Amiodarone (Monograph)
Brand names: Cordarone, Pacerone
Drug class: Class III Antiarrhythmics
Introduction
Class III antiarrhythmic agent; also exhibits activity in each of the 4 Vaughn-Williams antiarrhythmic classes, including some class I (membrane-stabilizing) antiarrhythmic action.
Uses for Amiodarone
Ventricular Arrhythmias
Treatment to suppress or prevent the recurrence of documented life-threatening ventricular arrhythmias (e.g., recurrent VF; recurrent, hemodynamically unstable VT) that do not respond to documented adequate dosages of other currently available antiarrhythmic agents or when alternative antiarrhythmic agents are not tolerated.
Used during cardiac arrest for treatment of refractory (i.e., unresponsive to CPR, defibrillation, and a vasopressor [e.g., epinephrine]) VF or pulseless VT. Considered the preferred antiarrhythmic drug for this use in current ACLS guidelines in adults; lidocaine may be used as an alternative. In pediatric patients, current evidence supports use of either amiodarone or lidocaine.
Also may be used for treatment of wide-complex tachycardias during periarrest period; included in current ACLS guidelines for both adult and pediatric tachycardia.
Treatment of sustained monomorphic VT not associated with angina, pulmonary edema, or hypotension† [off-label], or hemodynamically stable monomorphic VT† [off-label] .
Treatment of polymorphic (irregular) VT† [off-label] associated with myocardial ischemia in the absence of QT interval prolongation.
Has been used for primary prevention† [off-label] of sustained VT (i.e., VT lasting >30 seconds and/or associated with hemodynamic compromise), VF, or sudden cardiac death in patients with nonsustained ventricular arrhythmia following MI.
Has been used in a limited number of patients for life-threatening ventricular arrhythmias associated with post-infarction aneurysm† [off-label] or with chronic myocarditis induced by Chagas’ disease† .
Supraventricular Tachyarrhythmias
Used for suppression and prevention of various supraventricular tachycardias (SVTs)†.
Because of higher risk of toxicity and proarrhythmic effects, antiarrhythmic agents generally reserved for patients who do not respond to or cannot be treated with AV nodal blocking agents (β-adrenergic blocking agents, diltiazem, verapamil).
Some experts state amiodarone may be useful when ventricular rate control is needed but AV nodal blocking agents are contraindicated (e.g., patients with preexcited atrial arrhythmias associated with an accessory pathway†).
May be effective for conversion of atrial fibrillation† to normal sinus rhythm (i.e., rhythm control); however, other antiarrhythmic agents (e.g., flecainide, dofetilide, propafenone, ibutilide) are preferred.
Used to maintain sinus rhythm in patients with atrial fibrillation or flutter†.
Termination of paroxysmal supraventricular tachycardia (PSVT)†, including atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT) (e.g., Wolff-Parkinson-White syndrome); generally reserved for use when other therapies are ineffective or contraindicated. Avoid IV use in patients with Wolff-Parkinson-White syndrome who have preexcited atrial fibrillation; may accelerate ventricular rate and potentially cause life-threatening ventricular arrhythmias.
Also used for long-term prevention of PSVT†, including those refractory to other antiarrhythmic agents.
Has been used in the treatment of atrial tachycardia†.
Has been effective in the prevention of supraventricular arrhythmias associated with bradycardia-tachycardia syndrome†.
Angina
Has been used in treatment of chronic stable angina pectoris† and Prinzmetal variant angina†; because of potential toxicity, generally not considered a first-line agent but may have beneficial antianginal effect in patients receiving the drug for the management of arrhythmias.
Hypertrophic Cardiomyopathy
Has been used in the management of ventricular and supraventricular arrhythmias associated with hypertrophic cardiomyopathy†.
Amiodarone Dosage and Administration
General
-
Administer lowest effective dosage to minimize the risk and occurrence of adverse effects.
-
Adjust dosage carefully according to individual requirements and response and the general condition and cardiovascular status of the patient. Adjustment of maintenance dosage is difficult due to variable absorption and elimination of amiodarone; dosage reduction or temporary withdrawal or discontinuance of the drug may be required.
-
When dosage adjustment is necessary, close monitoring for an extended period of time is recommended.
-
Clinical and ECG monitoring of cardiac function, including appropriate ambulatory ECG monitoring (e.g., Holter monitoring) and/or programmed electrical stimulation (PES), as appropriate, is recommended.
-
Monitor plasma amiodarone concentrations if patient does not respond or experiences unexpectedly severe toxicity.
-
When initiating therapy in patients receiving other antiarrhythmic agents, attempt to gradually discontinue the other antiarrhythmic agents.
Administration
Administer orally or by IV infusion.
Also has been administered via intraosseous (IO) injection† during cardiac resuscitation.
Oral Administration
Usually administered once daily. Administer in divided doses (e.g., twice daily) with meals when dosages ≥1 g daily are administered (e.g., during the loading-dose phase of therapy) or when intolerable adverse GI effects occur.
Administer in a consistent manner relative to food intake.
Administration of a loading-dose phase of therapy is required for the management of life-threatening ventricular arrhythmias; administer oral loading dose in hospital setting and monitor closely until risk of recurrent VT or VF has abated.
Extemporaneous Oral Suspension
Extemporaneous oral suspensions of amiodarone have been prepared using the tablets and a commercially available vehicle.
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral suspension of amiodarone have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web]
|
Concentration Standards |
|---|
|
5 mg/mL 20 mg/mL for doses of 75 mg or greater |
Amiodarone needs to have a pH very close to 8 to assure particle consistency
IV Administration
IV therapy may be used for acute antiarrhythmic therapy until cardiac rhythm is stabilized and oral therapy can be initiated. IV therapy may be required for 48–96 hours, but may be administered safely for longer periods. Experience with IV administration of amiodarone exceeding 3 weeks is limited.
Administer in 3-phase sequence: rapid loading phase, slow loading phase, and maintenance infusion phase.
Dilute amiodarone hydrochloride concentrate prior to administration by IV infusion.
Administer solutions containing an amiodarone hydrochloride concentration >2 mg/mL via central venous catheter.
Use in-line filter.
Amiodarone hydrochloride infusions exceeding 2 hours should be administered in 5% dextrose in glass or polyolefin containers . Manufacturer recommends using PVC tubing (used in clinical studies). Leaching of plasticizer diethylhexylphthalate (DEHP) from IV tubing may occur.
Standardize 4 Safety
Standardized concentrations for IV amiodarone have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care. Multidisciplinary expert panels were convened to determine recommended standard concentrations. Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label. For additional information on S4S (including updates that may be available), see [Web].
Dosing units differ from concentration units
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
1.8 mg/mL |
mg/min |
|
Pediatric patients (<50 kg) |
1.8 mg/mL |
mcg/kg/min |
Dilution
For the first rapid loading infusion or for supplemental infusions, add 3 mL of amiodarone hydrochloride concentrate to 100 mL of 5% dextrose, resulting in a final concentration of 1.5 mg/mL.
For the slow loading infusion and maintenance infusion, add 18 mL of amiodarone hydrochloride concentrate to 500 mL of 5% dextrose, resulting in a final concentration of 1.8 mg/mL. For subsequent maintenance infusions, solutions containing a final amiodarone hydrochloride concentration of 1–6 mg/mL may be used.
Rate of Administration
For treatment of ventricular arrhythmias in adults, 15 mg/minute for 10 minutes (rapid loading phase), then 1 mg/minute for 6 hours (slow loading phase), then 0.5 mg/minute (initial maintenance phase) for 18 hours; infuse supplemental doses of 150 mg over 10 minutes (at a rate of 15 mg/minute). Initial (rapid) loading infusion rate should not exceed 30 mg/minute. Monitor initial rate of infusion closely; do not exceed recommended rate.
Use volumetric infusion pump. Do not use drop-counter infusion sets; may result in underdosage.
Dosage
Available as amiodarone hydrochloride; dosage expressed in terms of the salt.
Pediatric Patients
Ventricular Arrhythmias†
Oral
Pediatric dosage has not been established; dosage may vary considerably. Some clinicians have recommended loading dosages of 10–15 mg/kg daily or 600–800 mg/1.73 m2 daily for approximately 4–14 days and/or until adequate control of cardiac arrhythmias is achieved or adverse effects become prominent. Subsequently, reduce dosage to 5 mg/kg daily or 200–400 mg/1.73 m2 daily for several weeks; if possible, reduce dosage to the lowest effective level.
Children <1 year of age may require higher oral loading and maintenance dosages than older children when dosage is calculated on the basis of body weight, but not on the basis of body surface area†.
Pediatric Resuscitation
IV or IO†Refractory VF or pulseless VT: 5 mg/kg as a rapid bolus. May repeat twice up to 15 mg/kg (maximum single dose of 300 mg).
To minimize pediatric exposure to DEHP, may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).
Wide-complex Tachycardias in Patients Not in Cardiac Arrest
IV5 mg/kg over 20–60 minutes (depending on urgency).
To minimize pediatric exposure to DEHP, may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).
Supraventricular Arrhythmias†
Oral
Pediatric dosage has not been established; dosage may vary considerably. Some clinicians have recommended loading dosages of 10–15 mg/kg daily or 600–800 mg/1.73m2 daily for approximately 4–14 days and/or until adequate control of cardiac arrhythmias is achieved or adverse effects become prominent. Subsequently, reduce dosage to 5 mg/kg daily or 200–400 mg/1.73 m2 daily for several weeks; if possible, reduce dosage to the lowest effective level.
Children <1 year of age may require higher oral loading and maintenance dosages than older children when dosage is calculated on the basis of body weight, but not on the basis of body surface area.†
IV
5 mg/kg over 20–60 minutes depending on urgency.
To minimize pediatric exposure to DEHP, may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).
Adults
Ventricular Arrhythmias
Oral
|
Loading Dose |
800–1600 mg daily for 1–3 weeks or until initial therapeutic response occurs |
|
Dosage Adjustment |
When adequate control of ventricular arrhythmias is achieved or adverse effects become prominent, decrease dosage to 600–800 mg daily for about 1 month |
|
Maintenance Dosage |
400–600 mg daily; if possible, cautiously reduce dosage to 200 mg daily |
Consult published protocols for specific information about oral loading doses >1600 mg daily or IV loading-dose regimens† followed by oral therapy. If an IV loading-dose regimen is used, initiate oral therapy as soon as possible after an adequate response is obtained and gradually eliminate IV amiodarone.
IV
Total initial dosage during first 24 hours is approximately 1000 mg.
|
Loading Phase |
Initial rapid loading phase: 150 mg administered at rate of 15 mg/minute (i.e., over 10 minutes) |
|
Followed by slow loading phase: 360 mg administered at rate of 1 mg/minute (i.e., over 6 hours) |
|
|
Maintenance Phase |
First maintenance phase: 540 mg administered at rate of 0.5 mg/minute (i.e., over 18 hours) |
|
Maintenance Phase |
0.5 mg/minute (i.e., 720 mg over 24 hours); can be administered for 2–3 weeks |
|
Breakthrough Episodes of VF or Hemodynamically Unstable VT |
Supplemental infusion of 150 mg administered at rate of 15 mg/minute (i.e., over 10 minutes) |
IV/Oral
When switching from IV to oral therapy, oral dosage depends on dose and duration of IV therapy, as well as bioavailability of oral drug. When switching from IV to oral therapy, clinical monitoring is recommended, particularly for geriatric patients.
Assuming 720-mg/day infusion (0.5 mg/minute)
IV amiodarone not intended for maintenance treatment
|
Duration of IV Therapy |
Initial Oral Daily Dosage |
|---|---|
|
<1 week |
800–1600 mg |
|
1–3 weeks |
600–800 mg |
|
>3 weeks |
400 mg |
ACLS
IV or IO†Refractory VF or pulseless VT: 300 mg by rapid IV/IO injection; may consider an additional dose of 150 mg.
Supraventricular Arrhythmias†
IV
For acute treatment of SVT, 150 mg over 10 minutes. Follow with 1 mg/minute for 6 hours, then 0.5 mg/minute for remaining 18 hours or initiate oral dosing.
Oral
For ongoing management of SVT, some experts recommend 400–600 mg daily (in divided doses) in adults for approximately 2–4 weeks, followed by a maintenance dosage of 100–200 mg daily.
Consult published protocols for specific information about oral loading-dose regimens using higher dosages.
Atrial Fibrillation†
IV
When used for rate control in patients with atrial fibrillation, some experts recommend an initial IV dose of 300 mg over 1 hour, followed by 10–50 mg/hr over 24 hours.
Oral
Usual maintenance dose is 100–200 mg daily.
Long-term Management of Recurrent Atrial Fibrillation†
Oral
Initially, 10 mg/kg daily for 14 days, followed by 300 mg daily for 4 weeks, and then 200 mg daily.
Prescribing Limits
Pediatric Patients
Ventricular Arrhythmias†
IV
Maximum single dose: 300 mg, up to a total dose of 15 mg/kg.
Adults
Ventricular Arrhythmias
IV
Mean daily doses >2.1 g are associated with an increased risk of hypotension.
Limited experience with IV administration of amiodarone for >3 weeks.
Special Populations
Hepatic Impairment
Dosage reduction recommended in patients with substantial hepatic impairment.
Renal Impairment
Routine dosage reduction not required.
Geriatric Patients
Select dosage with caution, usually starting at low end of dosage range, because of possible age-related decrease in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy; however, dosage requirements generally similar in geriatric and younger adults.
Use caution with high dosages due to increased susceptibility to drug-induced bradycardia and conduction disturbances.
Cautions for Amiodarone
Contraindications
-
Cardiogenic shock.
-
Severe sinus node dysfunction resulting in marked sinus bradycardia (unless a functioning pacemaker is present).
-
Second- or third-degree AV block (unless a functioning pacemaker is present).
-
Bradycardia that has caused syncope (unless a functioning pacemaker is present).
-
Known hypersensitivity to amiodarone or any ingredient in the formulation, including iodine.
Warnings/Precautions
Warnings
Mortality
Potentially fatal toxicities and severe adverse effects; use principally for documented life-threatening ventricular arrhythmias.
Amiodarone therapy should be administered only by physicians experienced in the management of life-threatening arrhythmias who have access to laboratory facilities necessary to adequately monitor efficacy and adverse effects, including continuous ECG monitoring and electrophysiologic techniques for evaluating the patient in both ambulatory and hospital settings.
Pulmonary Effects
Possible acute-onset (days to weeks) pulmonary injury; findings may include pulmonary infiltrates and/or mass on radiograph, pulmonary alveolar hemorrhage, bronchospasm, wheezing, fever, dyspnea, cough, hemoptysis, or hypoxia, sometimes leading to respiratory failure and/or death.
Potentially fatal pulmonary toxicity may result from pulmonary interstitial pneumonitis (or alveolitis) or hypersensitivity pneumonitis. Toxicity is usually reversible following discontinuance of the drug (with or without corticosteroid therapy).
Baseline pulmonary function testing (prior to initiating therapy) and periodic (e.g., every 3–6 months) chest radiographs, clinical evaluation, and pulmonary function testing recommended.
If hypersensitivity pneumonitis occurs, discontinue amiodarone and initiate corticosteroid therapy.
If interstitial pneumonitis occurs, reduce dosage or discontinue therapy, especially if other acceptable antiarrhythmic therapies are available. Supportive treatment, including mechanical ventilation, may be required.
Use with caution, if at all, in patients with preexisting pulmonary disease (e.g., chronic obstructive disease, reduced pulmonary diffusion capacity ); poorer prognosis if pulmonary toxicity develops in such patients.
If new respiratory symptoms develop, consider the possibility of amiodarone-induced pulmonary toxicity; clinical and radiographic evaluation, as well as scintigraphic and pulmonary function testing (including diffusion capacity), if necessary, are recommended. Carefully assess respiratory symptoms and rule out other causes of respiratory impairment (e.g., CHF, pulmonary embolism, malignancy, infectious causes) before discontinuing therapy.
Bronchiolitis obliterans organizing pneumonia (possibly fatal) and pleuritis reported during postmarketing experience.
Hepatic Effects
Possible liver function test abnormalities; abnormalities are usually minor, not accompanied by clinical symptoms, and generally return to normal following dosage reduction or discontinuance of the drug.
Rarely, potentially fatal hepatic injury (i.e., clinical hepatitis, cholestatic hepatitis, hepatocellular necrosis, cirrhosis) has occurred.
Monitor serum hepatic enzyme concentrations at regular intervals. Reduce oral dosage, decrease IV infusion rate, or discontinue therapy if enzyme concentrations are >3 times normal values in patients with normal pretreatment values or twice baseline pretreatment values in patients with elevated pretreatment values or if hepatomegaly or progressive hepatic injury occurs.
Possible acute centrolobular confluent hepatic necrosis during IV therapy; may be related to a much higher loading dose concentration and more rapid infusion rate than recommended. Closely monitor initial concentration and rate of IV infusion; do not exceed recommended initial drug concentration and infusion rate.
Arrhythmogenic Effects
Possible worsening of existing arrhythmias or occurrence of new arrhythmias. Arrhythmogenic effects include progression of VT to VF, sustained VT, increased resistance to cardioversion, atrial fibrillation, nodal arrhythmia, and atypical VT (torsades de pointes).
Monitor for QTc prolongation during IV infusion of amiodarone.
If new signs of arrhythmia appear, consider possibility of hyperthyroidism.
Chronic administration of antiarrhythmic drugs (e.g., amiodarone) in patients with an implanted cardiac device (e.g., defibrillator, pacemaker) may change electrical conduction properties of the heart and potentially affect pacing and/or defibrillating thresholds. Therefore, manufacturer recommends assessment to ensure appropriate device parameters before and during amiodarone therapy.
Electrolyte Abnormalities
Electrolyte abnormalities (e.g., hypokalemia, hypomagnesemia) may increase arrhythmogenic effects. Evaluate patient for potassium or magnesium deficiency; if present, correct deficiency prior to initiation of therapy.
Monitor electrolyte and acid-base balance in patients with severe or prolonged diarrhea and in patients receiving diuretics concomitantly.
Effects on Cardiac Conduction
Possible AV, intraventricular, or SA block; SA node dysfunction (e.g., symptomatic sinus bradycardia), sinus arrest with suppression of escape foci); or bradycardia (usually associated with IV therapy).
Administer IV amiodarone in a setting where a temporary pacemaker is available for patients with known predisposition to bradycardia or AV block.
Ocular Effects
Optic neuropathy and/or optic neuritis may occur at any time during amiodarone therapy; usually results in visual impairment and may progress to permanent blindness.
Baseline and routine (e.g., after the first 6 months and then annually and/or as necessary) ophthalmologic examinations recommended, including slit-lamp and funduscopic tests.
Careful monitoring recommended for patients experiencing visual disturbances or those receiving long-term therapy. If visual impairment occurs (e.g., changes in visual acuity, decreases in peripheral vision), prompt ophthalmologic examination recommended.
If optic neuropathy and/or optic neuritis develops, reevaluate therapy; consider risks and complications against the possible benefits of antiarrhythmic therapy.
Thyroid Effects
Thyroid nodules or thyroid cancer reported during postmarketing experience, sometimes accompanied by hyperthyroidism.
Possible altered thyroid function test results: increased serum thyroxine (T4) and reverse triiodothyronine (rT3) concentrations, decreased serum T3 concentrations.
Possible hypothyroidism or hyperthyroidism. Amiodarone-induced hyperthyroidism may result in thyrotoxicosis and/or arrhythmia breakthrough or aggravation; fatalities have occurred.
Thyroid function tests recommended prior to initiating therapy and at periodic intervals (approximately every 3–6 months) thereafter, particularly in geriatric patients and/or in patients with a history of thyroid nodules, goiter, or other thyroid dysfunction.
If hypothyroidism occurs, reduce amiodarone dosage and/or carefully supplement with thyroid agents if necessary; discontinuance of amiodarone may be required.
If hyperthyroidism occurs, aggressive therapy (including dosage reduction or discontinuance of amiodarone) is indicated, since clinical manifestations (i.e., cardiac arrhythmias) may be potentially serious and may be fatal. Antithyroid drugs, adrenergic blockers, and/or temporary corticosteroid therapy may be necessary. However, antithyroid agents appear to be of limited benefit when used alone, since high intrathyroidal iodine stores (typically observed in patients receiving long-term amiodarone therapy) antagonize the inhibitory effects of antithyroid drugs on thyroidal iodine utilization. Radioactive iodine treatment contraindicated because of low radioiodine uptake in amiodarone-associated hyperthyroidism. In patients in whom aggressive treatment of amiodarone-induced toxicity has failed or the drug cannot be discontinued because it is the only drug effective against the resistant arrhythmia, thyroidectomy may be an option. However, experience with surgical management is limited and such treatment could induce thyroid storm; therefore, careful surgical and anesthetic management is required.
Fetal/Neonatal Morbidity
Possible adverse effects on fetal thyroid function and overall development. Possible congenital goiter/hypothyroidism and hyperthyroidism. Women should avoid becoming pregnant during amiodarone therapy. Use during pregnancy only when the potential benefits justify the possible risks to the fetus. If amiodarone is used during pregnancy or the patient becomes pregnant while taking the drug, apprise patient of potential hazard to fetus.
Hypotension
Hypotension associated with IV therapy; mean daily IV dosages >2.1 g associated with increased risk of hypotension. Hypotension may be refractory in some cases, resulting in death. Monitor initial rate of infusion closely; do not exceed recommended rate.
Hypotension (possibly severe) reported during open-heart surgery (during and/or following cardiopulmonary bypass) in amiodarone-treated patients.
Arrhythmia Recurrence
Possible recurrence of life-threatening arrhythmias after dosage reduction or discontinuance of therapy; time to recurrence may range from weeks to months. Prolonged hospitalization or intensive ambulatory monitoring (e.g., via telemetric ECG), possibly with periodic determination of plasma amiodarone concentrations, may be required.
Sensitivity Reactions
Hypersensitivity Reactions
Possible hypersensitivity pneumonitis. If hypersensitivity pneumonitis occurs, initiate corticosteroid therapy and discontinue amiodarone. Rechallenge may result in more rapid and more severe adverse effects than rechallenge with amiodarone in patients with interstitial pneumonitis.
Anaphylactic/anaphylactoid reaction (including shock) and angioedema reported during postmarketing experience.
Dermatologic Reactions
Possible photosensitivity. Reactions generally begin within 2 hours of exposure to sunlight and last for 1–3 days; may last a week in severe cases. Reactions may occur up to 4 months following discontinuance of the drug.
Possible pigmentary changes (blue-gray discoloration) to exposed areas of the body (e.g., face, hands) in patients receiving long-term therapy, in patients with fair complexions, or following excessive exposure to sunlight. Usually slowly reversible following discontinuance of the drug.
Sunscreen agents, protective clothing, and avoidance of excessive exposure to sunlight are recommended.
Toxic epidermal necrolysis (sometimes fatal), erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, skin cancer, and pruritus reported during postmarketing experience.
General Precautions
Ocular Effects
Corneal microdeposits occur in almost all patients. Usually not associated with visual disturbances; however, halo vision, blurred vision, photophobia, and dry eyes may occur.
Corneal deposits are related to dosage and duration of therapy. Reversible following dosage reduction or discontinuance of therapy. Asymptomatic, nonprogressive deposits do not necessitate dosage reduction or drug discontinuance.
Routine ophthalmologic examinations, including slit-lamp and funduscopic tests, recommended.
Most manufacturers of corneal refractive laser surgery devices consider the procedure to be contraindicated in patients receiving amiodarone.
Nervous System Effects
Possible peripheral neuropathy and proximal myopathy.
Delirium, hallucination, confusional state, pseudotumor cerebri, disorientation, and parkinsonian symptoms (e.g., akinesia, bradykinesia) reported during postmarketing experience.
Cardiac Failure
Possible new or worsened heart failure; rarely requires discontinuance of the drug.
Pulmonary Precautions
Possible ARDS following cardiothoracic or other surgery. Closely monitor forced inspiratory oxygen and tissue oxygenation. Preoperative pulmonary function testing recommended for patients undergoing cardiothoracic surgery.
Symptomatic Bradycardia in Patients Receiving HCV Treatment
Symptomatic bradycardia, including cases requiring pacemaker intervention, reported in patients receiving amiodarone concomitantly with an HCV treatment regimen containing sofosbuvir in conjunction with another HCV direct-acting antiviral (DAA), including ledipasvir, simeprevir, or daclatasvir. Fatal cardiac arrest reported in a patient receiving amiodarone concomitantly with fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir).
In most reported cases, bradycardia occurred within hours to days after HCV treatment initiated in patients receiving amiodarone (also has been observed up to 2 weeks after initiation of HCV treatment) and resolved after HCV treatment discontinued. Mechanism for this adverse cardiovascular effect unknown.
Patients who may be at increased risk for symptomatic bradycardia if amiodarone used concomitantly with HCV treatment regimen containing sofosbuvir with another DAA include those also receiving a β-adrenergic blocking agent, those with underlying cardiac comorbidities, and/or those with advanced liver disease.
Concomitant use of amiodarone with HCV treatment regimen containing sofosbuvir with another DAA not recommended.
If there are no alternative HCV treatment options and regimen of sofosbuvir with another DAA must be used in a patient receiving amiodarone, advise patient about the risk of serious symptomatic bradycardia before initiating HCV treatment. Perform cardiac monitoring in an inpatient setting during first 48 hours of concomitant use of amiodarone and regimen of sofosbuvir with another DAA; subsequently, perform heart rate monitoring daily (outpatient or self-monitoring) through at least the first 2 weeks of concomitant use. Similar cardiac monitoring recommended in patients who discontinued amiodarone just prior to initiation of regimen of sofosbuvir with another DAA or if alternative antiarrhythmic agent cannot be used and amiodarone must be initiated in a patient already receiving regimen of sofosbuvir with another DAA.
Advise patients receiving amiodarone concomitantly with regimen of sofosbuvir with another DAA to immediately contact a clinician if signs or symptoms of bradycardia (e.g., near-fainting or fainting, dizziness or lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pain, confusion, memory problems) develop.
Specific Populations
Pregnancy
Category D.
Lactation
Amiodarone and desethylamiodarone are distributed into milk. Discontinue nursing.
Pediatric Use
Safety and efficacy not established; however, amiodarone has been used in children.
Large amounts of benzyl alcohol (e.g., 100–400 mg/kg daily) have been associated with toxicity in neonates; each mL of amiodarone hydrochloride injection contains 20.2 mg of benzyl alcohol.
Amiodarone hydrochloride injection leaches DEHP plasticizer from IV tubing; exposure to DEHP may adversely affect male reproductive tract development during fetal, infant, and toddler stages of development. Consider dosing methods to reduce potential exposure to DEHP.
Geriatric Use
Response similar to that in younger adults.
Possible increased susceptibility to bradycardia and conduction disturbances.
Possible thyroid effects.
Select dosage with caution, usually starting at low end of dosage range, because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Hepatic Impairment
Effects of hepatic impairment on amiodarone elimination have not been evaluated; however, amiodarone is extensively metabolized, probably in the liver. Consider dosage reduction in patients with substantial hepatic impairment.
Renal Impairment
Possible excessive accumulation of iodine and possible resultant thyroid effects.
Common Adverse Effects
IV administration: hypotension.
Oral therapy: adverse nervous system (e.g., malaise and fatigue, tremor and/or involuntary movements, lack of coordination, abnormal gait and/or ataxia, dizziness, paresthesia ) and GI (e.g., nausea, vomiting, constipation, anorexia ) effects.
Drug Interactions
Metabolized by CYP3A4 and CYP2C8.
Elimination half-life of amiodarone is long and variable; potential for interactions exists with drugs administered after discontinuance of amiodarone therapy.
Drugs, Foods, and Dietary or Herbal Supplements Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with substrates, inhibitors, or inducers of CYP3A4 are likely. Inhibits CYP isoenzymes 1A2, 2C9, 2D6, and 3A4; potential pharmacokinetic interaction with drugs metabolized by these isoenzymes (increased plasma concentrations). Amiodarone is a substrate for CYP3A4 and CYP2C8; drugs and other substances that inhibit these isoenzymes may decrease metabolism and increase serum concentrations of amiodarone.
Drugs with P-Glycoprotein-Mediated Clearance
Amiodarone inhibits the P-glycoprotein transport system, which may result in unexpectedly high plasma concentrations of drugs that are substrates for this transport system.
Drugs Affecting QT Interval
Potential pharmacodynamic interaction (additive effects on the QTc interval).
Antiarrhythmic Agents
Cautious use and close monitoring for possible adverse effects recommended if amiodarone is used concomitantly with other antiarrhythmic agents, particularly class IA antiarrhythmic agents.
Reserve concomitant use for the management of life-threatening arrhythmias unresponsive to monotherapy.
In general, reduce dosage of other antiarrhythmic agent(s) by 30–50% several days after initiating amiodarone therapy; assess necessity of continuing the other antiarrhythmic agent(s) after antiarrhythmic effect of amiodarone has been established.
In patients already receiving amiodarone, reduce initial dosage of other antiarrhythmic agent(s) by approximately 50%.
Specific Drugs, Foods, and Dietary or Herbal Supplements
|
Drug, Food, or Supplement |
Interaction |
Comments |
|---|---|---|
|
Agalsidase beta |
Theoretical risk of inhibited intracellular α-galactosidase activity |
Some clinicians recommend avoidance of concurrent use of biosynthetic forms of α-galactosidase and amiodarone |
|
Anesthetics, general |
Potential serious cardiovascular (e.g., hypotension) and cardiac (e.g., sinus bradyarrhythmias, AV block) effects |
Close perioperative monitoring is recommended |
|
Anticoagulants, oral |
Decreased warfarin clearance; increased PT in almost all patients. Can result in serious or fatal hemorrhage |
Reduce anticoagulant dosage by 33–50% when initiating amiodarone Frequent PT determinations and close observation for adverse effects recommended; adjust anticoagulant dosage as necessary PT may not return to normal for 1–4 months following discontinuance of amiodarone |
|
Azole antifungals |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) reported |
Assess risks versus benefits |
|
β-adrenergic blocking agents (e.g., propranolol) |
Possible potentiation of sinus bradycardia, sinus arrest, and AV block |
Concomitant therapy may be considered in patients with severe sinus bradycardia or sinus arrest following insertion of artificial pacemaker; monitor cardiac function |
|
Calcium-channel blocking agents (e.g., diltiazem, verapamil) |
Possible potentiation of sinus bradycardia, sinus arrest, and AV block |
Concomitant therapy may be considered in patients with severe sinus bradycardia or sinus arrest following insertion of artificial pacemaker |
|
Cardiac glycosides |
Increased serum digoxin concentrations and digoxin toxicity |
When initiating amiodarone therapy, reassess need for continued cardiac glycoside therapy; discontinue digoxin or reduce digoxin dosage by 50% Monitor serum digoxin concentrations carefully and reduce digoxin dosage as necessary Close observation for signs of cardiac glycoside toxicity recommended Monitor thyroid function carefully due to potential for altered cardiac glycoside sensitivity in patients with amiodarone-induced changes in thyroid function |
|
Cholestyramine |
Decreased plasma amiodarone concentrations and half-life |
|
|
Cimetidine |
Increased plasma amiodarone concentrations |
|
|
Cisapride (no longer commercially available in the US) |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) reported |
Concurrent use contraindicated |
|
Clopidogrel |
Potential interaction resulting in ineffective inhibition of platelet aggregation by clopidogrel |
|
|
Cyclosporine |
Increased plasma cyclosporine concentrations resulting in elevated serum creatinine concentrations |
|
|
Dextromethorphan |
Possible inhibition of dextromethorphan metabolism with prolonged administration (>2 weeks) of oral amiodarone |
|
|
Disopyramide |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes) |
|
|
Dolasetron |
Possible additive effects in prolonging QTc interval |
Use concomitantly with caution; monitor cardiac function |
|
Fentanyl |
Possible hypotension, bradycardia, and decreased cardiac output |
|
|
Flecainide |
Decreased flecainide clearance |
Reduce flecainide dosage by 30–50% several days after initiating amiodarone therapy Monitor patient and plasma flecainide concentrations closely; adjust flecainide dosage as necessary |
|
Fluoroquinolone anti-infectives (e.g., ciprofloxacin, gemifloxacin, levofloxacin, moxifloxacin) |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes) |
Avoid concomitant use |
|
Grapefruit juice |
Increased amiodarone concentrations. |
Avoid concomitant use. |
|
Halofantrine (no longer commercially available in the US) |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes) |
Avoid concomitant use |
|
HCV antivirals |
Regimen containing sofosbuvir with another DAA (e.g., ledipasvir, simeprevir, daclatasvir): May result in serious symptomatic bradycardia (mechanism unknown); effect on plasma concentrations of the drugs is unknown Simeprevir-containing regimen that does not include sofosbuvir: Modestly increased plasma concentrations of oral amiodarone due to intestinal CYP3A4 inhibition by simeprevir Fixed combination of ombitasvir, paritaprevir, and ritonavir (ombitasvir/paritaprevir/ritonavir) with dasabuvir: Increased plasma concentrations of amiodarone |
Regimen containing sofosbuvir with another DAA: Concomitant use not recommended; if concomitant use necessary, patient counseling and cardiac monitoring required Simeprevir-containing regimen that does not include sofosbuvir: Use concomitantly with caution; amiodarone therapeutic drug monitoring recommended, if available Ombitasvir/paritaprevir/ritonavir with dasabuvir: Use concomitantly with caution; amiodarone therapeutic drug monitoring recommended, if available |
|
HIV protease inhibitors |
HIV protease inhibitors used with low-dose ritonavir (ritonavir-boosted) or without low-dose ritonavir (unboosted): Possible increased plasma concentrations of amiodarone and the HIV protease inhibitor |
Ritonavir-boosted saquinavir or ritonavir-boosted tipranavir: Concomitant use not recommended Other ritonavir-boosted HIV protease inhibitors or unboosted HIV protease inhibitors: Use concomitantly with caution; monitor for amiodarone toxicity; consider monitoring ECG and amiodarone plasma concentrations |
|
HMG-CoA reductase inhibitors (statins) |
Increased risk of myopathy and/or rhabdomyolysis, particularly when used with higher dosages of certain statins (e.g., simvastatin) |
Reduce dosage of lovastatin (to ≤40 mg daily) or simvastatin (to ≤20 mg daily) during concomitant therapy with amiodarone |
|
Lidocaine |
Increased serum lidocaine concentrations; potential increase in adverse effects (e.g., sinus bradycardia, seizures) |
|
|
Loratadine |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) |
|
|
Macrolide antibiotics |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) |
Assess risks versus benefits |
|
Methotrexate |
Possible inhibition of methotrexate metabolism with prolonged administration (>2 weeks) of oral amiodarone |
|
|
Phenytoin |
Increased serum phenytoin concentrations; possible phenytoin toxicity (e.g., nystagmus, ataxia, lethargy) Possible decreased plasma amiodarone concentrations |
Monitor serum phenytoin concentrations and closely observe patient for signs of phenytoin toxicity; reduce phenytoin dosage as necessary |
|
Pimozide |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes) |
Concomitant use contraindicated |
|
Procainamide |
Increased plasma procainamide and N-acetylprocainamide (NAPA) concentrations; possible increases in QTc and QRS intervals and acceleration of ventricular tachycardia |
Reduce procainamide dosage by 20–33% when amiodarone therapy is initiated or discontinue procainamide therapy |
|
Quinidine |
Increased serum quinidine concentrations; possible marked QT prolongation and torsades de pointes |
Reduce quinidine dosage by 33–50% when amiodarone therapy is initiated or discontinue quinidine therapy Monitor serum quinidine concentrations carefully and reduce quinidine dosage as necessary; observe patient closely for signs of toxicity, including QT prolongation |
|
Rifampin |
Decreased plasma amiodarone and desethylamiodarone concentrations |
|
|
St. John’s wort (Hypericum perforatum) |
Potential decrease in amiodarone concentrations |
|
|
Trazodone |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) |
|
|
Ziprasidone |
Possible additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes) |
Avoid concomitant use |
Amiodarone Pharmacokinetics
Absorption
Bioavailability
Slowly and variably absorbed from the GI tract following oral administration; absolute bioavailability averages 50% (range: 22–86%). Considerable interindividual variation in plasma concentrations attained with a given dosage. Following oral administration, peak plasma concentrations usually occur within 3–7 hours.
Onset
Following oral administration, onset of antiarrhythmic activity is highly variable; however, a therapeutic response generally is not evident until 1–3 weeks after beginning therapy, even when loading doses are administered.
Duration
Antiarrhythmic effects generally persist for 10–150 days following withdrawal of long-term therapy; duration of antiarrhythmic activity is variable and unpredictable and appears to depend on length of therapy and type of arrhythmia.
Food
Food increases rate and extent of absorption.
Distribution
Extent
Following chronic oral administration, amiodarone and N-desethylamiodarone are distributed extensively into many body tissues and fluids. Tissue concentrations generally exceed concurrent plasma concentrations of the drug. After long-term therapy, concentrations of the metabolite usually are substantially higher than concentrations of unchanged drug in almost all tissues, except adipose tissue.
Following IV administration, amiodarone is rapidly and widely distributed.
Amiodarone and N-desethylamiodarone cross the placenta to a limited extent. Amiodarone and N-desethylamiodarone are distributed into milk.
Plasma Protein Binding
Approximately 96%.
Elimination
Metabolism
Extensively metabolized, probably in the liver and possibly in the intestinal lumen and/or GI mucosa, to at least one major metabolite, N-desethylamiodarone. This metabolite appears to possess substantial electrophysiologic and antiarrhythmic activity similar to amiodarone’s.
Elimination Route
Excreted almost completely in feces as unchanged drug and N-desethylamiodarone, presumably via biliary elimination.
Half-life
Half-life of amiodarone appears to be substantially more prolonged following multiple rather than single doses.
Following a single IV dose, the terminal elimination phase half-life of amiodarone averages 25 days (range 9–47 days); elimination half-life of N-desethylamiodarone equals or exceeds that of amiodarone.
Following chronic oral administration, amiodarone has an initial elimination half-life of about 2.5–10 days, followed by a terminal elimination half-life averaging 53 days; elimination half-life of N-desethylamiodarone averages 57–61 days.
Clearance may be more rapid in pediatric patients.
Clearance may be decreased in geriatric patients (>65 years of age).
Stability
Storage
Oral
Tablets
Tightly sealed containers at 20–25°C; protect from light. The manufacturer of one commercially available amiodarone tablet preparation (Pacerone) states the tablets may be exposed to 15–30°C.
Parenteral
Injection Concentrate
20–25°C; protect from light and excessive heat. Store ampuls in carton to protect from light until used. Light protection not necessary during administration.
Compatibility
Parenteral
Do not use evacuated glass containers for amiodarone hydrochloride infusions (incompatibility with a buffer in the container may cause precipitation). Polysorbate 80, a component of IV amiodarone injection, can cause leaching of diethylhexyl phthalate (DEHP) from IV tubing, including PVC tubing; leaching increases at lower than recommended flow rates and at higher than recommended infusion concentrations.
Solution Compatibilityc
Manufacturer states physically compatible in PVC container with amiodarone loss of <10% at 2 hours at room temperature and physically compatible in polyolefin or glass container with no amiodarone loss at 24 hours at room temperature.
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Variable |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Dobutamine HCl |
|
Lidocaine HCl |
|
Potassium chloride |
|
Procainamide HCl |
|
Verapamil HCl |
|
Variable |
|
Furosemide |
|
Quinidine gluconate |
|
Compatible |
|---|
|
Amikacin sulfate |
|
Amphotericin B |
|
Atracurium besylate |
|
Atropine sulfate |
|
Calcium chloride |
|
Calcium gluconate |
|
Caspofungin acetate |
|
Ceftaroline fosamil |
|
Ceftriaxone sodium |
|
Cefuroxime sodium |
|
Ciprofloxacin |
|
Clindamycin phosphate |
|
Dexmedetomidine HCl |
|
Dobutamine HCl |
|
Dopamine HCl |
|
Doripenem |
|
Doxycycline hyclate |
|
Epinephrine HCl |
|
Eptifibatide |
|
Erythromycin lactobionate |
|
Esmolol HCl |
|
Famotidine |
|
Fenoldopam mesylate |
|
Fentanyl citrate |
|
Fluconazole |
|
Gentamicin sulfate |
|
Hetastarch in lactated electrolyte injection (Hextend) |
|
Insulin, regular |
|
Isoproterenol HCl |
|
Labetalol HCl |
|
Lepirudin |
|
Lidocaine HCl |
|
Lorazepam |
|
Methylprednisolone sodium succinate |
|
Metoprolol tartrate |
|
Midazolam HCl |
|
Milrinone lactate |
|
Morphine sulfate |
|
Nesiritide |
|
Nitroglycerin |
|
Norepinephrine bitartrate |
|
Penicillin G potassium |
|
Phentolamine mesylate |
|
Phenylephrine HCl |
|
Potassium chloride |
|
Procainamide HCl |
|
Tirofiban HCl |
|
Tobramycin sulfate |
|
Vancomycin HCl |
|
Vasopressin |
|
Vecuronium bromide |
|
Incompatible |
|
Aminophylline |
|
Ampicillin sodium-sulbactam sodium |
|
Argatroban |
|
Bivalirudin |
|
Ceftazidime |
|
Digoxin |
|
Heparin sodium |
|
Imipenem-cilastatin sodium |
|
Micafungin sodium |
|
Piperacillin sodium-tazobactam |
|
Potassium phosphates |
|
Sodium bicarbonate |
|
Sodium phosphates |
|
Variable |
|
Cefazolin sodium |
|
Furosemide |
|
Magnesium sulfate |
|
Sodium nitroprusside |
Actions
-
Exhibits greater efficacy and a lower incidence of proarrhythmic effects than class I or other class III antiarrhythmic drugs.
-
Delays repolarization by prolonging the action potential duration and effective refractory period in cardiac tissue.
-
Inhibits transmembrane influx of extracellular sodium ions via fast sodium channels. Combines with fast sodium channels in their inactive state and inhibits recovery after repolarization in a time- and voltage-dependent manner.
-
Noncompetitively inhibits α- and β-adrenergic responses to sympathetic stimulation and catecholamine administration.
-
Depresses sinus node function and automaticity.
-
Relaxes cardiac and vascular smooth muscle, thereby dilating both systemic and coronary arteries.
-
Inhibits extrathyroidal deiodinases, resulting in decreased peripheral conversion of thyroxine (T4) to triiodothyronine (T3).
-
Contains 37.3% iodine; each 200-mg tablet or each mL of the injection contains approximately 75 or 18.7 mg of iodine, respectively.
-
Inhibits phospholipase (e.g., phospholipase A1, A2, and C) activity in vitro; production of amiodarone-phospholipid complexes within certain organs may be involved in the development of adverse effects.
-
Inhibits α-galactosidase activity.
Advice to Patients
-
Importance of patients taking medication exactly as prescribed. Importance of not taking a double dose to make up for a missed dose but instead taking the next scheduled dose.
-
Importance of not interrupting or discontinuing therapy without consulting a clinician, even if improvement is evident, as condition may worsen.
-
Importance of seeking medical attention immediately or proceeding to a hospital emergency department if too many oral doses are ingested.
-
If serious adverse effects occur, importance of informing a clinician before discontinuing the drug.
-
Importance of patients informing clinician of history of BP abnormalities, lung, liver, or thyroid disorders prior to treatment initiation.
-
Importance of clinicians informing patients of potential toxicities (e.g., lung, liver) that may occur during therapy.
-
Importance of patients informing clinician of any episodes of shortness of breath, wheezing, coughing, spitting up blood, chest pain, any other breathing disorders, or aggravation of cardiovascular disease.
-
Importance of patients informing clinician of symptoms of thyroid dysfunction such as weakness, weight gain or loss, heat or cold intolerance, hair thinning, sweating, menstrual cycle changes, swelling of the neck (goiter), nervousness, irritability, restlessness, decreased concentration, depression in geriatric patients, or tremor.
-
Importance of patients contacting their clinician if nausea or vomiting, dark urine, fatigue, yellowing of the skin or whites of eyes, or stomach pain occurs.
-
Importance of patients contacting their clinician if heart pounding, irregular heart beat, rapid or slow heartbeat, lightheadedness, or faintness occurs.
-
Importance of patients contacting their clinician if visual disturbances (e.g., blurred vision, visual halos, ocular photosensitivity) occur.
-
Importance of advising patients that most manufacturers of corneal refractive laser surgery devices consider the procedure to be contraindicated in patients receiving amiodarone.
-
Importance of regular laboratory monitoring (e.g., pulmonary, thyroid, and liver function) and clinical (e.g., cardiac, ophthalmologic) evaluation.
-
Importance of patients informing clinicians of existing or contemplated therapy, including prescription and OTC drugs, dietary supplements and/or herbal products, as well as any concomitant illnesses.
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed. Importance of avoiding pregnancy during therapy.
-
Importance of using sunscreen agents and protective clothing and of avoiding excessive exposure to sunlight or sun lamps.
-
Importance of taking amiodarone in a consistent manner relative to food intake.
-
Importance of not consuming grapefruit juice during oral amiodarone therapy.
-
Importance of advising patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
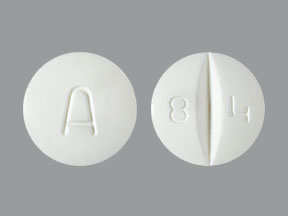
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
100 mg |
Pacerone |
Upsher-Smith |
|
200 mg* |
Amiodarone Hydrochloride Tablets |
|||
|
Cordarone (scored) |
Wyeth |
|||
|
Pacerone (scored) |
Upsher-Smith |
|||
|
400 mg* |
Amiodarone Hydrochloride Tablets |
|||
|
Pacerone (scored) |
Upsher-Smith |
|||
|
Parenteral |
Concentrate for injection, for IV infusion |
50 mg/mL* |
Amiodarone Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about amiodarone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (96)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
Patient resources
Professional resources
Other brands
Pacerone, Cordarone, Nexterone