Amoxicillin/Clavulanate (Monograph)
Drug class: Aminopenicillins
VA class: AM052
Chemical name: [2R-(2α,3Z,5α)]-3-(2-Hydroxyethylidene)-7-oxo-4-oxa-1-azabicyclo[3.2.0]heptane-2-carboxylic acid monopotassium salt mixt. with [2S-[2α,5α,6β(S*)]]-6-[[Amino(4-hydroxyphenylacetyl]amino]-3,3-dimethyl-7-oxo-4-thia-1-azabicyclo[3.2.0] heptane-2-carboxylic acid trihydrate
Molecular formula: C16H19N3O5S•3H2O C8H8KNO5
CAS number: 74469-00-4
Amoxicillin and Clavulanate Potassium is also contained as an ingredient in the following combinations:
Amoxicillin and Clavulanate Potassium
Introduction
Antibacterial; β-lactam antibiotic; fixed combination containing amoxicillin (an aminopenicillin) and clavulanate potassium (a β-lactamase inhibitor).1 61
Uses for Amoxicillin/Clavulanate
Otitis Media
Treatment of acute otitis media (AOM) caused by β-lactamase producing H. influenzae or M. catarrhalis.1 3 61 67 74 77 78 81 82 88 89 92 93 94 95 96 98 99 101 115 AAP, AAFP, CDC, and others recommend the fixed combination of amoxicillin and clavulanate (amoxicillin/clavulanate) instead of amoxicillin for initial treatment of AOM in those with severe illness (moderate to severe otalgia or fever ≥39°C)115 or when the infection is suspected of being caused by β-lactamase-producing Haemophilus influenzae or Moraxella catarrhalis.74 76 77 78 81 89 115
Treatment of persistent or recurrent AOM caused by H. influenzae (including β-lactamase-producing strains), M. catarrhalis (including β-lactamase-producing strains), or Streptococcus pneumoniae (penicillin MIC ≤2 mcg/mL) in pediatric patients.76 79 81 89 90 91 97 115 Drug of choice for retreatment of AOM that has not responded to other anti-infectives81 89 90 100 107 115 (e.g., no response to amoxicillin within 48–72 hours).115 Not indicated for AOM caused by S. pneumoniae with penicillin MIC ≥4 mcg/mL.3
Has been used for management of otitis media with effusion† [off-label] (OME).68 94 102 107 Anti-infectives not usually recommended;102 103 104 105 107 116 they provide only limited benefit in enhancing resolution of effusion and may promote resistance.103 104 105 106 107 AAP, AAFP, and others recommend watchful waiting for 3 months from date of effusion onset or diagnosis in those 2 months to 12 years of age who are not at risk for speech, language, or learning problems; some suggest a short course of anti-infectives may be considered for possible short-term benefits when parent and/or caregiver expresses a strong aversion to impending surgery.116 If anti-infectives are used for treatment, amoxicillin/clavulanate or amoxicillin recommended.102 107
Pharyngitis and Tonsillitis
Treatment of symptomatic patients who have multiple, recurrent episodes of pharyngitis known to be caused by S. pyogenes (group A β-hemolytic streptococci)† [off-label].75 76 80
Not a drug of choice for treatment of streptococcal pharyngitis and tonsillitis,61 75 76 80 but one of several possible alternatives recommended by AAP, IDSA , and AHA when multiple episodes occur and the patient fails to respond to drugs of choice (oral penicillin V, IM penicillin G benzathine, oral amoxicillin).75 76 80
Consider that multiple, recurrent episodes of symptomatic pharyngitis occurring within several months to years may indicate that the patient is a streptococcal carrier experiencing repeated episodes of nonstreptococcal (e.g., viral) pharyngitis;75 80 treatment not usually recommended for streptococcal pharyngeal carriers.75 76 80
Respiratory Tract Infections
Treatment of acute sinusitis and lower respiratory tract infections caused by susceptible H. influenzae1 2 5 17 53 67 68 69 or M. catarrhalis.1 2 5 17 53 59
Treatment of acute sinusitis or community-acquired pneumonia (CAP) caused by or suspected to be caused by β-lactamase-producing pathogens (i.e., H. influenzae, M. catarrhalis, H. parainfluenzae, Klebsiella pneumoniae, oxacillin-susceptible Staphylococcus aureus).4 61 305 Treatment of acute sinusitis or CAP caused by or suspected of being caused by S. pneumoniae with reduced penicillin susceptibility (i.e., penicillin MIC 2 mcg/mL).4 Not indicated for treatment of infections caused by S. pneumoniae with penicillin MIC ≥4 mcg/mL.4
ATS and IDSA recommend a regimen of amoxicillin/clavulanate with a macrolide (azithromycin or clarithromycin) as one of several options for empiric treatment of CAP in adult outpatients with comorbidities (e.g., chronic heart, lung, liver, or renal disease; diabetes mellitus; alcoholism; malignancy; asplenia).305
Skin and Skin Structure Infections
Treatment of skin or skin structure infections (e.g., abscesses, cellulitis, impetigo) caused by β-lactamase-producing S. aureus, Escherichia coli, or Klebsiella.1 2 5 33 42
Urinary Tract Infections (UTIs)
Treatment of UTIs caused by β-lactamase-producing E. coli, Klebsiella, or Enterobacter.1 2 5 14 17 27 28 32 41 43 44 45 47 49 51 53 111
Useful for outpatient treatment of recurrent UTIs or UTIs acquired in hospitals or nursing homes likely to be caused by drug-resistant S. aureus, Enterococcus, or gram-negative bacilli.111 In severe gram-negative infections, consider concomitant use of an aminoglycoside (amikacin, gentamicin, tobramycin).111
Tuberculosis
Has been suggested as an alternative for use in multiple-drug regimens for treatment of active tuberculosis† [off-label] in patients with multidrug-resistant Mycobacterium tuberculosis (MDR-TB),20 31 66
ATS, CDC, IDSA, and others state that amoxicillin/clavulanate is not recommended for inclusion in multiple-drug regimens used for the treatment of MDR-TB because of lack of evidence of clinical benefit.306 However, because of synergistic effects reported between clavulanate and meropenem, these experts state that amoxicillin/clavulanate should be included in multiple-drug regimens whenever a carbapenem is used for the treatment of MDR-TB.306
Bite Wounds
Has been used for empiric treatment of animal or human bites† [off-label].76 109 Active against many likely bite pathogens, including anaerobes, Staphylococcus, Eikenella corrodens, Pasteurella multocida.108 110
Alternative for treatment of infections caused by P. multocida† [off-label] or E. corrodens†.111
Pelvic Inflammatory Disease
Has been used for treatment of acute pelvic inflammatory disease† (PID).46 52
Not included in CDC recommendations for treatment of PID.344
Amoxicillin/Clavulanate Dosage and Administration
Administration
Oral Administration
The various film-coated, scored, and chewable tablets and the oral suspension containing 125, 200, 250, or 400 mg of amoxicillin/5 mL may be administered without regard to meals.1 However, administration with meals results in optimal absorption of clavulanate potassium and may minimize adverse GI effects.1 2 17 37 41 48 53 61
Extended-release tablets containing 1 g of amoxicillin4 and the oral suspension containing 600 mg of amoxicillin/5 mL3 should be administered at the start of a meal to enhance absorption and minimize adverse GI effects.
Chewable tablets should be thoroughly chewed before swallowing.
In adults who have difficulty swallowing tablets, the oral suspension containing 125 or 250 mg of amoxicillin/5 mL may be substituted for 500-mg film-coated tablets or the oral suspension containing 200 or 400 mg of amoxicillin/5 mL may be substituted for 875-mg scored tablets.1
When 500-mg film-coated tablets are indicated, do not substitute 250-mg film-coated tablets and do not substitute chewable tablets.2
When extended-release tablets containing 1 g of amoxicillin are indicated, do not substitute film-coated, scored, or chewable tablets.4
Reconstitution
Reconstitute oral suspension at the time of dispensing.1 3 Tap bottle to thoroughly loosen powder and then add the amount of water specified on the bottle in 2 portions; agitate vigorously after each addition.1 3
Agitate suspension well prior to administration of each dose.1 3
Dosage
Available as fixed combination containing amoxicillin and clavulanate potassium (amoxicillin/clavulanate);1 2 3 4 dosage expressed in terms of amoxicillin.1 2 3 4
Not all preparations of amoxicillin/clavulanate are interchangeable since they contain different amounts of clavulanic acid.1 3
Powders for oral suspension contain a 4:1, 7:1, or 14:1 ratio of amoxicillin to clavulanic acid;1 3 chewable tablets contain a 4:1 or 7:1 ratio of the drugs;1 film-coated tablets contain a 2:1 or 4:1 ratio of the drugs;2 scored tablets contain a 7:1 ratio of the drugs;1 and extended-release tablets contain a 16:1 ratio of the drugs.4
Pediatric Patients
Children weighing <40 kg should not receive film-coated tablets containing 250 mg of amoxicillin since this preparation contains a high dose of clavulanic acid.1
The oral suspension containing 125 mg of amoxicillin/5 mL is the only preparation recommended for use in neonates and infants <12 weeks (3 months) of age.1
Acute Otitis Media (AOM)
AOM in Neonates and Infants <12 Weeks (3 Months) of Age
OralOral suspension: Manufacturer recommends 30 mg/kg daily given in divided doses every 12 hours for 10 days using the oral suspension containing 125 mg/5 mL.1
AOM in Children ≥12 Weeks of Age Weighing <40 kg
OralOral suspension: Manufacturer recommends 45 mg/kg daily given in divided doses every 12 hours for 10 days using the suspension containing 200 or 400 mg/5 mL; alternatively, 40 mg/kg daily given in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1
Chewable tablets: Manufacturer recommends 45 mg/kg daily given in divided doses every 12 hours for 10 days using the chewable tablets containing 200 or 400 mg; alternatively, 40 mg/kg daily given in divided doses every 8 hours using chewable tablets containing 125 or 250 mg.1
AOM in Children Weighing ≥40 kg
OralFilm-coated tablets: Manufacturer recommends one 250-mg tablet every 8 hours or one 500-mg tablet every 12 hours for 10 days.1 2
Oral suspension: Manufacturer recommends 500 mg every 12 hours for 10 days using the suspension containing 125 or 250 mg/5 mL.1
AOM with Severe Illness or When β-Lactamase-producing Strains are Suspected
Oral90 mg/kg daily given in divided doses every 12 hours recommended by AAP and AAFP.115
Usual duration is 10 days; optimal duration is uncertain.115 AAP and AAFP recommend 10 days in those <6 years of age and in those with severe disease and state 5–7 days may be appropriate in those ≥6 years of age with mild to moderate AOM.115
AOM that Failed to Respond to Amoxicillin
Oral90 mg/kg daily given in divided doses every 12 hours recommended by AAP and AAFP.115
Usual duration is 10 days; optimal duration is uncertain.115 AAP and AAFP recommend 10 days in those <6 years of age and in those with severe disease and state 5–7 days may be appropriate in those ≥6 years of age with mild to moderate AOM.115
Persistent or Recurrent AOM
Infections in Children ≥3 Months of Age Weighing <40 kg
OralOral suspension: Manufacturer recommends 90 mg/kg daily given in divided doses every 12 hours for 10 days using the suspension containing 600 mg/5 mL.3
|
Weight (kg) |
Volume of Suspension to Provide 90 mg/kg daily |
|---|---|
|
8 |
3 mL twice daily |
|
12 |
4.5 mL twice daily |
|
16 |
6 mL twice daily |
|
20 |
7.5 mL twice daily |
|
24 |
9 mL twice daily |
|
28 |
10.5 mL twice daily |
|
32 |
12 mL twice daily |
|
36 |
13.5 mL twice daily |
Pharyngitis and Tonsillitis
Oral
40 mg/kg daily (up to 750 mg daily) in 3 divided doses for 10 days for treatment of multiple, recurrent episodes of pharyngitis known to be caused by S. pyogenes†.80
Respiratory Tract Infections
Infections in Neonates and Infants <12 weeks (3 months) of Age
OralOral suspension: 30 mg/kg daily given in divided doses every 12 hours using the suspension containing 125 mg/5 mL.1
Infections in Children ≥12 Weeks of Age Weighing <40 kg
OralOral suspension: 45 mg/kg daily given in divided doses every 12 hours using the suspension containing 200 or 400 mg/5 mL; alternatively, 40 mg/kg daily given in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1
Chewable tablets: 45 mg/kg daily given in divided doses every 12 hours using chewable tablets containing 200 or 400 mg; alternatively, 40 mg/kg daily given in divided doses every 8 hours using chewable tablets containing 125 or 250 mg.1
Infections in Children Weighing ≥40 kg
OralFilm-coated or scored tablets: One 500-mg tablet every 8 hours or one 875-mg tablet every 12 hours.1
Oral suspension: 500 mg every 8 hours using the suspension containing 125 or 250 mg/5 mL1 2 or 875 mg every 12 hours using the suspension containing 200 or 400 mg/5 mL.1 2
Skin and Skin Structure Infections
Infections in Neonates and Infants <12 Weeks (3 Months) of Age
OralOral suspension: 30 mg/kg daily in divided doses every 12 hours using the suspension containing 125 mg/5 mL.1
Infections in Children ≥12 Weeks of Age Weighing <40 kg
OralOral suspension: 25 mg/kg daily in divided doses every 12 hours using the suspension containing 200 or 400 mg/5 mL; alternatively, 20 mg/kg daily in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1 For severe infections, 45 mg/kg daily in divided doses every 12 hours using the suspension containing 200 or 400 mg/5 mL; alternatively, 40 mg/kg daily in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1
Chewable tablets: 25 mg/kg daily in divided doses every 12 hours using chewable tablets containing 200 or 400 mg.1 For severe infections, 45 mg/kg daily given in divided doses every 12 hours using chewable tablets containing 200 or 400 mg.1
Infections in Children Weighing ≥40 kg
OralFilm-coated or scored tablets: One 250-mg tablet every 8 hours or one 500-mg tablet every 12 hours.1 2 For severe infections, one 500-mg tablet every 8 hours or one 875-mg tablet every 12 hours.1
Oral suspension: 500 mg every 12 hours using the suspension containing 125 or 250 mg/5 mL.1
Urinary Tract Infections (UTIs)
Infections in Neonates and Infants <12 Weeks (3 Months) of Age
OralOral suspension: 30 mg/kg daily in divided doses every 12 hours using the suspension containing 125 mg/5 mL.1
Infections in Children ≥12 Weeks of Age Weighing <40 kg
OralOral suspension: 25 mg/kg daily in divided doses every 12 hours using the suspension containing 200 or 400 mg/5 mL; alternatively, 20 mg/kg daily in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1 For severe infections, 45 mg/kg daily in divided doses every 12 hours using the suspension containing 200 or 400 mg/5 mL; alternatively, 40 mg/kg daily in divided doses every 8 hours using the suspension containing 125 or 250 mg/5 mL.1
Chewable tablets: 25 mg/kg daily in divided doses every 12 hours using chewable tablets containing 200 or 400 mg.1 For severe infections, 45 mg/kg daily given in divided doses every 12 hours using chewable tablets containing 200 or 400 mg.1
Infections in Children Weighing ≥40 kg
OralFilm-coated or scored tablets: One 250-mg tablet every 8 hours or one 500-mg tablet every 12 hours.1 2 For severe infections, one 500-mg tablet every 8 hours or one 875-mg tablet every 12 hours.1
Oral suspension: 500 mg every 12 hours using the suspension containing 125 or 250 mg/5 mL.1
Adults
Respiratory Tract Infections
Oral
Scored tablets: one 875-mg-tablet every 12 hours.2
Oral suspension: 875 mg every 12 hours using the suspension containing 200 or 400 mg/5 mL.1
Community-acquired Pneumonia
OralExtended-release tablets: Two 1-g tablets every 12 hours for 7–10 days.4
Sinusitis
OralExtended-release tablets: Two 1-g tablets every 12 hours for 10 days.4
Acute Otitis Media (AOM)
Oral
Film-coated tablets: One 500-mg tablet every 12 hours or one 250-mg tablet every 8 hours.2 For severe infections, one 875-mg tablet every 12 hours or one 500-mg tablet every 8 hours.2
Oral suspension: 500 mg every 12 hours using the suspension containing 125 or 250 mg/5 mL.1 For severe infections, 875 mg every 12 hours using the suspension containing 200 or 400 mg/5 mL.1
Pharyngitis and Tonsillitis
Oral
500 mg twice daily for 10 days for treatment of multiple, recurrent episodes of pharyngitis known to be caused by S. pyogenes†.80 Adult dosage was extrapolated from pediatric dosage and has not been evaluated in clinical studies.80
Skin and Skin Structure Infections
Oral
Film-coated or scored tablets: One 500-mg tablet every 12 hours or one 250-mg tablet every 8 hours.2 For severe infections, one 875 mg-tablet every 12 hours or one 500-mg tablet every 8 hours.2
Oral suspension: 500 mg every 12 hours using the suspension containing 125 or 250 mg/5 mL.1 For severe infections, 875 mg every 12 hours using the suspension containing 200 or 400 mg/5 mL.1
Urinary Tract Infections (UTIs)
Oral
Film-coated or scored tablets: One 500-mg tablet every 12 hours or one 250-mg tablet every 8 hours.2 For severe infections, one 875-mg tablet every 12 hours or one 500-mg tablet every 8 hours.2
Oral suspension: 500 mg every 12 hours using the suspension containing 125 or 250 mg/5 mL.1 For severe infections, 875 mg every 12 hours using the suspension containing 200 or 400 mg/5 mL.1
Special Populations
Hepatic Impairment
Select dosage with caution and monitor hepatic function.1 2 3 4 (See Hepatic Effects under Cautions.)
Renal Impairment
Dosage adjustment necessary in patients with moderate to severe renal impairment.2 5 17 63 65
Do not use scored tablets containing 875 mg of amoxicillin in those with severe renal impairment and GFR <30 mL/minute.2
Do not use extended-release tablets containing 1 g of amoxicillin in those with Clcr <30 mL/minute or in hemodialysis patients.4
|
GFR (mL/min) |
Daily Dosage |
|---|---|
|
10–30 |
250 or 500 mg every 12 hours depending on infection severity |
|
<10 |
250 or 500 mg every 24 hours depending on infection severity |
|
Hemodialysis Patients |
250 or 500 mg every 24 hours depending on infection severity; with an additional dose both during and at the end of dialysis |
Geriatric Patients
No dosage adjustments except those related to renal impairment.4 (See Renal Impairment under Dosage and Administration.)
Cautions for Amoxicillin/Clavulanate
Contraindications
-
Previous history of cholestatic jaundice or hepatic dysfunction associated with amoxicillin/clavulanate.1 2 3 4
-
Use of extended-release tablets containing 1 g of amoxicillin in those with Clcr <30 mL/minute or in hemodialysis patients.4
Warnings/Precautions
Warnings
Superinfection/Clostridioides difficile-associated Colitis
Possible emergence and overgrowth of nonsusceptible bacteria or fungi.1 2 3 4 Discontinue and institute appropriate therapy if superinfection occurs.1 2 3 4
Treatment with anti-infectives alters normal colon flora and may permit overgrowth of C. difficile.1 2 3 4 302 C. difficile infection (CDI) and C. difficile-associated diarrhea and colitis (CDAD; also known as antibiotic-associated diarrhea and colitis or pseudomembranous colitis) reported with nearly all anti-infectives, including amoxicillin/clavulanate, and may range in severity from mild diarrhea to fatal colitis.1 2 3 4 302 Consider CDAD if diarrhea develops during or after therapy and manage accordingly.1 2 3 4 302
If CDAD suspected or confirmed, discontinue anti-infectives not directed against C. difficile as soon as possible.1 2 3 4 302 Initiate appropriate anti-infective therapy directed against C. difficile (e.g., fidaxomicin, vancomycin, metronidazole), appropriate supportive therapy (e.g., fluid and electrolyte management, protein supplementation), and surgical evaluation as clinically indicated.1 2 3 4 302
Hepatic Effects
Rare reports of hepatic dysfunction (e.g., increases in serum AST, ALT, bilirubin, and/or alkaline phosphatase), especially in geriatric patients, males, or with prolonged therapy.1 2 3 4
Hepatic dysfunction may occur during or several weeks following discontinuance of therapy.1 2 3 4
Hepatic dysfunction may be severe, but usually is reversible.1 2 3 4 Histologic findings indicate predominantly cholestatic, hepatocellular, or mixed cholestatic-hepatocellular changes.1 2 3 4
Fatalities has been reported rarely,1 2 3 4 71 most frequently in those with serious underlying diseases or concomitant drug therapy.1 2 3 4
Assess hepatic function periodically during prolonged therapy.1 2 3 4
Use with caution if there is evidence of hepatic dysfunction.1 2 3 4
Sensitivity Reactions
Hypersensitivity Reactions
Serious and occasionally fatal hypersensitivity reactions reported with penicillins.1 2 3 4
Prior to initiation of therapy, make careful inquiry regarding previous hypersensitivity reactions to penicillins, cephalosporins, or other drugs.1 2 3 4 Partial cross-allergenicity occurs among penicillins and other β-lactam antibiotics including cephalosporins and cephamycins.1 2 3 4
If hypersensitivity reaction occurs, discontinue immediately and institute appropriate therapy as indicated (e.g., epinephrine, corticosteroids, maintenance of an adequate airway and oxygen).1 2 3 4
General Precautions
Renal Effects
Acute interstitial nephritis and hematuria reported rarely.1 2 3 4
Assess renal function periodically during prolonged therapy.1 2 3 4
Hematologic Effects
Adverse hematologic effects (e.g., anemia, hemolytic anemia, leukopenia, agranulocytosis, thrombocytopenia, thrombocytopenic purpura) reported with penicillins.1 2 3 4 Usually reversible when drug discontinued; may be a hypersensitivity reaction.1 2 3 4
Assess hematologic function periodically during prolonged therapy.1 2 3 4
Mononucleosis
Possible increased risk of erythematous rash in patients with mononucleosis; use in these patients not recommended.1 2 3 4 22 23
Phenylketonuria
Chewable tablets containing 200 or 400 mg of amoxicillin contain aspartame (NutraSweet), which is metabolized in the GI tract to provide 2.1 or 4.2 mg of phenylalanine, respectively.1
Oral suspensions containing 200 400, or 600 mg of amoxicillin/5 mL contain aspartame (NutraSweet), which is metabolized in the GI tract to provide 7 mg of phenylalanine/5 mL.1 3
Other commercially available preparations do not contain aspartame;1 2 4 these other preparations should be used in individuals with phenylketonuria (i.e., homozygous genetic deficiency of phenylalanine hydroxylase) and other individuals who must restrict their intake of phenylalanine.1
Potassium and Sodium Content
Chewable tablets containing 125 or 250 mg of amoxicillin contain 0.16 or 0.32 mEq of potassium, respectively; chewable tablets containing 200 or 400 mg of amoxicillin contain 0.14 or 0.29 mEq of potassium, respectively.1
Each 5 mL of oral suspension containing 125 or 250 mg of amoxicillin contains 0.16 or 0.32 mEq of potassium, respectively.1 Each 5 mL of oral suspension containing 200 or 400 mg of amoxicillin contains 0.14 or 0.29 mEq of potassium, respectively.1 Each 5 mL of oral suspension containing 600 mg of amoxicillin contains 0.23 mEq of potassium.3
Each film-coated or conventional tablet containing 250, 500, or 875 mg of amoxicillin contains 0.63 mEq of potassium.2
Each extended-release tablet containing 1 g of amoxicillin contains 12.6 mg (0.32 mEq) of potassium and 29.3 (1.27 mEq) of sodium.4
Selection and Use of Anti-infectives
To reduce development of drug-resistant bacteria and maintain effectiveness of amoxicillin/clavulanate and other antibacterials, use only for treatment or prevention of infections proven or strongly suspected to be caused by susceptible bacteria.1 2 3 4
When selecting or modifying anti-infective therapy, use results of culture and in vitro susceptibility testing.1 2 3 4 In the absence of such data, consider local epidemiology and susceptibility patterns when selecting anti-infectives for empiric therapy.1 2 3 4
Use of Fixed Combinations
Consider cautions, precautions, contraindications, and drug interactions associated with both drugs in the fixed combination.
When prescribing, preparing, and dispensing amoxicillin/clavulanate, consider that dosage of the fixed combination usually is expressed as the amoxicillin component.1 2 3 4
Specific Populations
Pregnancy
Lactation
Distributed into milk; use with caution.1 2 3 4
Pediatric Use
Renal clearance of amoxicillin may be delayed in neonates and young infants because of incompletely developed renal function.1 Dosage adjustments necessary in those <12 weeks (3 months) of age compared with older infants and children.1 (See Pediatric Patients under Dosage and Administration.)
Adverse effects profile similar to adults.1 In children 2 months to 12 years of age receiving oral suspension, diarrhea occurs less frequently with dosing every 12 hours compared with every 8 hours.1
Safety and efficacy of oral suspension containing 600 mg of amoxicillin/5 mL not established in children <3 months of age.3
Safety and efficacy of extended-release tablets containing 1 g of amoxicillin not established in children <16 years of age.4
Geriatric Use
Possible increased incidence of hepatic dysfunction compared with younger adults.1 2 3 4 (See Hepatic Effects under Cautions.)
Studies using extended-release tablets containing 1 g of amoxicillin indicate no substantial differences in safety and efficacy relative to younger adults, but increased sensitivity cannot be ruled out.4
Substantially eliminated by kidneys.4 Monitor renal function since geriatric patients more likely to have decreased renal function.17 63 65
Consider that extended-release tablets containing 1 g of amoxicillin contain 29.3 mg (1.27 mEq) of sodium.4
Hepatic Impairment
Use with caution;1 2 3 4 assess hepatic function periodically during prolonged therapy.1 2 3 4
Renal Impairment
Substantially eliminated by kidneys; risk of dose-dependent adverse effects may be greater in those with impaired renal function.17 63 65
Evaluate renal function periodically during prolonged therapy.1 2 3 4
Dosage adjustments necessary in moderate or severe renal impairment.2 5 17 63 65
Tablets containing 875 mg of amoxicillin should not be used in those with severe renal impairment (GFR <30 mL/minute).2
Pharmacokinetics of extended-release tablets not evaluated in renal impairment;4 extended-release tablets contraindicated in those with Clcr <30 mL/minute and in hemodialysis patients.4
Common Adverse Effects
Adverse GI effects (e.g., diarrhea or loose stools,1 2 3 4 17 27 32 33 41 42 44 49 nausea,1 2 3 4 27 32 42 53 vomiting),1 2 3 4 27 32 42 53 hypersensitivity reactions (e.g., rash,1 2 3 4 46 urticaria).1 2 3 4
Adverse GI effects may be more frequent with amoxicillin/clavulanate than with amoxicillin alone.5 Severe diarrhea may occur less frequently in adults if 875 mg given every 12 hours rather than 500 mg every 8 hours.1
Drug Interactions
Specific Drugs and Laboratory Tests
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Allopurinol |
Possible increased incidence of rash;1 2 3 4 reported with ampicillin but no data regarding amoxicillin1 2 3 4 113 114 |
Unclear whether potentiation of rash is caused by allopurinol or hyperuricemia present in these patients1 2 3 4 113 114 |
|
Antacids |
No effect on pharmacokinetics of amoxicillin or clavulanate when antacids administered simultaneously with or 2 hours after extended-release tablets containing amoxicillin and clavulanate potassium4 |
|
|
Hormonal contraceptives |
||
|
Probenecid |
Decreased renal tubular secretion of amoxicillin and increased and prolonged amoxicillin plasma concentrations.1 2 3 4 56 |
|
|
Tests for glucose |
Possible false-positive reactions in urine glucose tests using Clinitest, Benedict’s solution, or Fehling’s solution;1 2 3 4 reported with ampicillin but no data regarding amoxicillin1 2 3 4 |
Use glucose tests based on enzymatic glucose oxidase reactions (e.g., Clinistix, Tes-Tape)1 2 3 4 |
Amoxicillin/Clavulanate Pharmacokinetics
Absorption
Bioavailability
Both amoxicillin and clavulanate potassium well absorbed following oral administration.1 2 3 4 5 30 41 53 62 62
Amoxicillin plasma concentrations attained with amoxicillin/clavulanate are similar to those attained with equivalent doses of amoxicillin alone.1 2 3 4 5 61 62
A single chewable tablet containing 250 mg of amoxicillin and 62.5 mg of clavulanate potassium or 2 chewable tablets containing 125 mg of amoxicillin and 31.25 mg of clavulanate potassium are bioequivalent to 5 mL of the oral suspension containing 250 mg of amoxicillin/5 mL.1
A single chewable tablet containing 400 mg of amoxicillin and 57 mg of clavulanate potassium is bioequivalent to 5 mL of the oral suspension containing 400 mg of amoxicillin/5 mL.1
Food
Food has minimal or no effect on bioavailability of oral amoxicillin;1 2 3 4 5 6 48 61 62 bioavailability of clavulanate may be increased when taken with food.1 2 3 4
Optimal absorption of both amoxicillin and clavulanic acid occurs when extended-release tablets containing 1 g of amoxicillin are taken at the start of a standardized meal.4 With this preparation, absorption of amoxicillin is decreased in the fasted state and absorption of clavulanate is decreased when taken with a high-fat meal.4
Distribution
Extent
Amoxicillin readily distributed into most tissues and fluids following oral administration,1 2 3 4 including lungs,5 17 bronchial secretions72 maxillary sinus secretions,7 bile,5 pleural fluid,5 17 53 peritoneal fluid,41 53 55 sputum,5 and middle ear fluid.1 3
Animal studies indicate clavulanic acid well distributed into body tissues.1 2 3 4 5
Only low amoxicillin concentrations attained in CSF.5 17 41 53
Both amoxicillin and clavulanate potassium cross the placenta.5 7 19 53
Both amoxicillin1 2 3 4 5 21 and clavulanate potassium distribute into human milk.5 7 21 53
Plasma Protein Binding
Amoxicillin: 17–20%.1 2 3 4 5 6
Clavulanic acid: 22–30%.1 2 3 4 41
Elimination
Metabolism
Amoxicillin probably metabolized to some extent in the liver.5
Clavulanic acid may be extensively metabolized.5 17 40 62
Elimination Route
Amoxicillin eliminated principally in urine1 2 3 4 5 by both glomerular filtration and tubular secretion;5 clavulanate eliminated by renal and nonrenal routes.4 5 62
Approximately 50–80% of amoxicillin1 2 3 4 5 and 25–50% of clavulanic acid dose excreted unchanged in urine.1 2 3 4
Half-life
Amoxicillin: 1–1.4 hours.1 2 3 4 39 41 57
Clavulanic acid: 0.78–1.2 hours.1 2 3 4 17 39 41 50 57 62
Special Populations
Serum concentrations and half-life of amoxicillin increased in patients with renal impairment.5 6 17 63 65 Half-life of clavulanic acid increased slightly in patients with renal impairment.5
Renal clearance may be delayed in neonates and young infants because of incompletely developed renal function.1
Stability
Storage
Oral
For Suspension
≤25°C.1 3 Following reconstitution, refrigerate and discard after 10 days.1 3
Tablets
Scored, film-coated, chewable, or extended-release tablets: ≤25°C.1 2 4
Actions and Spectrum
-
Amoxicillin/clavulanate is a fixed combination of amoxicillin trihydrate (a β-lactam antibacterial classified as an aminopenicillin) and the potassium salt of clavulanic acid (a β-lactamase inhibitor).17 35 41 61
-
Clavulanic acid synergistically expands activity of amoxicillin against β-lactamase-producing bacteria1 5 8 10 11 12 13 15 16 17 25 34 35 37 41 46 53 58 60 61 by irreversibly and competitively inhibiting β-lactamases.5 8 10 16 17 34 35 37 54 60 70
-
Active against bacteria susceptible to amoxicillin alone and also active against many β-lactamase-producing bacteria resistant to amoxicillin alone.5 11 13 17 25 29 35 38 41 53 54 60 61
-
Gram-positive aerobes: Active in vitro and in clinical infections against Staphylococcus (including β-lactamase-producing strains),1 4 5 17 35 37 42 108 Streptococcus pneumoniae,1 4 17 35 S. pyogenes (group A β-hemolytic streptococci),5 and Enterococcus faecalis.5
-
Gram-negative aerobes: Active in vitro and in clinical infections against β-lactamase-producing strains of Haemophilus influenzae,4 5 13 17 1 35 38 H. parainfluenzae,4 Klebsiella pneumoniae,1 4 5 Moraxella catarrhalis,4 17 35 59 108 and Escherichia coli.15 17 28 1 29 35 Also active in vitro against Eikenella corrodens108 and Pasteurella multocida.108 110
-
Active in vitro and in clinical infections against Mycobacteria tuberculosis, including multidrug-resistant strains.24 26 31 66 Active in vitro against some anaerobic bacteria, including Peptostreptococcus,1 4 108 Bacteroides,1 4 10 15 17 25 35 Fusobacterium,1 4 108 and Prevotella.108
-
Resistance reported in some gram-negative bacteria (e.g., Citrobacter freundii, Enterobacter cloacae, Serratia marcescens, Pseudomonas aeruginosa, some strains of E. coli).5 17 35 37 41 42 49 53
Advice to Patients
-
Advise patients that antibacterials (including amoxicillin/clavulanate) should only be used to treat bacterial infections and not used to treat viral infections (e.g., the common cold).1 2 3 4
-
Importance of taking each dose with a meal or snack to decrease the risk of adverse GI effects.1 2 3 4
-
Importance of contacting clinician if diarrhea occurs that is severe or lasts longer than 2 or 3 days.1 2 3 4
-
Importance of completing the entire prescribed course of treatment, even if feeling better after a few days.1 2 3 4
-
Advise patients that skipping doses or not completing the full course of therapy may decrease effectiveness and increase the likelihood that bacteria will develop resistance and will not be treatable with amoxicillin/clavulanate or other antibacterials in the future.1 2 3 4
-
Importance of keeping oral suspension refrigerated; shaking the suspension well prior to withdrawal of each dose; using a dosing spoon or medicine dropper and rinsing it well after each use; and discarding any unused suspension.1 3
-
Advise individuals with phenylketonuria and other individuals who must restrict their intake of phenylalanine that 200- and 400-mg chewable tablets and oral suspensions containing 200, 400, or 600 mg of amoxicillin/5 mL contain aspartame (NutraSweet), which is metabolized in the GI tract to phenylalanine.1 3
-
Importance of informing clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs.1 2 3 4
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 2 3 4
-
Importance of advising patients of other important precautionary information.1 2 3 4 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
For suspension |
125 mg (of amoxicillin) per 5 mL and 31.25 mg (of clavulanic acid) per 5 mL* |
Amoxicillin and Clavulanate Potassium for Oral Suspension |
|
|
Augmentin |
GlaxoSmithKline |
|||
|
200 mg (of amoxicillin) per 5 mL and 28.5 mg (of clavulanic acid) per 5 mL* |
Amoxicillin and Clavulanate Potassium for Oral Suspension |
|||
|
250 mg (of amoxicillin) per 5 mL and 62.5 mg (of clavulanic acid) per 5 mL |
Amoxicillin and Clavulanate Potassium for Oral Suspension |
|||
|
Augmentin |
||||
|
400 mg (of amoxicillin) per 5 mL and 57 mg (of clavulanic acid) per 5 mL* |
Amoxicillin and Clavulanate Potassium for Oral Suspension |
|||
|
600 mg (of amoxicillin) per 5 mL and 42.9 mg (of clavulanic acid) per 5 mL* |
Amoxicillin and Clavulanate Potassium for Oral Suspension |
|||
|
Augmentin ES-600 |
||||
|
Tablets, chewable |
200 mg (of amoxicillin) and 28.5 mg (of clavulanic acid)* |
Amoxicillin and Clavulanate Potassium Chewable Tablets |
||
|
400 mg (of amoxicillin) and 57 mg (of clavulanic acid) |
Amoxicillin and Clavulanate Potassium Chewable Tablets |
|||
|
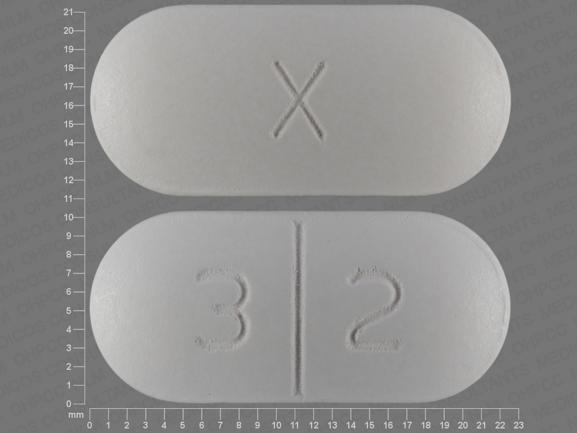
Tablets, film-coated |
250 mg (of amoxicillin) and 125 mg (of clavulanic acid)* |
Amoxicillin and Clavulanate Potassium Tablets |
||
|
500 mg (of amoxicillin) and 125 mg (of clavulanic acid)* |
Amoxicillin and Clavulanate Potassium Tablets |
|||
|
875 mg (of amoxicillin) and 125 mg (of clavulanic acid)* |
Amoxicillin and Clavulanate Potassium Tablets |
|||
|
Augmentin |
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, extended-release |
1 g (of amoxicillin) and 62.5 mg (of clavulanic acid) |
Amoxicillin and Clavulanate Potassium Extended-release Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions February 2, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. GlaxoSmithKline. Augmentin (amoxicillin/clavulanate potassium) powder for oral suspension and chewable tablets prescribing information. Research Triangle Park, NC; 2004 Jun.
2. GlaxoSmithKline. Augmentin (amoxicillin/clavulanate potassium) tablets prescribing information. Research Triangle Park, NC; 2004 Jun.
3. GlaxoSmithKline. Augmentin ES-600 (amoxicillin/clavulanate potassium) powder for oral suspension prescribing information. Research Triangle Park, NC; 2004 Jun.
4. GlaxoSmithKline. Augmentin XR (amoxicillin/clavulanate potassium) extended release tablets prescribing information. Research Triangle Park, NC; 2004 Jun.
5. Kucers A, Crowe S, Grayson ML et al, eds. The use of antibiotics. A clinical review of antibacterial, antifungal, and antiviral drugs. 5th ed. Jordan Hill, Oxford: Butterworth-Heinemann; 1997: 134-44,192-208.
6. Chambers HF. Penicillins. In: Mandell GL, Bennett JE, Dolin R, eds. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 5th ed. New York: Churchill Livingstone; 2000: 261-74.
7. Brogden RN, Speight TM, Avery GS. Amoxycillin: a review of its antibacterial and pharmacokinetic properties and therapeutic use. Drugs. 1975; 9:88-140. https://pubmed.ncbi.nlm.nih.gov/1126306
8. Wise R. β-Lactamase inhibitors. J Antimicrob Chemother. 1982; 9(Suppl B):31-40. https://pubmed.ncbi.nlm.nih.gov/6977527
10. Wise R, Andrews JM, Bedford KA. In vitro study of clavulanic acid in combination with penicillin, amoxycillin, and carbenicillin. Antimicrob Agents Chemother. 1978; 13:389-93. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC352250/ https://pubmed.ncbi.nlm.nih.gov/122520
11. Hunter PA, Coleman K, Fisher J et al. In vitro synergistic properties of clavulanic acid, with ampicillin, amoxycillin and ticarcillin. J Antimicrob Chemother. 1980; 6:455-70. https://pubmed.ncbi.nlm.nih.gov/6968746
12. Spratt BG, Jobanputra V, Zimmermann W. Binding of thienamycin and clavulanic acid to the penicillin-binding proteins of Escherichia coli K-12. Antimicrob Agents Chemother. 1977; 12:406-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC429926/ https://pubmed.ncbi.nlm.nih.gov/334066
13. Girouard YC, Maclean IW, Ronald AR et al. Synergistic antibacterial activity of clavulanic acid and amoxicillin against β-lactamase-producing strains of Haemophilus ducreyi. Antimicrob Agents Chemother. 1981; 20:144-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC181647/ https://pubmed.ncbi.nlm.nih.gov/6974538
14. Crokaert F, Van der Linden MP, Yourassowsky E. Activities of amoxicillin and clavulanic acid combinations against urinary tract infections. Antimicrob Agents Chemother. 1982; 22:346-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC183740/ https://pubmed.ncbi.nlm.nih.gov/6765418
15. Matsuura M, Nakazawa H, Hashimoto T et al. Combined antibacterial activity of amoxicillin with clavulanic acid against ampicillin-resistant strains. Antimicrob Agents Chemother. 1980; 17:908-11. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC283901/ https://pubmed.ncbi.nlm.nih.gov/6967713
16. Reading C, Cole M. Clavulanic acid: a beta-lactamase-inhibiting beta lactam from Streptomyces clavuligerus. Antimicrob Agents Chemother. 1977; 11:852-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC352086/ https://pubmed.ncbi.nlm.nih.gov/879738
17. Brogden RN, Carmine A, Heel RC et al. Amoxycillin/clavulanic acid: a review of its antibacterial activity, pharmacokinetics and therapeutic use. Drugs. 1981; 22:337-62. https://pubmed.ncbi.nlm.nih.gov/7037354
19. Buckingham M, Welply G, Miller JF et al. Gastro-intestinal absorption and transplacental transfer of amoxycillin during labour and the influence of metoclopramide. Curr Med Res Opin. 1975; 3:342-6.
20. Centers for Disease Control and Prevention. Treatment of tuberculosis, American Thoracic Society, CDC, and Infectious Diseases Society of America. MMWR Morb Mortal Wkly Rep. 2003; 52(No. RR-11):1-77. https://www.cdc.gov/mmwr/PDF/rr/rr5211.pdf https://pubmed.ncbi.nlm.nih.gov/12549898
21. Kafetzis DA, Siafas CA, Georgakopoulos PA et al. Passage of cephalosporins and amoxicillin into the breast milk. Acta Paediatr Scand. 1981; 70:285-8. https://pubmed.ncbi.nlm.nih.gov/7246123
22. Almeyda J, Levantine A. Drug reactions XIX: adverse cutaneous reactions to the penicillins—ampicillin rashes. Br J Dermatol. 1972; 87:293-6. https://pubmed.ncbi.nlm.nih.gov/4342950
23. Mulroy R. Amoxycillin rash in infectious mononucleosis. Br Med J. 1973; 1:554. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1588712/ https://pubmed.ncbi.nlm.nih.gov/4266345
24. Cynamon MH, Palmer GS. In vitro activity of amoxicillin in combination with clavulanic acid against Mycobacterium tuberculosis. Antimicrob Agents Chemother. 1983; 24:429-31. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185338/ https://pubmed.ncbi.nlm.nih.gov/6416162
25. Lomothe F, Auger F, Lacroix J-M. Effect of clavulanic acid on the activities of ten β-lactam agents against members of the Bacteroides fragilis group. Antimicrob Agents Chemother. 1984; 25:662-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185612/ https://pubmed.ncbi.nlm.nih.gov/6732233
26. Abate G, Miorner H. Susceptibility of multidrug-resistant strains of Mycobacterium tuberculosis to amoxycillin in combination with clavulanic acid and ethambutol. J Antimicrob Chemother. 1998; 42:735-40. https://pubmed.ncbi.nlm.nih.gov/10052896
27. Iravani A, Richard GA. Treatment of urinary tract infections with a combination of amoxicillin and clavulanic acid. Antimicrob Agents Chemother. 1982; 22:672-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC183812/ https://pubmed.ncbi.nlm.nih.gov/7181477
28. Martinelli R, Lopes AA, De Oliveira MM et al. Amoxicillin-clavulanic acid in treatment of urinary tract infections due to gram-negative bacteria resistant to penicillin. Antimicrob Agents Chemother. 1981; 20:800-2. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC181801/ https://pubmed.ncbi.nlm.nih.gov/7034642
29. Perryman F, Johnson S, Hussain Qadri SM. In vitro activity of augmentin against pathogenic bacteria and its comparison with other antibiotics. Chemotherapy. 1983; 29:111-5. https://pubmed.ncbi.nlm.nih.gov/6839863
30. Adam D, Visser ID, Koeppe P. Pharmacokinetics of amoxicillin and clavulanic acid administered alone and in combination. Antimicrob Agents Chemother. 1982; 22:353-7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC183747/ https://pubmed.ncbi.nlm.nih.gov/7137979
31. Nadler JP, Berger J, Nord JA et al. Amoxicillin-clavulanic acid for treating drug-resistant Mycobacterium tuberculosis. 1991; 99:1025-6.
32. Brumfitt W, Hamilton-Miller JM. Amoxicillin plus clavulanic acid in the treatment of recurrent urinary tract infections. Antimicrob Agents Chemother. 1984; 25:276-8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185489/ https://pubmed.ncbi.nlm.nih.gov/6561953
33. Fleisher GR, Wilmott CM, Campos JM. Amoxicillin combined with clavulanic acid for the treatment of soft tissue infections in children. Antimicrob Agents Chemother. 1983; 24:679-81. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185924/ https://pubmed.ncbi.nlm.nih.gov/6660847
34. Labia R, Peduzzi J. Augmentin and β-lactamases: inactivation of β-lactamases by clavulanic acid. In: Croydon EA, Michel MF, eds. Augmentin: Proceedings of the European symposium Scheveningen, The Netherlands 28–29 June, 1982. Amsterdam: Elsevier; 1983:11-20.
35. White AR, Boon RJ, Masters PJ et al. Antibacterial activity of amoxycillin/clavulanic acid (Augmentin) in vitro. In: Croydon EA, Michel MF, eds. Augmentin: Proceedings of the European symposium Scheveningen, The Netherlands 28–29 June, 1982. Amsterdam: Elsevier; 1983:21-41.
37. Neu HC, Fu KP. Clavulanic acid, a novel inhibitor of β-lactamases. Antimicrob Agents Chemother. 1978; 14:650-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC352529/ https://pubmed.ncbi.nlm.nih.gov/310279
38. Yogev R, Melick C, Kabat WJ. In vitro and in vivo synergism between amoxicillin and clavulanic acid against ampicillin-resistant Haemophilus influenzae type b. Antimicrob Agents Chemother. 1981; 19:993-6. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC181597/ https://pubmed.ncbi.nlm.nih.gov/6973952
39. Hoffken G, Witkowski G, Lode H et al. Comparative pharmacokinetics of amoxycillin, clavulanic acid and their combination. In: Croydon EA, Michel MF, eds. Augmentin: Proceedings of the European symposium Scheveningen, The Netherlands 28–29 June, 1982. Amsterdam: Elsevier; 1983:102-8.
40. Haginaka J, Nakagawa T, Hoshino T et al. Pharmacokinetic studies of the urinary excretion of clavulanic acid in man. Chem Pharm Bull. 1981; 29:3342-9. https://pubmed.ncbi.nlm.nih.gov/7337933
41. Stein GE, Gurwith MJ. Amoxicillin-potassium clavulanate, a β-lactamase-resistant antibiotic combination. Clin Pharm. 1984; 3:591-9. https://pubmed.ncbi.nlm.nih.gov/6391783
42. Pien FD. Double-blind comparative study of two dosage regimens of cefaclor and amoxicillin-clavulanic acid in the outpatient treatment of soft tissue infections. Antimicrob Agents Chemother. 1983; 24:856-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185396/ https://pubmed.ncbi.nlm.nih.gov/6362559
43. Fancort GJ, Flavell Matts SG, Mitchell CJ. Augmentin (amoxycillin-clavulanic acid) compared with co-trimoxazole in urinary tract infections. BMJ. 1984; 289:82-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1441926/ https://pubmed.ncbi.nlm.nih.gov/6428687
44. Stein GE, Patterson MJ, Gurwith D et al. Amoxycillin/clavulanic acid therapy of acute urinary tract infection. Curr Ther Res Clin Exp. 1982; 32:617-23.
45. Greenwood D, Slack R. Urinary tract infection. Br J Clin Pharmacol. 1982; 13:619-30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1402097/ https://pubmed.ncbi.nlm.nih.gov/7044399
46. Ball P, Watson T, Mehtar S. Amoxycillin and clavulanic acid in intra-abdominal and pelvic sepsis. J Antimicrob Chemother. 1981; 7:441-4. https://pubmed.ncbi.nlm.nih.gov/7251526
47. Hart CA, Desmond AD, Percival A. Treatment of gentamicin-resistant Klebsiella urinary tract infections with cephradine, augmentin, cefuroxime and amikacin. J Antimicrob Chemother. 1981; 8:231-7. https://pubmed.ncbi.nlm.nih.gov/6912860
48. Staniforth DH, Lillystone RJ, Jackson D. Effect of food on the bioavailability and tolerance of clavulanic acid/amoxycillin combination. J Antimicrob Chemother. 1982; 10:131-9. https://pubmed.ncbi.nlm.nih.gov/7118763
49. Al Roomi LG, Sutton AM, Cockburn F et al. Amoxycillin and clavulanic acid in the treatment of urinary infection. Arch Dis Child. 1984; 59:256-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1628547/ https://pubmed.ncbi.nlm.nih.gov/6712275
50. Daigneault EA, Aten E, Roseman JM. Pharmacokinetics and urinary excretion of clavulanic acid after oral administration of amoxicillin and clavulanic acid (Augmentin). J Clin Pharmacol. 1984; 24:402.
51. Gurwith MJ, Stein GE, Gurwith D. Prospective comparison of amoxicillin-clavulanic acid and cefaclor in treatment of uncomplicated urinary tract infections. Antimicrob Agents Chemother. 1983; 24:716-9. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC185931/ https://pubmed.ncbi.nlm.nih.gov/6362553
52. Uri FI, Sartawi SA, Dajani YF et al. Amoxycillin/clavulanic acid (augmentin) compared with triple drug therapy for pelvic inflammatory disease. Int J Gynaecol Obstet. 1992; 38:41-3. https://pubmed.ncbi.nlm.nih.gov/1348989
53. Weber DJ, Tolkoff-Rubin NE, Rubin RH. Amoxicillin and potassium clavulanate: an antibiotic combination: mechanisms of action, pharmacokinetics, antimicrobial spectrum, clinical efficacy and adverse effects. Pharmacotherapy. 1984; 4:122-36. https://pubmed.ncbi.nlm.nih.gov/6739312
54. Reading C, Farmer T, Cole M. The β-lactamase stability of amoxycillin with the β-lactamase inhibitor, clavulanic acid. J Antimicrob Chemother. 1983; 11:27-32. https://pubmed.ncbi.nlm.nih.gov/6600741
55. Wise R, Donovan IA, Drumm J et al. The penetration of amoxycillin/clavulanic acid into peritoneal fluid. J Antimicrob Chemother. 1983; 11:57-60. https://pubmed.ncbi.nlm.nih.gov/6826486
56. Staniforth DH, Jackson D, Clarke HL et al. Amoxycillin/clavulanic acid: the effect of probenecid. J Antimicrob Chemother. 1983; 12:272-5.
57. Wise R, Bennett SA, Dent J. The pharmacokinetics of orally absorbed cefuroxime compared with amoxycillin/clavulanic acid. J Antimicrob Chemother. 1984; 13:603-10. https://pubmed.ncbi.nlm.nih.gov/6469882
58. Semenitz E, Casey PA, Pfaller W et al. Microcalorimetric, turbidimetric, phase-contrast microscopic, and electron microscopic investigations of the actions of amoxicillin, clavulanic acid and Augmentin on amoxicillin-sensitive and amoxicillin-resistant strains of Escherichia coli. Chemotherapy. 1983; 29:192-207. https://pubmed.ncbi.nlm.nih.gov/6347546
59. Ninane G, Joly J, Kraytman M et al. Bronchopulmonary infection due to β-lactamase-producing Branhamella catarrhalis treated with amoxycillin/clavulanic-acid. Lancet. 1978; 2:257. https://pubmed.ncbi.nlm.nih.gov/79045
60. Reading C. The biochemistry and mode of action of Augmentin. In: Leigh DA, Robinson OPW, eds. Augmentin clavulanate-potentiated amoxycillin: Proceedings of the second symposium 17 July, 1981. Amsterdam: Elsevier; 1982:5-21.
61. Grayson ML, ed. Kucers' the use of antibiotics: a clinical review of antibacterial, antifungal, antiparasitic, and antiviral drugs. 7th ed. Boca Raton, FL: CRC Press; 2018:.
62. Jackson D, Cooper DL, Horton R et al. Absorption, pharmacokinetic and metabolic studies with Augmentin. In: Croydon EA, Michel MF, eds. Augmentin: Proceedings of the European symposium Scheveningen, The Netherlands 28–29 June, 1982. Amsterdam: Elsevier; 1983:83-101.
63. Dalet F, Cabrera E, Donate T et al. Pharmacokinetics of the association amoxycillin and clavulanic acid in renal insufficiency and during haemodialysis. In: Croydon EA, Michel MF, eds. Augmentin: Proceedings of the European symposium Scheveningen, The Netherlands 28–29 June, 1982. Amsterdam: Elsevier; 1983:109-20.
65. Slaughter RL, Kohli R, Brass C. Effects of hemodialysis on the pharmacokinetics of amoxicillin/clavulanic acid combination. Ther Drug Monit. 1984; 6:424-7. https://pubmed.ncbi.nlm.nih.gov/6393464
66. Chambers HF, Kocagoz T, Sipit T et al. Activity of amoxicillin/clavulanate in patients with tuberculosis. Clin Infect Dis. 1998; 26:8748-9.
67. Marchant CD, Shurin PA, Johnson CE et al. A randomized controlled trial of amoxicillin plus clavulanate compared with cefaclor for treatment of acute otitis media. J Pediatr. 1986; 109:891-6. https://pubmed.ncbi.nlm.nih.gov/3534203
68. Odio CM, Kusmiesz H, Shelton S et al. Comparative treatment trial of augmentin versus cefaclor for acute otitis media with effusion. Pediatrics. 1985; 75:819-26. https://pubmed.ncbi.nlm.nih.gov/4039433
69. Wallace RJ Jr, Steele LC, Brooks DL et al. Amoxicillin-clavulanic acid in the treatment of lower respiratory tract infections caused by β-lactamase-positive Haemophilus influenzae and Branhamella catarrhalis. Antimicrob Agents Chemother. 1985; 27:912-5. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC180185/ https://pubmed.ncbi.nlm.nih.gov/3875310
70. Neu HC. Contribution of beta-lactamases to bacterial resistance and mechanisms to inhibit beta-lactamases. Am J Med. 1985; 79(Suppl 5B):2-12.
71. Hebbard GS, Smith KGC, Gibson PR et al. Augmentin-induced jaundice with a fatal outcome. Med J Aust. 1992; 156:285-6. https://pubmed.ncbi.nlm.nih.gov/1738330
72. Bergogne-Berezin E, Morel C, Benard Y et al. Pharmacokinetic study of β-lactam antibiotics in bronchial secretions. Scand J Infect Dis. 1978; 14(Suppl):267-72.
74. Anon. Drugs for treatment of acute otitis media in children. Med Lett Drug Ther. 1994; 36:19-21.
75. Dajani A, Taubert K, Ferrieri P et al and the Committee on Rheumatic Fever et al. Treatment of acute streptococcal pharyngitis and prevention of rheumatic fever: a statement for health professionals. Pediatrics. 1995; 96:758-64. https://pubmed.ncbi.nlm.nih.gov/7567345
76. Committee on Infectious Diseases, American Academy of Pediatrics. Red book: 2003 report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village, IL: American Academy of Pediatrics; 2003:495, 578-80.
77. Klein JO. Selection of oral antimicrobial agents for otitis media and pharyngitis. Infect Dis Clin Pract. 1995; 4(Suppl 2):S88-94.
78. Pichichero ME, Cohen R. Shortened course of antibiotic therapy for acute otitis media, sinusitis and tonsillopharyngitis. Pediatr Infect Dis J. 1997; 16:680-95. https://pubmed.ncbi.nlm.nih.gov/9239773
79. Mehra S, Van Moerkerke M, Welck J et al. Short course therapy with cefuroxime axetil for group A streptococcal tonsillopharyngitis in children. Pediatr Infect Dis J. 1998; 17:452-7. https://pubmed.ncbi.nlm.nih.gov/9655533
80. Bisno AL, Gerber MA, Gwaltney JM et al. Practice guidelines for the diagnosis and management of group A streptococcal pharyngitis. Clin Infect Dis. 2002; 35:113-25. https://pubmed.ncbi.nlm.nih.gov/12087516
81. McCracken GH. Treatment of acute otitis media in an era of increasing microbial resistance. Pediatr Infect Dis J. 1998; 17:576-9. https://pubmed.ncbi.nlm.nih.gov/9655564
82. Klein JO. Otitis Media. Clin Infect Dis J. 1994; 19:823-33.
88. Bauchner H, Adams W, Barnett E et al. Therapy for acute otitis media: preference of parents for oral or parenteral antibiotics. Arch Pediatr Adolesc Med. 1996; 150:396-9. https://pubmed.ncbi.nlm.nih.gov/8634735
89. Dowell SF, Butler JC, Giebink GS et al. Acute otitis media: management and surveillance in an era of pneumococcal resistance—a report from the drug-resistant Streptococcal pneumoniae Therapeutic Working Group. Pediatr Infect Dis J. 1999; 18:1-9. https://pubmed.ncbi.nlm.nih.gov/9951971
90. Klein JO. Current recommendations on the therapy of otitis media. Pediatr Infect Dis J. 1998; 17:1058-9. https://pubmed.ncbi.nlm.nih.gov/9849999
91. Poole MD. Implications of drug-resistant Streptococcus pneumoniae for otitis media. Pediatr Infect Dis J. 1998; 17:953-6. https://pubmed.ncbi.nlm.nih.gov/9802652
92. Cohen R, Levy C, Boucherat M et al. A multicenter, randomized, double-blind trial of 5 versus 10 days of antibiotic therapy for acute otitis media in young children. J Pediatr. 1998; 133:634-9. https://pubmed.ncbi.nlm.nih.gov/9821420
93. Mendelman PM, Del Beccaro MA, McLinn SE et al. Cefpodoxime proxetil compared with amoxicillin-clavulanate for the treatment of otitis media. J Pediatr. 1992; 121:459-65. https://pubmed.ncbi.nlm.nih.gov/1517926
94. Arguedas AG, Zaleska M, Stutman HR et al. Comparative trial of cefprozil vs. amoxicillin clavulanate potassium in the treatment of children with acute otitis media with effusion. Pediatr Infect Dis J. 1991; 10:375-80. https://pubmed.ncbi.nlm.nih.gov/1906160
95. Berman S. Otitis media in children. N Engl J Med. 1995; 332:1560-5. https://pubmed.ncbi.nlm.nih.gov/7739711
96. White LL, Holimon TD, Tepedino JT et al. Antimicrobials prescribed for otitis media in a pediatric Medicaid population. Am J Health-Syst Pharm. 1996; 53:2963-9. https://pubmed.ncbi.nlm.nih.gov/8974159
97. Block SL, Harrison CJ, Hedrick JA et al. Penicillin-resistant Streptococcus pneumoniae in acute otitis media: risk factors, susceptibility patterns and antimicrobial management. Pediatr Infect Dis J. 1995; 14:751-9. https://pubmed.ncbi.nlm.nih.gov/8559623
98. Mandel EM, Casselbrandt ML, Rockette HE et al. Efficacy of 20- versus 10-day antimicrobial treatment for acute otitis media. Pediatrics. 1995; 96:5-13. https://pubmed.ncbi.nlm.nih.gov/7596722
99. Cohen R, Navel M, Grunberg J et al. One dose ceftriaxone vs. ten days of amoxicillin/clavulanate therapy for acute otitis media: clinical efficacy and change in nasopharyngeal flora. Pediatr Infect Dis J. 1999; 18:403-9. https://pubmed.ncbi.nlm.nih.gov/10353511
100. Hoppe HL, Johnson CE. Otitis media: focus on antimicrobial resistance and new treatment options. Am J Health-Syst Pharm. 1998; 55:1881-97. https://pubmed.ncbi.nlm.nih.gov/9784768
101. Hoberman A, Paradise JL, Burch DJ et al. Equivalent efficacy and reduced occurrence of diarrhea from a new formulation of amoxicillin/clavulanate potassium (Augmentin) for treatment of acute otitis media in children. Pediatr Infect Dis J. 1997; 16:463-70. https://pubmed.ncbi.nlm.nih.gov/9154538
102. Thomsen J, Sederberg-Olsen J, Balle V et al. Antibiotic treatment of children with secretory otitis media: amoxicillin-clavulanate is superior to penicillin V in a double-blind randomized study. Arch Otolaryngol Head Neck Sur. 1997; 123:695-9.
103. Dowell SF, Marcy SM, Phillips WR et al. Otitis media—principles of judicious use of antimicrobial agents. Pediatrics. 1998; 101:165-71.
104. Stool SE, Berg AO, Berman S et al for the Otitis Media Guideline Panel. Otitis media with effusion in young children. Clinical Practice Guideline. Number 12. AHCPR Publication No. 94-0622. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, US Department of Health and Human Resources. July 1994.
105. Hsu GS, Levine SC, Giebink GS. Management of otitis media using agency for health care policy and research guidelines. Otolaryngol Head Neck Surg. 1998; 118:437-43. https://pubmed.ncbi.nlm.nih.gov/9560092
106. Williams RL, Chalmers TC, Stange KC et al. Use of antibiotics in preventing recurrent acute otitis media and in treating otitis media with effusion: a meta-analytic attempt to resolve the brouhaha. JAMA. 1993; 270:1344-51. https://pubmed.ncbi.nlm.nih.gov/8141875
107. Bluestone CD. Ear and mastoid infections. In: Gorbach SL, Bartlett JG, Blacklow NR, eds. Infectious Diseases. Philadelphia, PA: WB Saunders; 1998:530-9.
108. Goldstein EJC, Citron DM. Comparative susceptibilities of 173 aerobic and anaerobic bite wound isolates to sparfloxacin, temafloxacin, clarithromycin, and older agents. Antimicrob Agents Chemother. 1993; 37:1150-3. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC187919/ https://pubmed.ncbi.nlm.nih.gov/8390810
109. Abrahamian FM. Dog bites: bacteriology, management, and prevention. Curr Infect Dis Rep. 2000; 2:446-453. https://pubmed.ncbi.nlm.nih.gov/11095891
110. Mortensen JE, Giger O, Rodgers GL. In vitro activity of oral antimicrobial agents against clinical isolates of Pasteurella multocida. Diagn Microbiol Infect Dis. 1998; 30:99-102. https://pubmed.ncbi.nlm.nih.gov/9554176
111. Anon. The choice of antibacterial drugs. Med Lett Drugs Ther. 2001; 43:69-78. https://pubmed.ncbi.nlm.nih.gov/11518876
113. Jick H, Porter JB. Potentiation of ampicillin skin reactions by allopurinol or hyperuricemia. J Clin Pharmacol. 1981; 21:456-8. https://pubmed.ncbi.nlm.nih.gov/6458626
114. Jick H, Slone D, Shapiro S et al. Excess of ampicillin rashes associated with allopurinol or hyperuricemia. N Engl J Med. 1972; 286:505-7. https://pubmed.ncbi.nlm.nih.gov/4258181
115. American Academy of Pediatrics and American Academy of Family Physicians Subcommittee on Management of Acute Otitis Media. Diagnosis and management of acute otitis media. Pediatrics. 2004: 113:1451-65.
116. American Academy of Pediatrics, American Academy of Family Physicians, American Academy of Otolaryngology-Head and Neck Surgery, and American Academy of Pediatrics Subcommittee on Otitis Media with Effusion. Otitis media with effusion. Pediatrics. 2004: 113:1412-29.
302. McDonald LC, Gerding DN, Johnson S et al. Clinical Practice Guidelines for Clostridium difficile Infection in Adults and Children: 2017 Update by the Infectious Diseases Society of America (IDSA) and Society for Healthcare Epidemiology of America (SHEA). Am J Respir Crit Care Med. 2019; 200:e93-e142. https://pubmed.ncbi.nlm.nih.gov/29562266
305. Metlay JP, Waterer GW, Long AC et al. Treatment of Drug-Resistant Tuberculosis. An Official ATS/CDC/ERS/IDSA Clinical Practice Guideline. Am J Respir Crit Care Med. 2019; 200:e45-e67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6812437/ https://pubmed.ncbi.nlm.nih.gov/31573350
306. Nahid P, Mase SR, Migliori GB et al. Diagnosis and Treatment of Adults with Community-acquired Pneumonia. An Official Clinical Practice Guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019; 200:e45-e67. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6857485/ https://pubmed.ncbi.nlm.nih.gov/31729908
344. Workowski KA, Bachmann LH, Chan PA et al. Sexually Transmitted Infections Treatment Guidelines, 2021. MMWR Recomm Rep. 2021; 70:1-187. https://pubmed.ncbi.nlm.nih.gov/34292926
Related/similar drugs
Augmentin
Augmentin is a prescription antibiotic combining amoxicillin and clavulanate to treat bacterial ...
Cefdinir
Cefdinir is used for bacterial infection, bronchitis, middle ear infections, pneumonia, sinusitis ...
Ozempic
Learn about Ozempic (semaglutide) for type 2 diabetes treatment, weight management, cardiovascular ...
Clindamycin
Clindamycin (Cleocin) is used to treat serious infections caused by bacteria. Includes clindamycin ...
Levofloxacin
Levofloxacin is a fluoroquinolone antibiotic used to treat serious bacterial infections and prevent ...
Cephalexin
Cephalexin is a cephalosporin antibiotic used to treat bacterial infections like respiratory, skin ...
Ceftriaxone
Ceftriaxone is used for bacteremia, bacterial endocarditis prevention, bacterial infection, bone ...
Metronidazole
Metronidazole is an antibiotic used to fight bacteria in your body. Learn about side effects ...
Ciprofloxacin
Ciprofloxacin is an antibiotic belong to a group of drugs called fluoroquinolones. Learn about side ...
Doxycycline
Doxycycline is a tetracycline antibiotic used to treat many different bacterial infections such as ...
Frequently asked questions
- Amoxicillin rash: When should I be concerned?
- What are the best antibiotics for pneumonia?
- Does AMOX-CLAV treat an abcessed tooth?
- Can Amox-Clav tablets be crushed?
More about amoxicillin / clavulanate
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (912)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: penicillins/beta-lactamase inhibitors
- En español
Patient resources
Professional resources
- Amoxicillin and Clavulanate Chewable prescribing information
- Amoxicillin and Clavulanate ER Tablets (FDA)
- Amoxicillin and Clavulanate Oral Suspension (FDA)
- Amoxicillin and Clavulanate Tablets (FDA)
Other brands
Augmentin, Amoclan, Augmentin ES-600, Augmentin XR