996 Jan 28-Feb 1. Washington, DC: American Society for Microbiology, 1996:85. Abstract.
220. Dube M, Sattler F, Torriani F et al. Prevention of relapse of MAC bacteremia in AIDS: a randomized study of clarithromycin plus clofazimine, with or without ethambutol. In: Abstracts of the 3rd Conference on Retroviruses and Opportunistic Infections, Washington, DC, 1996 Jan 28-Feb 1. Washington, DC: American Society for Microbiology, 1996:91. Abstract.
221. Currier J. Progress report: prophylaxis and therapy for MAC. AIDS Clin Care. 1996; 8:45-8. https://pubmed.ncbi.nlm.nih.gov/11363599
222. Benson CA. MAC: pathogenesis and treatment. In: Abstracts of the 3rd Conference on Retroviruses and Opportunistic Infections, Washington, DC, 1996 Jan 28-Feb 1. Washington, DC: American Society for Microbiology, 1996:166. Abstract.
223. Anon. High-dose clarithromycin should be avoided. AIDS Alert. 1996; 11:102. https://pubmed.ncbi.nlm.nih.gov/11363723
224. Cohn DL, Fisher E, Franchino B et al. Comparison of two doses of clarithromycin in a randomized trial of four 3-drug regimens for treatment of disseminated Mycobacterium avium complex disease in AIDS: excess mortality associated with high-dose clarithromycin. Presented at the 11th International Conference on AIDS, Vancouver, BC, July 7-12, 1996. Abstract.
225. Horowitz RS, Dart RC, Gomez HF. Clinical ergotism with lingual ischemia induced by clarithromycin-ergotamine interaction. Arch Intern Med. 1996; 156:456-8. https://pubmed.ncbi.nlm.nih.gov/8607732
226. Nightingale SD, Koster FT, Mertz GJ et al. Clarithromycin-induced mania in two patients with AIDS. Clin Infect Dis. 1995; 20:1563-4. https://pubmed.ncbi.nlm.nih.gov/7548513
227. Wallace RJ Jr, Brown BA, Griffith DE et al. Reduced serum levels of clarithromycin in patients treated with multidrug regimens including rifampin or rifabutin for Mycobacterium avium-M. intracellulare infection. J Infect Dis. 1995; 171:747-50. https://pubmed.ncbi.nlm.nih.gov/7876634
229. Goldberger M, Masur H. Clarithromycin therapy for Mycobacterium avium complex disease in patients with AIDS: potential and problems. Ann Intern Med. 1994; 121:974-5. https://pubmed.ncbi.nlm.nih.gov/7978725
230. Soll AH. Medical treatment of peptic ulcer disease. JAMA. 1996; 275:622-9. https://pubmed.ncbi.nlm.nih.gov/8594244
231. Soll AH. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1136-7.
232. Olsen CA. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1135-6.
233. Ateshkadi A, Lam NP, Johnson CA. Helicobacter pylori and peptic ulcer disease. Clin Pharm. 1993; 12:34-48. https://pubmed.ncbi.nlm.nih.gov/8428432
234. Blaser MJ. Helicobacter pylori: its role in disease. Clin Infect Dis. 1992; 15:386-91. https://pubmed.ncbi.nlm.nih.gov/1520782
235. Marshall BJ. Treatment strategies for Helicobacter pylori infection. Gastroenterol Clin North Am. 1993; 22:183-98. https://pubmed.ncbi.nlm.nih.gov/8449566
236. Israel DM, Hassall E. Treatment and long-term follow-up of Helicobacter pylori-associated duodenal ulcer disease in children. J Pediatr. 1993; 123:53-8. https://pubmed.ncbi.nlm.nih.gov/8320625
237. Murray DM, DuPont HL, Cooperstock M et al. Evaluation of new anti-infective drugs for the treatment of gastritis and peptic ulcer disease associated with infection by Helicobacter pylori . Clin Infect Dis. 1992; 15(Suppl 1):S268-73.
238. Chiba N, Rao BV, Rademaker JW et al. Meta-analysis of the efficacy of antibiotic therapy in eradicating Helicobacter pylori . Am J Gastroenterol. 1992; 87:1716-27. https://pubmed.ncbi.nlm.nih.gov/1449132
239. Glassman MS. Helicobacter pylori infection in children. A clinical overview. Clin Pediatr (Phila). 1992; 31:481-7. https://pubmed.ncbi.nlm.nih.gov/1643767
240. Peterson WL. Helicobacter pylori and peptic ulcer disease. N Engl J Med. 1991; 324:1043-8. https://pubmed.ncbi.nlm.nih.gov/2005942
241. Logan RP, Gummett PA, Misiewicz JJ et al. One week eradication regimen for Helicobacter pylori . Lancet. 1991; 338:1249-52. https://pubmed.ncbi.nlm.nih.gov/1682653
242. Burette A, Glupczynski Y. On: The who’s and when’s of therapy for Helicobacter pylori. 1991; 86:924-5. Letter.
243. Bayerdörffer E, Mannes GA, Sommer A et al. Long-term follow-up after eradication of Helicobacter pylori with a combination of omeprazole and amoxycillin. Scand J Gastroenterol Suppl. 1993; 196:19-25. https://pubmed.ncbi.nlm.nih.gov/8341987
244. Unge P, Ekstrom P. Effects of combination therapy with omeprazole and an antibiotic on H. pylori and duodenal ulcer disease. Scand J Gastroenterol Suppl. 1993; 196:17-8.
245. Hunt RH. Hp and pH: implications for the eradication of Helicobacter pylori . Scand J Gastroenterol Suppl. 1993; 196:12-6. https://pubmed.ncbi.nlm.nih.gov/8341986
246. Malfertheiner P. Compliance, adverse events and antibiotic resistance in Helicobacter pylori treatment. Scand J Gastroenterol Suppl. 1993; 196:34-7. https://pubmed.ncbi.nlm.nih.gov/8341989
247. Bell GD, Powell U. Eradication of Helicobacter pylori and its effect in peptic ulcer disease. Scand J Gastroenterol Suppl. 1993; 196:7-11. https://pubmed.ncbi.nlm.nih.gov/8341990
248. Adamek RJ, Wegener M, Opferkuch W et al. Successful Helicobacter pylori eradication: a systemic effect of antibiotics? Am J Gastroenterol. 1993; 88:792-3. Letter.
249. Bianchi Porro G, Parente F, Lazzaroni M. Short and long term outcome of Helicobacter pylori positive resistant duodenal ulcers treated with colloidal bismuth subcitrate plus antibiotics or sucralfate alone. Gut. 1993; 34:466-9. https://pubmed.ncbi.nlm.nih.gov/8491391 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374304/
250. Reviewers’ comments (personal observations).
251. Marshall BJ. Helicobacter pylori. Am J Gastroenterol. 1994; 89:S116-28.
252. Labenz J, Gyenes E, Rühl GH et al. Amoxicillin plus omeprazole versus triple therapy for eradication of Helicobacter pylori in duodenal ulcer disease: a prospective, randomized, and controlled study. Gut. 1993; 34:1167-70. https://pubmed.ncbi.nlm.nih.gov/8406147 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1375447/
253. Labenz J, Gyenes E, Rühl GH et al. Omeprazole plus amoxicillin: efficacy of various treatment regimens to eradicate Helicobacter pylori . Am J Gastroenterol. 1993; 88:491-5. https://pubmed.ncbi.nlm.nih.gov/8470626
254. Bell GD, Powell KU, Burridge SM et al. Helicobacter pylori eradication: efficacy and side effect profile of a combination of omeprazole, amoxycillin and metronidazole compared with four alternative regimens. Q J Med. 1993; 86:743-50. https://pubmed.ncbi.nlm.nih.gov/8265776
255. Labenz J, Rühl GH, Bertrams J et al. Medium- and high-dose omeprazole plus amoxicillin for eradication of Helicobacter pylori in duodenal ulcer disease. Dig Dis Sci. 1994; 39:1483-7. https://pubmed.ncbi.nlm.nih.gov/8026260
256. Labenz J, Börsch G. Highly significant change of the clinical course of relapsing and complicated peptic ulcer disease after cure of Helicobacter pylori infection. Am J Gastroenterol. 1994; 89:1785-8. https://pubmed.ncbi.nlm.nih.gov/7942667
257. Wang WM, Chen CY, Jan CM et al. Long-term follow-up and serological study after triple therapy of Helicobacter pylori-associated duodenal ulcer. Am J Gastroenterol. 1994; 89:1793-6. https://pubmed.ncbi.nlm.nih.gov/7942669
258. Savarino V, Mela GS, Zentilin P et al. Acid inhibition and amoxicillin activity against Helicobacter pylori . Am J Gastroenterol. 1993; 88:1975-6. https://pubmed.ncbi.nlm.nih.gov/8237959
259. Labenz J, Börsch G. Response to Savarino et al . Am J Gastroenterol. 1993; 88:1976. https://pubmed.ncbi.nlm.nih.gov/8292199
260. Anon. Drugs for treatment of peptic ulcer. Med Lett Drugs Ther. 1994; 36:65-7. https://pubmed.ncbi.nlm.nih.gov/7912812
261. Freston JW. Emerging strategies for managing peptic ulcer disease. Scand J Gastroenterol. 1994; 29(Suppl 201):49-54.
262. Axon ATR. The role of acid inhibition in the treatment of Helicobacter pylori infection. Scand J Gastroenterol. 1994; 29(Suppl 201):16-23.
263. Labenz J, Rühl GH, Bertrams J et al. Medium- or high-dose omeprazole plus amoxicillin eradicates Helicobacter pylori in gastric ulcer disease. Am J Gastroenterol. 1994; 89:726-30. https://pubmed.ncbi.nlm.nih.gov/8172146
264. Walsh JH, Peterson WL. The treatment of Helicobacter pylori infection in the management of peptic ulcer disease. N Engl J Med. 1995; 333:984-91. https://pubmed.ncbi.nlm.nih.gov/7666920
265. Hackelsberger A, Malfertheiner P. A risk-benefit assessment of drugs used in the eradication of Helicobacter pylori infection. Drug Saf. 1996; 15:30-52. https://pubmed.ncbi.nlm.nih.gov/8862962
266. Rauws EAJ, van der Hulst RWM. Current guidelines for the eradication of Helicobacter pylori in peptic ulcer disease. Drugs. 1995; 6:984-90.
267. van der Hulst RWM, Keller JJ, Rauws EAJ et al. Treatment of Helicobacter pylori infection: a review of the world literature. Helicobacter. 1996; 1:6-19. https://pubmed.ncbi.nlm.nih.gov/9398908
268. Lind T, Veldhuyzen van Zanten S, Unge P et al. Eradication of Helicobacter pylori using one-week triple therapies combining omeprazole with two antimicrobials: the MACH I study. Helicobacter. 1996; 1:138-44. https://pubmed.ncbi.nlm.nih.gov/9398894
270. Webb DD. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1136. https://pubmed.ncbi.nlm.nih.gov/8827959
271. Flockhart DA, Richard E, Woosley RL et al. A metabolic interaction between clarithromycin and pimozide may result in cardiac toxicity. Clin Pharmacol Ther. 1996; 59:189.
272. Anon. Pimozide (Orap) contraindicated with clarithromycin (Biaxin) and other macrolide antibiotics. FDA Med Bull. 1996; 26:3.
273. Graham DY, Go MF. Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated. Clin Infect Dis. 1993; 17:293-4. https://pubmed.ncbi.nlm.nih.gov/8399892
274. Murray DM, DuPont HL. Reply. (Evaluation of new antiinfective drugs for Helicobacter pylori infection: revisited and updated.) Clin Infect Dis. 1993; 17: 294-5.
275. George LL, Borody TJ, Andrews P et al. Cure of duodenal ulcer after eradication of H. pylori . Med J Aust. 1990; 153:145-9. https://pubmed.ncbi.nlm.nih.gov/1974027
276. Farrell MK. Dr. Apley meets Helicobacter pylori . J Pediatr Gastroenterol Nutr. 1993; 16:118-9. https://pubmed.ncbi.nlm.nih.gov/8450375
277. Fiocca R, Solcia E, Santoro B. Duodenal ulcer relapse after eradication of Helicobacter pylori . Lancet. 1991; 337:1614. https://pubmed.ncbi.nlm.nih.gov/1675746
278. Marshall BJ. Campylobacter pylori: its link to gastritis and peptic ulcer disease. Clin Infect Dis. 1990; 12(Suppl 1):S87-93.
279. Graham DY, Lew GM, Evans DG et al. Effect of triple therapy (antibiotics plus bismuth) on duodenal ulcer healing: a randomized controlled trial. Ann Intern Med. 1991; 115:266-9. https://pubmed.ncbi.nlm.nih.gov/1854110
280. Rauws EAJ, Tytgat GNJ. Cure of duodenal ulcer with eradication of Helicobacter pylori . Lancet. 1990; 335:1233-5. https://pubmed.ncbi.nlm.nih.gov/1971318
281. Goodwin CS. Duodenal ulcer, Campylobacter pylori, and the “leaking roof” concept. Lancet. 1988; 2:1467-9. https://pubmed.ncbi.nlm.nih.gov/2904580
282. Blaser MJ. Epidemiology and pathophysiology of Campylobacter pylori infections. Clin Infect Dis. 1990; 12(Suppl 1):S99-106.
283. Nomura A, Stemmermann GN, Chyou PH et al. Helicobacter pylori infection and gastric carcinoma among Japanese Americans in Hawaii. N Engl J Med. 1991; 325:1132-6. https://pubmed.ncbi.nlm.nih.gov/1891021
284. Parsonnet J, Friedman GD, Vandersteen DP et al. Helicobacter pylori infection and the risk of gastric carcinoma. N Engl J Med. 1991; 325:1127-31. https://pubmed.ncbi.nlm.nih.gov/1891020
285. The EUROGAST Study Group. Lancet. 1993; 341:1359-62. An international association between Helicobacter pylori infection and gastric cancer.
286. Talley NJ, Zinsmeister AR, Weaver A et al. Gastric adenocarcinoma and Helicobacter pylori infection. J Natl Cancer Inst. 1991; 83:1734-9. https://pubmed.ncbi.nlm.nih.gov/1770552
287. Forman D, Newell DG, Fullerton F et al. Association between infection with Helicobacter pylori and risk of gastric cancer: evidence from a prospective investigation. BMJ. 1991; 302:1302-5. https://pubmed.ncbi.nlm.nih.gov/2059685 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1670011/
288. Forman D. Helicobacter pylori infection: a novel risk factor in the etiology of gastric cancer. J Natl Cancer Inst. 1991; 83:1702-3. https://pubmed.ncbi.nlm.nih.gov/1770545
289. Parsonnet J. Helicobacter pylori and gastric cancer. Gastroenterol Clin North Am. 1993; 22:89-104. https://pubmed.ncbi.nlm.nih.gov/8449573
290. Correa P. Is gastric carcinoma an infectious disease? N Engl J Med. 1991; 325:1170-1.
291. Isaacson PG, Spencer J. Is gastric lymphoma an infectious disease? Hum Pathol. 1993; 24:569-70.
292. Graham DY, Lew GM, Klein PD et al. Effect of treatment of Helicobacter pylori infection on the long-term recurrence of gastric or duodenal ulcer. A randomized, controlled study. Ann Intern Med. 1992; 116:705-8. https://pubmed.ncbi.nlm.nih.gov/1558340
293. Cutler AF, Schubert TT. Patient factors affecting Helicobacter pylori eradication with triple therapy. Am J Gastroenterol. 1993; 88:505-9. https://pubmed.ncbi.nlm.nih.gov/8470629
294. Logan RP, Gummett PA, Hegarty BT et al. Clarithromycin and omeprazole for Helicobacter pylori . Lancet. 1992; 25:340:239.
295. Hentschel E, Brandstätter G, Dragosics B et al. Effect of ranitidine and amoxicillin plus metronidazole on the eradication of Helicobacter pylori and the recurrence of duodenal ulcer. N Engl J Med. 1993; 328:308-12. https://pubmed.ncbi.nlm.nih.gov/8419816
296. Graham DY. Treatment of peptic ulcers caused by Helicobacter pylori . N Engl J Med. 1993; 328:349-50. https://pubmed.ncbi.nlm.nih.gov/8419823
297. Hosking SW, Ling TK, Yung MY et al. Randomised controlled trial of short term treatment to eradicate Helicobacter pylori in patients with duodenal ulcer. BMJ. 1992; 305:502-4. https://pubmed.ncbi.nlm.nih.gov/1392995 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1882868/
298. Bell GD, Powell K, Burridge SM et al. Experience with ’triple’ anti-Helicobacter pylori eradication therapy: side effects and the importance of testing the pre-treatment bacterial isolate for metronidazole resistance. Aliment Pharmacol Ther. 1992; 6:427-35. https://pubmed.ncbi.nlm.nih.gov/1420735
299. NIH Consensus Development Panel on Helicobacter pylori in Peptic Ulcer Disease. Helicobacter pylori in peptic ulcer disease. JAMA. 1994; 272:65-9. https://pubmed.ncbi.nlm.nih.gov/8007082
300. O’Morain C, Gilvarry J. Eradication of Helicobacter pylori in patients with non-ulcer dyspepsia. Scand J Gastroenterol Suppl. 1993; 196:30-3. https://pubmed.ncbi.nlm.nih.gov/8102009
301. Patchett S, Beattie S, Leen E et al. Eradicating Helicobacter pylori and symptoms of non-ulcer dyspepsia. BMJ. 1991; 303:1238-40. https://pubmed.ncbi.nlm.nih.gov/1747644 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1671549/
302. Sloane R, Cohen H. Common-sense management of Helicobacter pylori-associated gastroduodenal disease. Personal views. Gastroenterol Clin North Am. 1993; 22:199-206. https://pubmed.ncbi.nlm.nih.gov/8449567
303. Katelaris P. Eradicating Helicobacter pylori . Lancet. 1992; 339:54. https://pubmed.ncbi.nlm.nih.gov/1345965
304. Talley NJ. The role of Helicobacter pylori in nonulcer dyspepsia. A debate—against. Gastroenterol Clin North Am. 1993; 22(1):153-6 https://pubmed.ncbi.nlm.nih.gov/8449564
305. Borody T, Andrews P, Mancuso N et al. Helicobacter pylori reinfection 4 years post-eradication. Lancet. 1992; 339:1295. https://pubmed.ncbi.nlm.nih.gov/1349686
306. Hixson LJ, Kelley CL, Jones WN et al. Current trends in the pharmacotherapy for peptic ulcer disease. Arch Intern Med. 1992; 152:726-32. https://pubmed.ncbi.nlm.nih.gov/1558429
307. Fennerty MB. Practice guidelines for treatment of peptic ulcer disease. JAMA. 1996; 276:1135. https://pubmed.ncbi.nlm.nih.gov/8827957
308. Hunt RH. pH and Hp—gastric acid secretion and Helicobacter pylori: implications for ulcer healing and eradication of the organism. Am J Gastroenterol. 1993; 88:481-3. https://pubmed.ncbi.nlm.nih.gov/8470623
309. Labenz J, Borsch G. Evidence for the essential role of Helicobacter pylori in gastric ulcer disease. Gut. 1994; 35:19-22. https://pubmed.ncbi.nlm.nih.gov/8307443 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1374625/
310. Fennerty MB. Helicobacter pylori. Ann Intern Med. 1994; 154:721-7.
311. Adamek RJ, Wegener M, Labenz J et al. Medium-term results of oral and intravenous omeprazole/amoxicillin Helicobacter pylori eradication therapy. Am J Gastroenterol. 1994; 89:39-42. https://pubmed.ncbi.nlm.nih.gov/8273795
312. O’Brien B, Goeree R, Mohamed AH et al. Cost-effectiveness of Helicobacter pylori eradication for the long-term management of duodenal ulcer in Canada. Arch Intern Med. 1995; 155:1958-64. https://pubmed.ncbi.nlm.nih.gov/7575049
313. Fennerty MB. “Cure” of Helicobacter pylori: clinically indicated and economically wise! Arch Intern Med. 1995; 155:1929-31. Editorial.
314. Imperiale TF, Speroff T, Cebul RD et al. A cost analysis of alternative treatments for duodenal ulcer. Ann Intern Med. 1995; 123:665-72. https://pubmed.ncbi.nlm.nih.gov/7574221
315. Vakil N, Fennerty MB. Cost-effectiveness of treatment regimens for the eradication of Helicobacter pylori in duodenal ulcer. Am J Gastroenterol. 1996; 91:239-45. https://pubmed.ncbi.nlm.nih.gov/8607487
316. Sonnenberg A, Townsend WF. Costs of duodenal ulcer therapy with antibiotics. Arch Intern Med. 1995; 155:922-8. https://pubmed.ncbi.nlm.nih.gov/7726700
317. Graham KS, Malaty H, el-Zimaity HM et al. Variability with omeprazole-amoxicillin combinations for treatment of Helicobacter pylori infection. Am J Gastroenterol. 1995; 90:1415-8. https://pubmed.ncbi.nlm.nih.gov/7661160
318. Bell GD. Anti-Helicobacter pylori therapy: clearance, elimination, or eradication? Lancet. 1991; 337:310-1. Letter.
319. Graham DY, Börsch GM. The who’s and when’s of therapy for Helicobacter pylori . Am J Gastroenterol. 1990; 85:1552-5. https://pubmed.ncbi.nlm.nih.gov/2252013
320. Logan RP, Polson RJ, Baron JH et al. Follow-up after anti-Helicobacter pylori treatment. Lancet. 1991; 337:562-3. https://pubmed.ncbi.nlm.nih.gov/1671932
321. Oderda G, Dell’Olio D, Morra I et al. Campylobacter pylori gastritis: long term results of treatment with amoxycillin. Arch Dis Child. 1989; 64:326-9. https://pubmed.ncbi.nlm.nih.gov/2495776 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1791940/
322. Peura DA, Graham DY. Helicobacter pylori: consensus reached: peptic ulcer is on the way to becoming an historic disease. Am J Gastroenterol. 1994; 89:1137-9. https://pubmed.ncbi.nlm.nih.gov/8053422
323. Borody TJ, Andrews J, Shortis NP et al. Optimal H.pylori [sic] (HP) therapy—a combination of omeprazole and triple therapy (TT). Gastroenterology. 1994; 106:A55.
324. Glaxo Wellcome. Tritec (ranitidine bismuth citrate) tablets prescribing information. Research Triangle Park, NC: 1996 Aug.
325. Rosioru C, Glassman MS, Halata MS et al. Esophagitis and Helicobacter pylori in children: incidence and therapeutic implications. Am J Gastroenterol. 1993; 88:510-3. https://pubmed.ncbi.nlm.nih.gov/8470630
326. Drumm B. Helicobacter pylori. Arch Dis Child. 1990; 65:1278-82. https://pubmed.ncbi.nlm.nih.gov/2248546 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1792590/
327. Bourke B, Jones N, Sherman P. Helicobacter pylori infection and peptic ulcer disease in children. Pediatr Infect Dis J. 1996; 15:1-13. https://pubmed.ncbi.nlm.nih.gov/8684868
328. Rowland M, Drumm B. Helicobacter pylori infection and peptic ulcer disease in children. Curr Opin Pediatr. 1995; 7:553-9. https://pubmed.ncbi.nlm.nih.gov/8541956
329. Yeung CK, Fu KH, Yuen KY et al. Helicobacter pylori and associated duodenal ulcer. Arch Dis Child. 1990; 65:1212-6. https://pubmed.ncbi.nlm.nih.gov/2248531 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1792624/
330. Sullivan PB. Helicobacter pylori in children. Baillieres Clin Gastroenterol. 1995; 9:519-28. https://pubmed.ncbi.nlm.nih.gov/8563051
331. Ofman JJ, Etchason J, Fulleron S et al. Management strategies for H. pylori-seropositive patients with dyspepsia: clinical and economic consequences. Ann Intern Med. 1997; 126:280-91. https://pubmed.ncbi.nlm.nih.gov/9036800
332. Rabeneck L, Graham DY. Helicobacter pylori: when to test, when to treat. Ann Intern Med. 1997; 126:315-6. https://pubmed.ncbi.nlm.nih.gov/9036804
333. Dautzenberg B, Truffot C, Legris S et al. Activity of clarithromycin against Mycobacterium avium infection in patients with the acquired immune deficiency syndrome: a controlled clinical trial. Am Rev Respir Dis. 1991; 144(3 Part 1):564-9. https://pubmed.ncbi.nlm.nih.gov/1832527
335. TAP Pharmaceuticals Inc. Prevacid (lansoprazole) delayed-release capsules prescribing information. Deerfield, IL; 1998 Jun.
336. Langtry HD, Wilde MI. Lansoprazole: an update of its pharmacological properties and clinical efficacy in the management of acid-related disorders. Drugs. 1997; 54:473-500. https://pubmed.ncbi.nlm.nih.gov/9279507
337. Treiber G, Ammon S, Klotz U. Age-dependent eradication of Helicobacter pylori with dual therapy. Aliment Pharmacol. 1997; 11:711-8.
338. Yasui N, Otani K, Kaneko S et al. Carbamazepine toxicity induced by clarithromycin coadministration in psychiatric patients. Int Clin Psychopharmacol. 1997. 12:225-9.
339. Sekkarie MA. Torsades de pointes in two chronic renal failure patients treated with cisapride and clarithromycin. Am J Kidney Dis. 1997; 30:437-9. https://pubmed.ncbi.nlm.nih.gov/9292575
340. Paar D, Terjung B, Sauerbruch T. Life-threatening interaction between clarithromycin and disopyramide. Lancet. 1997; 349:326-7. https://pubmed.ncbi.nlm.nih.gov/9024381
341. Abbott Laboratories. Norvir (ritonavir) capsules and oral solution prescribing information. North Chicago, IL; 2000 Dec.
343. Piscitelli SC, Flexner C, Minor JR et al. Drug interactions in patients infected with human immunodeficiency virus. Clin Infect Dis. 1996; 23:685-93. https://pubmed.ncbi.nlm.nih.gov/8909827
344. Hardy DJ, Swanson RN, Rode RA et al. Enhancement of the in vitro and in vivo activities of clarithromycin against Haemophilus influenzae by 14-hydroxy clarithromycin, its major metabolite in humans. Antimicrob Agents Chemother. 1990; 34:1407-13. https://pubmed.ncbi.nlm.nih.gov/2143642 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC175991/
345. Dajani AS, Taubert KA, Wilson W et al. Prevention of bacterial endocarditis: recommendations by the American Heart Association. JAMA. 1997; 277:1794-1801. https://pubmed.ncbi.nlm.nih.gov/9178793
346. Durack DT, Kaplan EL, Bisno AL. Apparent failures of endocarditis prophylaxis: analysis of 52 cases submitted to a national registry. JAMA. 1983; 250:2318-22. https://pubmed.ncbi.nlm.nih.gov/6632128
350. American Thoracic Society. Supplement: American Thoracic Society—Diagnosis and treatment of disease caused by nontuberculous mycobacteria. Am Rev Respir Crit Care Med. 1997; 156(2 Part 2):S1-19.
351. Amsden GW, Peloquin CA, Berning SE. The role of advance generation macrolides in the prophylaxis and treatment of Mycobacterium avium complex (MAC) infections. Drugs. 1997; 54:69-80. https://pubmed.ncbi.nlm.nih.gov/9211081
352. Klausner MA. Dear doctor letter regarding important safety information on Hismanal (astemizole). Titusville, NJ: Janssen Pharmaceutica; 1998 Feb.
353. TAP Pharmaceuticals. PrevPac (lansoprazole 30-mg capsules, amoxicillin 500-mg capsules, and clarithromycin 500-mg tablets) prescribing information. Deerfield, IL; 1997 Dec.
354. Parke-Davis. Lipitor (atorvastatin calcium) tablets prescribing information. Morris Plains, NJ; 1997 Jan.
355. Grunden JW, Fisher KA. Lovastatin-induced rhabdomyolysis possibly associated with clarithromycin and azithromycin. Ann Pharmacother. 1997; 31:859-63. https://pubmed.ncbi.nlm.nih.gov/9220046
356. Sandoz. Lescol (fluvastatin sodium) capsules prescribing information. East Hanover, NJ: 1996 Mar.
357. Ayanian JZ, Fuchs CS, Stone RM. Lovastatin and rhabdomyolysis. Ann Intern Med. 1988; 109:682. https://pubmed.ncbi.nlm.nih.gov/3421582
358. Bristol-Myers Squibb. Pravachol (pravastatin sodium) tablets prescribing information. Princeton, NJ; 1996 Jul.
359. Merck. Mevacor (lovastatin) tablets prescribing information. West Point, PA; 1997 Mar.
360. East C, Alivizatos PA, Grundy SM et al. Rhabdomyolysis in patients receiving lovastatin after cardiac transplantation. N Engl J Med. 1988; 318:47-8. https://pubmed.ncbi.nlm.nih.gov/3275892
361. Norman DJ, Illingworth DR, Munson J et al. Myolysis and acute renal failure in a heart-transplant recipient receiving lovastatin. N Engl J Med. 1988; 318:46-7. https://pubmed.ncbi.nlm.nih.gov/3275891
362. Tobert JA. Rhabdomyolysis in patients receiving lovastatin after cardiac transplantation. N Engl J Med. 1988; 318:48. https://pubmed.ncbi.nlm.nih.gov/3257291
363. Corpier CL, Jones PH, Suki WN et al. Rhabdomyolysis and renal injury with lovastatin use: report of two cases in cardiac transplant recipients. JAMA. 1988; 260:239-41. https://pubmed.ncbi.nlm.nih.gov/3290520
364. Merck & Co, Inc. Zocor (simvastatin) tablets prescribing information. West Point, PA; 1997 Jun.
365. Bizzaro N, Bagolin E, Milani L et al. Massive rhabdomyolysis and simvastatin. Clin Chem. 1992; 38:1504. https://pubmed.ncbi.nlm.nih.gov/1643724
366. Deslypere JP, Vermeulen A. Rhabdomyolysis and simvastatin. Ann Intern Med. 1991; 114:342. https://pubmed.ncbi.nlm.nih.gov/1987887
367. Salcedo JA, Al-Kawas F. Treatment of Helicobacter pylori infection. Arch Intern Med. 1998; 158:842-51. https://pubmed.ncbi.nlm.nih.gov/9570169
368. Jablonowski H, Fatkenheuer G, Youle M et al. Ancillary benefits of Mycobacterium avium-intracellulare complex prophylaxis with clarithromycin in HIV-infected patients. Drugs. 1997; 54(Suppl 2):16-22. https://pubmed.ncbi.nlm.nih.gov/9358196
369. Anon. Round-table discussion. Drugs. 1997; 54(Suppl 2):28-9.
370. Gavura SR, Nusinowitz S. Leukocytoclastic vasculitis associated with clarithromycin. Ann Pharmacother. 1998; 32:543-5. https://pubmed.ncbi.nlm.nih.gov/9606474
371. de Vega T, Blanco S, Lopez C et al. Clarithromycin-induced leukocytoclastic vasculitis. Eur J Clin Microbiol Infect Dis. 1993; 12:563. https://pubmed.ncbi.nlm.nih.gov/8404922
372. Rosina P, Chieregato C, Schena D. Fixed drug eruption from clarithromycin. Contact Derm. 1998; 38:105. https://pubmed.ncbi.nlm.nih.gov/9506224
373. Hafner R, Bethel J, Power M et al. Tolerance and pharmacokinetic interactions of rifabutin and clarithromycin in human immunodeficiency virus-infected volunteers. Antimicrob Agents Chemother. 1998; 42:631-9. https://pubmed.ncbi.nlm.nih.gov/9517944 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC105510/
374. Benson CA, Williams PL, Cohn DL et al. Clarithromycin or rifabutin alone or in combination with primary prophylaxis of Mycobacterium avium complex disease in patients with AIDS: a randomized, double-blind, placebo-controlled trial. J Infect Dis. 2000; 181:1289-97. https://pubmed.ncbi.nlm.nih.gov/10762562
375. Shafran SD, Singer J, Zarowny DP et al. Determinants of rifabutin-associated uveitis in patients treated with rifabutin, clarithromycin, and ethambutol for Mycobacterium avium complex bacteremia: a multivariate analysis. Canadian HIV Trials Network Protocol 010 Study Group. J Infect Dis. 1998; 177(1):252-5. https://pubmed.ncbi.nlm.nih.gov/9419201
376. Nichols CW. Mycobacterium avium complex infection, rifabutin, and uveitis—is there a connection? Clin Infect Dis. 1996; 22(Suppl 1):S43-7; discussion S47-9.
377. Astra Merck. Prilosec (omeprazole) delayed-release capsules prescribing information. West Point, PA; 1998 Jun.
378. SmithKline Beecham. Amoxil (amoxicillin) capsules, tablets, chewable tablets, and powder for oral suspension prescribing information. Philadelphia, PA; 1998 Jul.
380. Inderlied CB, Kolonoski PT, Wu M et al. In vitro and in vivo activity of azithromycin (CP 62,993) against the Mycobacterium avium complex. J Infect Dis. 1989; 159:994-7.
381. Pfizer Labs. Zithromax (azithromycin) capsules, tablets, oral suspension prescribing information. New York, NY; 1996 Jun.
382. Yew WW, Piddock LJV, Li MSK et al. In-vitro activity of quinolones and macrolides against mycobacteria. J Antimicrob Chemother. 1994; 34:343-51. (IDIS 336427)
383. Perronne C, Gikas A, Truffot-Pernot C et al. Activities of sparfloxacin, azithromycin, temafloxacin, and rifapentine compared with that of clarithromycin against multiplication of Mycobacterium avium complex within human macrophages. Antimicrob Agents Chemother. 1991; 35:1356-9.
384. Hammerschlag MR, Golden NH, Oh MK et al. Single dose of azithromycin for the treatment of genital chlamydial infections in adolescents. J Pediatr. 1993; 122:961-5.
385. Anon. WHO system finds 13 drugs with AEs not in PDR, Martindale. F-D-C Rep. 1998;(Vol?):16.
386. Di Mario F, Dal Bo N, Grassi SA et al. Azithromycin for the cure of Helicobacter pylori infection. Am J Gastroenterol. 1996; 91:264-7. https://pubmed.ncbi.nlm.nih.gov/8607490
387. Dattwyler RJ, Grunwaldt E, Luft BJ. Clarithromycin in treatment of early Lyme disease: a pilot study. Antimicrob Agents Chemother. 1996; 40:468-9. https://pubmed.ncbi.nlm.nih.gov/8834900 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC163136/
388. Spach DH, Liles WC, Campbell GL et al. Tick-borne diseases in the United States. N Engl J Med. 1993; 329:936-47.
389. Jantausch BA. Lyme disease, Rocky Mountain spotted fever, ehrlichiosis: emerging and established challenges for the clinician. Ann Allergy. 1994; 73:4-11.
390. Nadelman RB, Wormser GP. Erythema migrans and early Lyme disease. Am J Med. 1995; 98(4A):15-23S.
391. Sigal LH. Early disseminated Lyme disease: cardiac manifestations. Am J Med. 1995; 98(4A):25-8S.
392. Steere AC. Musculoskeletal manifestations of Lyme disease. Am J Med. 1995; 98(4A):44-8S.
393. Anon. The choice of antibacterial drugs. Med Lett Treat Guid. 2004; 2:13-26.
394. Nadelman RB, Wormser GP. Lyme borreliosis. Lancet. 1998; 352:557-65. https://pubmed.ncbi.nlm.nih.gov/9716075
395. Anon. Treatment of Lyme disease. Med Lett Drugs Ther. 1997; 39:47-8. https://pubmed.ncbi.nlm.nih.gov/9150689
396. Committee on Infectious Diseases, American Academy of Pediatrics. Red book: 2003 report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003.
397. Rahn DW, Felz MW. Lyme disease update. Current approach to early, disseminated, and late disease. Postgrad Med. 1998;103:51-4, 57-9, 63-4.
398. Nocton JJ, Steere AC. Lyme disease. Adv Intern Med. 1995; 40:69-117.
399. Perri F, Festa V, Andriulli A. Treatment of antibiotic-resistant Helicobacter pylori infection. N Engl J Med. 1998; 339:53. https://pubmed.ncbi.nlm.nih.gov/9660694
400. Johnson S, Gerding DN. Clostridium difficile-associated diarrhea. Clin Infect Dis. 1998; 26:1027-36. https://pubmed.ncbi.nlm.nih.gov/9597221
401. Gerding DN, Johnson S, Peterson LR et al for the Society for Healthcare Epidemiology of America. Position paper on Clostridium difficile-associated diarrhea and colitis. Infect Control Hosp Epidemiol. 1995; 16:459-77. https://pubmed.ncbi.nlm.nih.gov/7594392
402. Fekety R for the American College of Gastroenterology Practice Parameters Committee. Guidelines for the diagnosis and management of Clostridium difficile-associated diarrhea and colitis. Am J Gastroentero. 1997; 92:739-50.
403. American Society of Health-System Pharmacists Commission on Therapeutics. ASHP therapeutic position statement on the preferential use of metronidazole for the treatment of Clostridium difficile-associated disease. Am J Health-Syst Pharm. 1998; 55:1407-11. https://pubmed.ncbi.nlm.nih.gov/9659970
404. Wilcox MH. Treatment of Clostridium difficile infection. J Antimicrob Chemother. 1998; 41(Suppl C):41-6. https://pubmed.ncbi.nlm.nih.gov/9630373
405. McColl K, Murray L, El-Omar E et al. Symptomatic benefit from eradicating Helicobacter pylori infection in patients with nonulcer dyspepsia. N Engl J Med. 1998; 339:1869-74. https://pubmed.ncbi.nlm.nih.gov/9862941
406. Talley NJ, Vakil N, Ballard ED II et al. Absence of benefit of eradicating Helicobacter pylori in patients with nonulcer dyspepsia. N Engl J Med. 1999; 341:1106-11. https://pubmed.ncbi.nlm.nih.gov/10511608
407. Blum AL, Talley NJ, O’Morain C et al. Lack of effect of treating Helicobacter pylori infection in patients with nonulcer dyspepsia. N Engl J Med. 1998; 339:1875-81. https://pubmed.ncbi.nlm.nih.gov/9862942
408. Anon. Drugs for the treatment of otitis media in children. Med Lett Drugs Ther. 1994; 36:19-21. https://pubmed.ncbi.nlm.nih.gov/8107649
410. Giebink GS, Canafax DM, Kempthorne J. Antimicrobial treatment of acute otitis media. J Pediatr. 1991; 119:495-500. https://pubmed.ncbi.nlm.nih.gov/1880671
411. Pichichero ME. Assessing the treatment of alternatives for acute otitis media. Pediatr Infect Dis J. 1994; 13:S27-34. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2993315/
412. Klein JO. Selection of oral antimicrobial agents for otitis media and pharyngitis. Infect Dis Clin Pract. 1995; 4(Suppl 2):S88-94.
413. Pichichero ME, Cohen R. Shortened course of antibiotic therapy for acute otitis media, sinusitis and tonsillopharyngitis. Pediatr Infect Dis J. 1997; 16:680-95. https://pubmed.ncbi.nlm.nih.gov/9239773
414. McCracken GH. Treatment of acute otitis media in an era of increasing microbial resistance. Pediatr Infect Dis J. 1998; 17:576-9. https://pubmed.ncbi.nlm.nih.gov/9655564
415. Klein JO. Otitis Media. Clin Infect Dis J. 1994; 19:823-33.
416. Klein JO. Clinical implications of antibiotic resistance for management of acute otitis media. Pediatr Infect Dis J. 1998; 17:1084-9. https://pubmed.ncbi.nlm.nih.gov/9850003
417. Gooch WM, Philips A, Rhoades R et al. Comparison of the efficacy, safety and acceptability of cefixime and amoxicillin/clavulanate in acute otitis media. Pediatr Infect Dis J. 1997; 16(Suppl):21-4.
418. Kafetzis DA. Multi-investigator evaluation of the efficacy and safety of cefprozil, amoxicillin-clavulanate, cefixime and cefaclor in the treatment of acute otitis media, Eur J Clin Microbiol Infect Dis. 1994; 13:857-65.
419. Adler M, McDonald PJ, Trostmann U et al. Cefdinir versus amoxicillin/clavulanic acid in the treatment of suppurative acute otitis media in children. Eur J Clin Microbiol Infect Dis. 1997; 16:214-9. https://pubmed.ncbi.nlm.nih.gov/9131324
420. Gooch WM, Adelglass J, Kelsey DK et al. Loracarbef versus clarithromcyin in children with acute otitis media with effusion. Clin Ther. 1999; 21:711-21. https://pubmed.ncbi.nlm.nih.gov/10363736
421. Hoppe HL, Johnson CE. Otitis media: focus on antimicrobial resistance and new treatment options. Am J Health-Syst Pharm. 1998; 55:1881-97. https://pubmed.ncbi.nlm.nih.gov/9784768
422. Bluestone CD. Ear and mastoid infections. In: Gorbach SL, Bartlett JG, Blacklow NR, eds. Infectious Diseases. Philadelphia, PA: WB Saunders; 1998:530-9.
423. Dowell SF, Butler JC, Giebink GS et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the drug-resistant Streptococcal pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999; 18:1-9. https://pubmed.ncbi.nlm.nih.gov/9951971
424. Blumer JL. Pharmacokinetics and pharmacodynamics of new and old antimicrobial agents for acute otitis media. Pediatr Infect Dis J. 1998; 17:1070-5. https://pubmed.ncbi.nlm.nih.gov/9850001
425. Jacobs MR. Antibiotic-resistant Streptococcus pneumoniae in acute otitis media: overview and update. Pediatr Infect Dis J. 1998; 17:947-52. https://pubmed.ncbi.nlm.nih.gov/9802651
426. Poole MD. Implications of drug-resistant Streptococcus pneumoniae for otitis media. Pediatr Infect Dis J. 1998; 17:953-6. https://pubmed.ncbi.nlm.nih.gov/9802652
427. Steere AC. Lyme disease. N Engl J Med. 2001; 345:115-25. https://pubmed.ncbi.nlm.nih.gov/11450660
428. Wormser GP, Nadelman RB, Dattwyler R et al. Infectious Diseases Society of America. Practice guidelines for the treatment of Lyme disease. Clin Infect Dis. 2000; 31(Suppl 1):S1-14. https://pubmed.ncbi.nlm.nih.gov/10982743 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2573401/
429. Thompson C, Spielman A, Krause P. Coinfecting deer-associated zoonoses: Lyme disease, babesiosis, and ehrlichiosis. Clin Infect Dis. 2000; 33:676-85.
430. Bristol-Myers Squibb. Reyataz (atazanavir sulfate) capsules prescribing information. Princeton, NJ; 2004 Oct.
431. American Academy of Pediatrics and American Academy of Family Physicians Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004: 113:1451-65.
432. Roche Pharmaceuticals. Fortovase (saquinavir) soft gelatin capsules prescribing information. Nutley, NJ; 2003 Dec.
433. Abbott. Kaletra (lopinavir/ritonavir) capsules and oral solution prescribing information. North Chicago, IL; 2004 Feb.
434. Abbott. Norvir (ritonavir) soft gelatin capsules and oral solution prescribing information. Nutley, NJ; 2005 Mar 28.
435. Bristol-Myers Squibb. Sustiva (efavirenz) capsules and tablets prescribing information. Princeton, NJ; 2004 Aug.
436. Boehringer Ingelheim. Viramune (nevirapine) tablets and oral suspension prescribing information. Ridgefield, CT; 2005 Jan 11.
437. Panel on Clinical Practices for Treatment of HIV Infection of the Department of Health and Human Services (DHHS). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (Apr 7, 2005). From the US Department of Health and Human Services HIV/AIDS Information Services (HIV.gov) website. https://clinicalinfo.hiv.gov/en/guidelines
438. GlaxoSmithKline. Agenerase (amprenavir) capsules prescribing information. Research Triangle Park, NC; 2004 Feb.
439. Brophy DF, Israel DS, Pastor A et al. Pharmacokinetic interaction between amprenavir and clarithromycin in healthy male volunteers. Antimicrob Agents Chemother. 2000; 44:978-84. https://pubmed.ncbi.nlm.nih.gov/10722500 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC89801/
440. GlaxoSmithKline. Lexiva (fosamprenavir calcium) tablets prescribing information. Research Triangle Park, NC; 2004 Dec.
441. GlaxoSmithKline, Research Triangle Park, NC: personal communication.
442. Roche Laboratories. Invirase (saquinavir mesylate) capsules prescribing information. Nutley, NJ; 2004 Dec.
443. Merck & Company Inc. Crixivan (indinavir sulfate) capsules prescribing information. West Point, PA; 2004 May.
444. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-infected adults and adolescents: recommendations from CDC, the National Institutes of Health, and the HIV Medicine Association/Infectious Diseases Society of America. MMWR Morb Mortal Wkly Rep. 2004; 53(No. RR-15):1-112. https://pubmed.ncbi.nlm.nih.gov/14724557 https://www.cdc.gov/mmwr/PDF/rr/rr5315.pdf
445. Centers for Disease Control and Prevention. Treating opportunistic infections among HIV-exposed and infected children: recommendations from CDC, the National Institutes of Health, and the Infectious Diseases Society of America. MMWR Morb Mortal Wkly Rep. 2004; 53(No. RR-14):1-92. https://pubmed.ncbi.nlm.nih.gov/14724557 https://www.cdc.gov/mmwr/PDF/rr/rr5314.pdf
446. Richter SS, Heilmann KP, Beekmann SE et al. Macrolide-resistant Streptococcus pyogenes in the United States, 2002-2003. Clin Infect Dis. 2005; 41:599-608. https://pubmed.ncbi.nlm.nih.gov/16080080
447. Roig J, Rello J. Legionnaires’ disease: a rational approach to therapy. J Antimicrob Chemother. 2003; 51:1119-29. https://pubmed.ncbi.nlm.nih.gov/12668578
448. Amsden GW. Treatment of Lgionnaires’ disease. Drugs. 2005; 65:605-14. https://pubmed.ncbi.nlm.nih.gov/15748096
449. Mandell LA, Bartlett JG, Dowell SF et al. Update of practice guidelines for the management of community-acquired pneumonia in immunocompetent adults. Clin Infect Dis. 2003; 37:1405-33. https://pubmed.ncbi.nlm.nih.gov/14614663
450. Anon. Drugs for pneumonia. Med Lett Treat Guid. 2003; 1:83-8.
451. Field SK, Fisher D, Cowie RL. Mycobacterium avium complex pulmonary disease in patients without HIV infection. Chest. 2004; 126:566-81. https://pubmed.ncbi.nlm.nih.gov/15302746
452. von Konig CHW. Use of antibiotics in the prevention and treatment of pertussis. Pediatr Infect Dis. 2005; 24:S66-8.
453. Langley JM, Halperin SA, Boucher FD et al. Azithromycin is as effective as and better tolerated than erythromycin estolate for the treatment of pertussis. Pediatrics. 2004; 114:e96-101. https://pubmed.ncbi.nlm.nih.gov/15231980
454. Lebel MH, Mehra S. Efficacy and safety of clarithromycin versus erythromycin for the treatment of pertussis: a prospective, randomized, single blind trial. Pediatr Infect Dis J. 2001; 20:1149-54. https://pubmed.ncbi.nlm.nih.gov/11740322
455. Novartis. Enablex (darifenacin hydrobromide) extended-release tablets prescribing information. East Hanover, NJ; 2004 Dec.
456. Genentech. Tarceva (erlotinib) tablets prescribing information. San Francisca, CA; 2004.
457. Sepracor. Lunesta (Eszopiclone) tablets prescribing information. Marlborough, MA; 2005 Feb.
458. Maniu CV, Hellinger WC, Chu SY et al. Failure of treatment for chronic Mycobacterium abscessus meningitis despite adequate clarithromycin levels in cerebrospinal fluid. Clin Infect Dis. 2001; 33:745-8. https://pubmed.ncbi.nlm.nih.gov/11486298
459. Schmidt T, Froula J, Tauber MG. Clarithromycin lacks bactericidal activity in cerebrospinal fluid in experimental pneumococcal meningitis. J Antimicrob Chemother. 1993; 32:627-32. https://pubmed.ncbi.nlm.nih.gov/8288505
460. Sedlmayr T, Peters F, Raasch W et al. Clarithromycin, a new macrolide antibiotic. Effectiveness in puerperal infections and pharmacokinetics in breast milk. Geburtshilfe Frauenheilkd. 1993; 53:488-91. https://pubmed.ncbi.nlm.nih.gov/8370491
461. Kobayashi I, Hasegawa M, Kanayama A et al. Alarming trend of clarithromycin-resistsant Streptococcus pyogenes in Japan (1998-2002). J Infect Chemother. 2005; 11:56-8. https://pubmed.ncbi.nlm.nih.gov/15856371
462. Dytoc MT, Honish L, Shandro C et al. Clinical, microbiological, and epidemiological findings of an outbreak of Mycobacterium abscessus hand-and-foot disease. Diagn Microbiol Infect Dis. 2005. In press.
463. Hung IFN, Wu VCC, Cheng BSF et al. Fatal interaction between clarithromycin and colchicine in patients with renal insufficiency: a retrospective study. Clin Infect Dis. 2005; 41:291-300. https://pubmed.ncbi.nlm.nih.gov/16007523
464. Anon. Drugs for parasitic infections. Med Lett Drugs Ther. Aug 2004. From the Medical Letter website. http://www.medletter.com
465. Gaubitz M, Herrmann M, Shahin M et al. Cat scratch disease (bartonellosis) mimicking an SLE flare. Lupus. 2001; 10:883-5. https://pubmed.ncbi.nlm.nih.gov/11787880
467. Sandoz. Clarithromycin tablets prescribing information. Princeton, NJ; 2017 Sep.
468. US Food and Drug Administration. FDA drug safety communication: FDA review finds additional data supports the potential for increased long-term risks with antibiotic clarithromycin (Biaxin) in patients with heart disease. 2018 Feb 22. From FDA website. https://www.fda.gov/Drugs/DrugSafety/ucm597289.htm
469. Jespersen C, Als-Nielsen B, Damgaard M et al. Randomised placebo controlled multicentre trial to assess short term clarithromycin for patients with stable coronary heart disease: CLARICOR trial. BMJ. 2006; 332:22-7. https://pubmed.ncbi.nlm.nih.gov/16339220
470. Winkel P, Hilden J, Hansen J et al. Clarithromycin for stable coronary heart disease increases all-cause and cardiovascular mortality and cerebrovascular morbidity over 10 years in the CLARICOR randomised, blinded clinical trial. Int J Cardiol. 2015; 182:459-65. https://pubmed.ncbi.nlm.nih.gov/25602299
Related/similar drugs
Frequently asked questions
- What is the Best Antibiotic for Strep Throat?
- What are the best antibiotics for pneumonia?
- Do statins cause rhabdomyolysis, and how is it treated?
- Can Biaxin cause headaches?
- Can I drink alcohol while taking clarithromycin?
- Can clarithromycin be used to treat UTI's?
More about clarithromycin
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (853)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: macrolides
- Breastfeeding
- En español