Amiodarone Hydrochloride (Monograph)
Brand names: Cordarone, Pacerone
Drug class: Class III Antiarrhythmics
Introduction
Class III antiarrhythmic agent;1 2 4 5 8 12 17 18 21 24 25 26 28 31 38 355 also exhibits activity in each of the 4 Vaughn-Williams antiarrhythmic classes, including some class I (membrane-stabilizing) antiarrhythmic action.5 7 8 21 25 32 35 44 46 355 364
Uses for Amiodarone Hydrochloride
Ventricular Arrhythmias
Treatment to suppress or prevent the recurrence of documented life-threatening ventricular arrhythmias (e.g., recurrent VF; recurrent, hemodynamically unstable VT) that do not respond to documented adequate dosages of other currently available antiarrhythmic agents or when alternative antiarrhythmic agents are not tolerated.1 3 355 364
Used during cardiac arrest for treatment of refractory (i.e., unresponsive to CPR, defibrillation, and a vasopressor [e.g., epinephrine]) VF or pulseless VT.500 501 Considered the preferred antiarrhythmic drug for this use in current ACLS guidelines in adults; lidocaine may be used as an alternative.500 501 In pediatric patients, current evidence supports use of either amiodarone or lidocaine.502
Also may be used for treatment of wide-complex tachycardias during periarrest period; included in current ACLS guidelines for both adult and pediatric tachycardia.500 501 503
Treatment of sustained monomorphic VT not associated with angina, pulmonary edema, or hypotension† [off-label],364 442 or hemodynamically stable monomorphic VT† [off-label] .501
Treatment of polymorphic (irregular) VT† [off-label] associated with myocardial ischemia in the absence of QT interval prolongation.501
Has been used for primary prevention† [off-label] of sustained VT (i.e., VT lasting >30 seconds and/or associated with hemodynamic compromise),364 VF, or sudden cardiac death in patients with nonsustained ventricular arrhythmia following MI.344 368 370 384 394
Has been used in a limited number of patients for life-threatening ventricular arrhythmias associated with post-infarction aneurysm† [off-label] or with chronic myocarditis induced by Chagas’ disease† .26 72 172
Supraventricular Tachyarrhythmias
Used for suppression and prevention of various supraventricular tachycardias (SVTs)†.3 4 5 9 10 12 25 26 27 35 62 66 71 72 92 109 110 111 113 116 119 120 122 125 126 402 501 701
Because of higher risk of toxicity and proarrhythmic effects, antiarrhythmic agents generally reserved for patients who do not respond to or cannot be treated with AV nodal blocking agents (β-adrenergic blocking agents, diltiazem, verapamil).501 700
Some experts state amiodarone may be useful when ventricular rate control is needed but AV nodal blocking agents are contraindicated (e.g., patients with preexcited atrial arrhythmias associated with an accessory pathway†).501 701
May be effective for conversion of atrial fibrillation† to normal sinus rhythm (i.e., rhythm control); however, other antiarrhythmic agents (e.g., flecainide, dofetilide, propafenone, ibutilide) are preferred.701
Used to maintain sinus rhythm in patients with atrial fibrillation or flutter†.4 5 9 10 12 25 26 27 35 62 66 71 72 92 109 110 111 113 116 119 120 122 700 701
Termination of paroxysmal supraventricular tachycardia (PSVT)†, including atrioventricular nodal reentrant tachycardia (AVNRT) and atrioventricular reentrant tachycardia (AVRT) (e.g., Wolff-Parkinson-White syndrome); generally reserved for use when other therapies are ineffective or contraindicated.9 38 48 501 700 Avoid IV use in patients with Wolff-Parkinson-White syndrome who have preexcited atrial fibrillation; may accelerate ventricular rate and potentially cause life-threatening ventricular arrhythmias.701
Also used for long-term prevention of PSVT†,4 5 8 9 25 26 27 28 29 37 39 41 47 48 66 71 72 109 110 112 113 122 128 318 including those refractory to other antiarrhythmic agents.5 26 27 39 66 71 110 113 122 128 318
Has been used in the treatment of atrial tachycardia†.700
Has been effective in the prevention of supraventricular arrhythmias associated with bradycardia-tachycardia syndrome†.4 9 25 110 129 130 131
Angina
Has been used in treatment of chronic stable angina pectoris† and Prinzmetal variant angina†; because of potential toxicity, generally not considered a first-line agent but may have beneficial antianginal effect in patients receiving the drug for the management of arrhythmias.17 50 133 134 229
Hypertrophic Cardiomyopathy
Has been used in the management of ventricular and supraventricular arrhythmias associated with hypertrophic cardiomyopathy†.25 258 259 278 292
Amiodarone Hydrochloride Dosage and Administration
General
-
Administer lowest effective dosage to minimize the risk and occurrence of adverse effects.1
-
Adjust dosage carefully according to individual requirements and response and the general condition and cardiovascular status of the patient.1 355 Adjustment of maintenance dosage is difficult due to variable absorption and elimination of amiodarone; dosage reduction or temporary withdrawal or discontinuance of the drug may be required.1 284
-
When dosage adjustment is necessary, close monitoring for an extended period of time is recommended.1 355
-
Clinical and ECG monitoring of cardiac function, including appropriate ambulatory ECG monitoring (e.g., Holter monitoring) and/or programmed electrical stimulation (PES), as appropriate, is recommended.1
-
Monitor plasma amiodarone concentrations if patient does not respond or experiences unexpectedly severe toxicity.1 2 3 5 25 35 62 63 64 70 71 75 81
-
When initiating therapy in patients receiving other antiarrhythmic agents, attempt to gradually discontinue the other antiarrhythmic agents.1
Administration
Administer orally or by IV infusion.1 3 9 10 25 35 355
Also has been administered via intraosseous (IO) injection† during cardiac resuscitation.501
Oral Administration
Usually administered once daily.1 3 Administer in divided doses (e.g., twice daily) with meals when dosages ≥1 g daily are administered (e.g., during the loading-dose phase of therapy) or when intolerable adverse GI effects occur.1 3
Administer in a consistent manner relative to food intake.1
Administration of a loading-dose phase of therapy is required for the management of life-threatening ventricular arrhythmias;1 2 3 5 23 25 35 42 59 64 68 72 73 administer oral loading dose in hospital setting and monitor closely until risk of recurrent VT or VF has abated.1 35
Extemporaneous Oral Suspension
Extemporaneous oral suspensions of amiodarone have been prepared using the tablets and a commercially available vehicle.463 464
Standardize 4 Safety
Standardized concentrations for an extemporaneously prepared oral suspension of amiodarone have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care.462 Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label.462 For additional information on S4S (including updates that may be available), see [Web]
|
Concentration Standards |
|---|
|
5 mg/mL 20 mg/mL for doses of 75 mg or greater |
Amiodarone needs to have a pH very close to 8 to assure particle consistency
IV Administration
IV therapy may be used for acute antiarrhythmic therapy until cardiac rhythm is stabilized and oral therapy can be initiated.355 IV therapy may be required for 48–96 hours, but may be administered safely for longer periods.355 Experience with IV administration of amiodarone exceeding 3 weeks is limited.355
Administer in 3-phase sequence: rapid loading phase, slow loading phase, and maintenance infusion phase.355
Dilute amiodarone hydrochloride concentrate prior to administration by IV infusion.355
Administer solutions containing an amiodarone hydrochloride concentration >2 mg/mL via central venous catheter.355
Use in-line filter.355
Amiodarone hydrochloride infusions exceeding 2 hours should be administered in 5% dextrose in glass or polyolefin containers .355 Manufacturer recommends using PVC tubing (used in clinical studies).355 Leaching of plasticizer diethylhexylphthalate (DEHP) from IV tubing may occur.355
Standardize 4 Safety
Standardized concentrations for IV amiodarone have been established through Standardize 4 Safety (S4S), a national patient safety initiative to reduce medication errors, especially during transitions of care.460 461 Multidisciplinary expert panels were convened to determine recommended standard concentrations.460 461 Because recommendations from the S4S panels may differ from the manufacturer’s prescribing information, caution is advised when using concentrations that differ from labeling, particularly when using rate information from the label.460 461 For additional information on S4S (including updates that may be available), see [Web].460 461
Dosing units differ from concentration units
|
Patient Population |
Concentration Standards |
Dosing Units |
|---|---|---|
|
Adults |
1.8 mg/mL |
mg/min |
|
Pediatric patients (<50 kg) |
1.8 mg/mL |
mcg/kg/min |
|
3.6 mg/mL |
Dilution
For the first rapid loading infusion or for supplemental infusions, add 3 mL of amiodarone hydrochloride concentrate to 100 mL of 5% dextrose, resulting in a final concentration of 1.5 mg/mL.355
For the slow loading infusion and maintenance infusion, add 18 mL of amiodarone hydrochloride concentrate to 500 mL of 5% dextrose, resulting in a final concentration of 1.8 mg/mL.355 For subsequent maintenance infusions, solutions containing a final amiodarone hydrochloride concentration of 1–6 mg/mL may be used.355
Rate of Administration
For treatment of ventricular arrhythmias in adults, 15 mg/minute for 10 minutes (rapid loading phase), then 1 mg/minute for 6 hours (slow loading phase), then 0.5 mg/minute (initial maintenance phase) for 18 hours;355 infuse supplemental doses of 150 mg over 10 minutes (at a rate of 15 mg/minute).355 364 Initial (rapid) loading infusion rate should not exceed 30 mg/minute.355 364 397 Monitor initial rate of infusion closely; do not exceed recommended rate.355
Use volumetric infusion pump.355 Do not use drop-counter infusion sets; may result in underdosage.355
Dosage
Available as amiodarone hydrochloride; dosage expressed in terms of the salt.1 355
Pediatric Patients
Ventricular Arrhythmias†
Oral
Pediatric dosage has not been established; dosage may vary considerably.201 280 281 Some clinicians have recommended loading dosages of 10–15 mg/kg daily40 242 or 600–800 mg/1.73 m2 daily9 69 189 242 for approximately 4–14 days40 69 189 242 and/or until adequate control of cardiac arrhythmias is achieved or adverse effects become prominent.40 242 Subsequently, reduce dosage to 5 mg/kg daily40 242 or 200–400 mg/1.73 m2 daily9 69 189 242 for several weeks; if possible, reduce dosage to the lowest effective level.69 189 242
Children <1 year of age may require higher oral loading and maintenance dosages than older children when dosage is calculated on the basis of body weight, but not on the basis of body surface area†.280 282
Pediatric Resuscitation
IV or IO†Refractory VF or pulseless VT: 5 mg/kg as a rapid bolus.502 503 May repeat twice up to 15 mg/kg (maximum single dose of 300 mg).502 503
To minimize pediatric exposure to DEHP,408 may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).416
Wide-complex Tachycardias in Patients Not in Cardiac Arrest
IV5 mg/kg over 20–60 minutes (depending on urgency).503
To minimize pediatric exposure to DEHP,408 may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).416
Supraventricular Arrhythmias†
Oral
Pediatric dosage has not been established; dosage may vary considerably.201 280 281 Some clinicians have recommended loading dosages of 10–15 mg/kg daily40 242 or 600–800 mg/1.73m2 daily9 69 189 242 for approximately 4–14 days40 69 189 242 and/or until adequate control of cardiac arrhythmias is achieved or adverse effects become prominent.40 242 Subsequently, reduce dosage to 5 mg/kg daily40 242 or 200–400 mg/1.73 m2 daily9 69 189 242 for several weeks; if possible, reduce dosage to the lowest effective level.69 189 242
Children <1 year of age may require higher oral loading and maintenance dosages than older children when dosage is calculated on the basis of body weight, but not on the basis of body surface area.†280 282
IV
5 mg/kg over 20–60 minutes depending on urgency.503
To minimize pediatric exposure to DEHP,408 may infuse a loading dose of 5 mg/kg given in 5 divided doses of 1 mg/kg (each dose infused over 5–10 minutes).416
Adults
Ventricular Arrhythmias
Oral
|
Loading Dose |
800–1600 mg daily for 1–3 weeks or until initial therapeutic response occurs1 |
|
Dosage Adjustment |
When adequate control of ventricular arrhythmias is achieved or adverse effects become prominent, decrease dosage to 600–800 mg daily for about 1 month1 3 284 |
|
Maintenance Dosage |
400–600 mg daily;1 3 284 if possible, cautiously reduce dosage to 200 mg daily70 284 |
Consult published protocols for specific information about oral loading doses >1600 mg daily35 64 73 301 or IV loading-dose regimens† 64 250 followed by oral therapy.301 If an IV loading-dose regimen is used, initiate oral therapy as soon as possible after an adequate response is obtained and gradually eliminate IV amiodarone.301
IV
Total initial dosage during first 24 hours is approximately 1000 mg.355
|
Loading Phase |
Initial rapid loading phase: 150 mg administered at rate of 15 mg/minute (i.e., over 10 minutes) 355 364 |
|
Followed by slow loading phase: 360 mg administered at rate of 1 mg/minute (i.e., over 6 hours)355 364 397 |
|
|
Maintenance Phase |
First maintenance phase: 540 mg administered at rate of 0.5 mg/minute (i.e., over 18 hours)355 364 397 |
|
Maintenance Phase |
0.5 mg/minute (i.e., 720 mg over 24 hours); can be administered for 2–3 weeks 355 |
|
Breakthrough Episodes of VF or Hemodynamically Unstable VT |
Supplemental infusion of 150 mg administered at rate of 15 mg/minute (i.e., over 10 minutes)355 |
IV/Oral
When switching from IV to oral therapy, oral dosage depends on dose and duration of IV therapy, as well as bioavailability of oral drug.355 When switching from IV to oral therapy, clinical monitoring is recommended, particularly for geriatric patients.355
Assuming 720-mg/day infusion (0.5 mg/minute)
IV amiodarone not intended for maintenance treatment
|
Duration of IV Therapy |
Initial Oral Daily Dosage |
|---|---|
|
<1 week |
800–1600 mg |
|
1–3 weeks |
600–800 mg |
|
>3 weeks |
400 mg |
ACLS
IV or IO†Refractory VF or pulseless VT: 300 mg by rapid IV/IO injection; may consider an additional dose of 150 mg.500 501
Supraventricular Arrhythmias†
IV
For acute treatment of SVT, 150 mg over 10 minutes.700 Follow with 1 mg/minute for 6 hours, then 0.5 mg/minute for remaining 18 hours or initiate oral dosing.700
Oral
For ongoing management of SVT, some experts recommend 400–600 mg daily (in divided doses) in adults for approximately 2–4 weeks, followed by a maintenance dosage of 100–200 mg daily.700
Consult published protocols for specific information about oral loading-dose regimens using higher dosages.
Atrial Fibrillation†
IV
When used for rate control in patients with atrial fibrillation, some experts recommend an initial IV dose of 300 mg over 1 hour, followed by 10–50 mg/hr over 24 hours.701
Oral
Usual maintenance dose is 100–200 mg daily.701
Long-term Management of Recurrent Atrial Fibrillation†
Oral
Initially, 10 mg/kg daily for 14 days, followed by 300 mg daily for 4 weeks, and then 200 mg daily.402
Prescribing Limits
Pediatric Patients
Ventricular Arrhythmias†
IV
Maximum single dose: 300 mg,502 503 up to a total dose of 15 mg/kg.h 502 503
Adults
Ventricular Arrhythmias
IV
Mean daily doses >2.1 g are associated with an increased risk of hypotension.355
Limited experience with IV administration of amiodarone for >3 weeks.355
Special Populations
Hepatic Impairment
Dosage reduction recommended in patients with substantial hepatic impairment.35 283 284
Renal Impairment
Routine dosage reduction not required.1 35
Geriatric Patients
Select dosage with caution, usually starting at low end of dosage range, because of possible age-related decrease in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy; however, dosage requirements generally similar in geriatric and younger adults.1 355
Use caution with high dosages due to increased susceptibility to drug-induced bradycardia and conduction disturbances.301
Cautions for Amiodarone Hydrochloride
Contraindications
-
Severe sinus node dysfunction resulting in marked sinus bradycardia (unless a functioning pacemaker is present).1 355
-
Second- or third-degree AV block (unless a functioning pacemaker is present).1 355
-
Bradycardia that has caused syncope (unless a functioning pacemaker is present).1
-
Known hypersensitivity to amiodarone or any ingredient in the formulation, including iodine.1 355
Warnings/Precautions
Warnings
Mortality
Potentially fatal toxicities and severe adverse effects;1 106 355 use principally for documented life-threatening ventricular arrhythmias.1
Amiodarone therapy should be administered only by physicians experienced in the management of life-threatening arrhythmias who have access to laboratory facilities necessary to adequately monitor efficacy and adverse effects, including continuous ECG monitoring and electrophysiologic techniques for evaluating the patient in both ambulatory and hospital settings.1 106 355
Pulmonary Effects
Possible acute-onset (days to weeks) pulmonary injury; findings may include pulmonary infiltrates and/or mass on radiograph, pulmonary alveolar hemorrhage, bronchospasm, wheezing, fever, dyspnea, cough, hemoptysis, or hypoxia, sometimes leading to respiratory failure and/or death.1 355
Potentially fatal pulmonary toxicity1 3 9 25 136 324 325 326 327 333 338 370 may result from pulmonary interstitial pneumonitis (or alveolitis) or hypersensitivity pneumonitis.1 325 326 338 339 345 346 Toxicity is usually reversible following discontinuance of the drug (with or without corticosteroid therapy).1 3 75 136 138 139 140 142 272 308 327 329 333 336 337 338 350
Baseline pulmonary function testing (prior to initiating therapy)1 25 325 326 327 328 335 338 and periodic (e.g., every 3–6 months) chest radiographs, clinical evaluation, and pulmonary function testing recommended.1 25 148 284 325 327 338
If hypersensitivity pneumonitis occurs, discontinue amiodarone and initiate corticosteroid therapy.1 350
If interstitial pneumonitis occurs, reduce dosage or discontinue therapy, especially if other acceptable antiarrhythmic therapies are available.1 326 327 328 333 338 Supportive treatment, including mechanical ventilation, may be required.136 140 142
Use with caution, if at all, in patients with preexisting pulmonary disease35 (e.g., chronic obstructive disease,252 reduced pulmonary diffusion capacity35 138 324 ); poorer prognosis if pulmonary toxicity develops in such patients.1
If new respiratory symptoms develop, consider the possibility of amiodarone-induced pulmonary toxicity; 1 136 140 326 327 clinical and radiographic evaluation, as well as scintigraphic and pulmonary function testing (including diffusion capacity), if necessary, are recommended.1 138 151 324 326 327 328 333 336 337 338 Carefully assess respiratory symptoms and rule out other causes of respiratory impairment (e.g., CHF, pulmonary embolism, malignancy, infectious causes) before discontinuing therapy.1 136 138 140 327 328 338
Bronchiolitis obliterans organizing pneumonia (possibly fatal) and pleuritis reported during postmarketing experience.1
Hepatic Effects
Possible liver function test abnormalities;1 3 9 10 25 30 75 83 108 141 153 154 157 158 159 163 355 abnormalities are usually minor,1 25 75 not accompanied by clinical symptoms,1 3 9 10 70 72 75 153 158 159 161 and generally return to normal following dosage reduction or discontinuance of the drug.9 72 75 141 154 159
Rarely, potentially fatal hepatic injury (i.e., clinical hepatitis, cholestatic hepatitis, hepatocellular necrosis, cirrhosis) 1 3 35 155 156 160 162 341 342 355 has occurred.1 3 25 35 155 156 158 160 161 162 163 164 355
Monitor serum hepatic enzyme concentrations at regular intervals.1 153 157 160 164 355 Reduce oral dosage, decrease IV infusion rate, or discontinue therapy if enzyme concentrations are >3 times normal values in patients with normal pretreatment values or twice baseline pretreatment values in patients with elevated pretreatment values or if hepatomegaly or progressive hepatic injury occurs.1 156 162 163 164 355
Possible acute centrolobular confluent hepatic necrosis during IV therapy; may be related to a much higher loading dose concentration and more rapid infusion rate than recommended.355 Closely monitor initial concentration and rate of IV infusion; do not exceed recommended initial drug concentration and infusion rate.355
Arrhythmogenic Effects
Possible worsening of existing arrhythmias1 3 9 10 25 35 75 132 141 175 287 355 or occurrence of new arrhythmias.1 35 166 167 168 175 176 355 Arrhythmogenic effects include progression of VT to VF,1 132 355 sustained VT,1 25 141 175 176 355 increased resistance to cardioversion,1 25 122 175 304 atrial fibrillation,355 nodal arrhythmia,355 and atypical VT (torsades de pointes).1 3 9 25 75 132 171 173 265 355
Monitor for QTc prolongation during IV infusion of amiodarone.355
If new signs of arrhythmia appear, consider possibility of hyperthyroidism.1 355
Chronic administration of antiarrhythmic drugs (e.g., amiodarone) in patients with an implanted cardiac device (e.g., defibrillator, pacemaker) may change electrical conduction properties of the heart and potentially affect pacing and/or defibrillating thresholds.1 Therefore, manufacturer recommends assessment to ensure appropriate device parameters before and during amiodarone therapy.1
Electrolyte Abnormalities
Electrolyte abnormalities (e.g., hypokalemia, hypomagnesemia) may increase arrhythmogenic effects.1 3 41 Evaluate patient for potassium or magnesium deficiency; if present, correct deficiency prior to initiation of therapy.1 249
Monitor electrolyte and acid-base balance in patients with severe or prolonged diarrhea and in patients receiving diuretics concomitantly.45 47 50 355
Effects on Cardiac Conduction
Possible AV, intraventricular,1 3 4 25 26 30 35 355 or SA block;168 SA node dysfunction (e.g., symptomatic sinus bradycardia),1 3 4 9 10 25 26 30 35 50 75 154 169 175 355 393 sinus arrest with suppression of escape foci);1 141 166 167 168 169 or bradycardia (usually associated with IV therapy).355
Administer IV amiodarone in a setting where a temporary pacemaker is available for patients with known predisposition to bradycardia or AV block.355
Ocular Effects
Optic neuropathy1 25 153 154 184 185 186 187 355 and/or optic neuritis may occur at any time during amiodarone therapy; usually results in visual impairment1 294 311 355 357 and may progress to permanent blindness.1 355 357
Baseline and routine (e.g., after the first 6 months and then annually and/or as necessary) ophthalmologic examinations recommended, including slit-lamp and funduscopic tests.1 25 31 355 431
Careful monitoring recommended for patients experiencing visual disturbances or those receiving long-term therapy.1 186 188 If visual impairment occurs (e.g., changes in visual acuity, decreases in peripheral vision), prompt ophthalmologic examination recommended.1 355 357
If optic neuropathy and/or optic neuritis develops, reevaluate therapy; consider risks and complications against the possible benefits of antiarrhythmic therapy.1 355
Thyroid Effects
Thyroid nodules or thyroid cancer reported during postmarketing experience, sometimes accompanied by hyperthyroidism.1 355
Possible altered thyroid function test results:1 4 9 10 25 35 83 153 154 230 231 232 233 234 235 236 237 238 239 240 253 355 374 385 increased serum thyroxine (T4) and reverse triiodothyronine (rT3) concentrations, decreased serum T3 concentrations.1 4 9 10 25 35 83 153 230 231 232 233 234 235 237 253 283 355 393
Possible hypothyroidism or hyperthyroidism.1 3 4 9 10 25 26 70 83 153 154 230 231 233 234 235 236 237 238 239 240 253 370 374 355 393 Amiodarone-induced hyperthyroidism may result in thyrotoxicosis and/or arrhythmia breakthrough or aggravation; fatalities have occurred.1 355
Thyroid function tests recommended prior to initiating therapy and at periodic intervals (approximately every 3–6 months) thereafter,1 25 35 231 234 235 236 237 253 355 particularly in geriatric patients1 283 355 and/or in patients with a history of thyroid nodules, goiter, or other thyroid dysfunction.1 4 234 237 283 355
If hypothyroidism occurs, reduce amiodarone dosage1 25 154 283 355 and/or carefully supplement with thyroid agents if necessary;1 25 72 83 153 154 230 231 235 283 355 374 discontinuance of amiodarone may be required.1 231 283 344 355 368 374
If hyperthyroidism occurs, aggressive therapy (including dosage reduction or discontinuance of amiodarone) is indicated, since clinical manifestations (i.e., cardiac arrhythmias) may be potentially serious and may be fatal.1 72 153 154 230 253 283 344 355 368 374 Antithyroid drugs, adrenergic blockers, and/or temporary corticosteroid therapy may be necessary.1 355 However, antithyroid agents appear to be of limited benefit when used alone, since high intrathyroidal iodine stores (typically observed in patients receiving long-term amiodarone therapy)1 238 239 355 445 antagonize the inhibitory effects of antithyroid drugs on thyroidal iodine utilization.446 Radioactive iodine treatment contraindicated because of low radioiodine uptake in amiodarone-associated hyperthyroidism.1 355 In patients in whom aggressive treatment of amiodarone-induced toxicity has failed or the drug cannot be discontinued because it is the only drug effective against the resistant arrhythmia, thyroidectomy may be an option.1 355 However, experience with surgical management is limited and such treatment could induce thyroid storm; therefore, careful surgical and anesthetic management is required.1 355
Fetal/Neonatal Morbidity
Possible adverse effects on fetal thyroid function and overall development.25 35 89 91 Possible congenital goiter/hypothyroidism and hyperthyroidism.1 330 354 355 Women should avoid becoming pregnant during amiodarone therapy.431 Use during pregnancy only when the potential benefits justify the possible risks to the fetus.1 88 89 355 If amiodarone is used during pregnancy or the patient becomes pregnant while taking the drug, apprise patient of potential hazard to fetus.1 355
Hypotension
Hypotension associated with IV therapy;355 mean daily IV dosages >2.1 g associated with increased risk of hypotension.355 Hypotension may be refractory in some cases, resulting in death.1 355 Monitor initial rate of infusion closely; do not exceed recommended rate. 355
Hypotension (possibly severe) reported during open-heart surgery (during and/or following cardiopulmonary bypass) in amiodarone-treated patients.1 170 216 267
Arrhythmia Recurrence
Possible recurrence of life-threatening arrhythmias after dosage reduction or discontinuance of therapy; time to recurrence may range from weeks to months.1 Prolonged hospitalization1 35 or intensive ambulatory monitoring (e.g., via telemetric ECG),284 possibly with periodic determination of plasma amiodarone concentrations, may be required.35
Sensitivity Reactions
Hypersensitivity Reactions
Possible hypersensitivity pneumonitis.1 326 330 338 346 If hypersensitivity pneumonitis occurs, initiate corticosteroid therapy and discontinue amiodarone.1 350 Rechallenge may result in more rapid and more severe adverse effects than rechallenge with amiodarone in patients with interstitial pneumonitis.1
Anaphylactic/anaphylactoid reaction (including shock) and angioedema reported during postmarketing experience.1 355
Dermatologic Reactions
Possible photosensitivity.1 70 72 153 373 Reactions generally begin within 2 hours of exposure to sunlight 9 153 190 195 and last for 1–3 days;190 195 may last a week in severe cases.190 Reactions may occur up to 4 months following discontinuance of the drug.9 140
Possible pigmentary changes (blue-gray discoloration) to exposed areas of the body (e.g., face, hands) in patients receiving long-term therapy,1 3 9 25 30 35 108 153 154 190 191 192 193 196 385 in patients with fair complexions,1 or following excessive exposure to sunlight.1 9 25 35 153 191 193 Usually slowly reversible following discontinuance of the drug.1 191
Sunscreen agents,1 25 35 72 153 190 195 283 protective clothing,1 35 190 195 and avoidance of excessive exposure to sunlight25 35 190 are recommended.1 25 35 190 195
Toxic epidermal necrolysis (sometimes fatal), erythema multiforme, Stevens-Johnson syndrome, exfoliative dermatitis, skin cancer, and pruritus reported during postmarketing experience.1 355
General Precautions
Ocular Effects
Corneal microdeposits occur in almost all patients.1 3 9 25 35 70 72 75 141 153 176 185 186 187 393 Usually not associated with visual disturbances;1 9 35 185 however, halo vision,1 25 70 73 75 141 153 154 175 176 184 187 188 blurred vision,1 3 10 25 154 185 188 photophobia,1 25 75 176 184 187 and dry eyes may occur.1 175 176
Corneal deposits are related to dosage and duration of therapy.9 25 72 153 183 185 186 Reversible following dosage reduction or discontinuance of therapy.1 9 25 56 70 72 153 154 185 186 187 Asymptomatic, nonprogressive deposits do not necessitate dosage reduction or drug discontinuance.1 284
Routine ophthalmologic examinations, including slit-lamp and funduscopic tests, recommended.1 355
Most manufacturers of corneal refractive laser surgery devices consider the procedure to be contraindicated in patients receiving amiodarone.1 355
Nervous System Effects
Possible peripheral neuropathy 1 3 9 25 35 72 75 162 176 177 178 179 180 268 and proximal myopathy.3 9 25 75 153 162 176 177 268
Delirium, hallucination, confusional state, pseudotumor cerebri, disorientation, and parkinsonian symptoms (e.g., akinesia, bradykinesia) reported during postmarketing experience.1
Cardiac Failure
Possible new or worsened heart failure;1 9 25 35 70 75 108 299 355 rarely requires discontinuance of the drug.1
Pulmonary Precautions
Possible ARDS following cardiothoracic or other surgery.1 309 334 355 Closely monitor forced inspiratory oxygen and tissue oxygenation.1 355 Preoperative pulmonary function testing recommended for patients undergoing cardiothoracic surgery.309
Symptomatic Bradycardia in Patients Receiving HCV Treatment
Symptomatic bradycardia, including cases requiring pacemaker intervention, reported in patients receiving amiodarone concomitantly with an HCV treatment regimen containing sofosbuvir in conjunction with another HCV direct-acting antiviral (DAA), including ledipasvir, simeprevir, or daclatasvir.453 454 455 456 457 Fatal cardiac arrest reported in a patient receiving amiodarone concomitantly with fixed combination of ledipasvir and sofosbuvir (ledipasvir/sofosbuvir).453 454 455 456 457
In most reported cases, bradycardia occurred within hours to days after HCV treatment initiated in patients receiving amiodarone (also has been observed up to 2 weeks after initiation of HCV treatment) and resolved after HCV treatment discontinued.454 455 456 457 Mechanism for this adverse cardiovascular effect unknown.453 454 455 456 457
Patients who may be at increased risk for symptomatic bradycardia if amiodarone used concomitantly with HCV treatment regimen containing sofosbuvir with another DAA include those also receiving a β-adrenergic blocking agent, those with underlying cardiac comorbidities, and/or those with advanced liver disease.454 455 456 457
Concomitant use of amiodarone with HCV treatment regimen containing sofosbuvir with another DAA not recommended.454 455 456 457
If there are no alternative HCV treatment options and regimen of sofosbuvir with another DAA must be used in a patient receiving amiodarone, advise patient about the risk of serious symptomatic bradycardia before initiating HCV treatment.454 455 456 457 Perform cardiac monitoring in an inpatient setting during first 48 hours of concomitant use of amiodarone and regimen of sofosbuvir with another DAA;454 455 456 457 subsequently, perform heart rate monitoring daily (outpatient or self-monitoring) through at least the first 2 weeks of concomitant use.454 455 456 457 Similar cardiac monitoring recommended in patients who discontinued amiodarone just prior to initiation of regimen of sofosbuvir with another DAA or if alternative antiarrhythmic agent cannot be used and amiodarone must be initiated in a patient already receiving regimen of sofosbuvir with another DAA.454 455 456 457
Advise patients receiving amiodarone concomitantly with regimen of sofosbuvir with another DAA to immediately contact a clinician if signs or symptoms of bradycardia (e.g., near-fainting or fainting, dizziness or lightheadedness, malaise, weakness, excessive tiredness, shortness of breath, chest pain, confusion, memory problems) develop.454 455 456 457
Specific Populations
Pregnancy
Lactation
Amiodarone and desethylamiodarone are distributed into milk.1 2 78 89 91 355 Discontinue nursing.1 91 355
Pediatric Use
Safety and efficacy not established;1 355 however, amiodarone has been used in children.35 40 69 189 280 281 282 502 503
Large amounts of benzyl alcohol (e.g., 100–400 mg/kg daily) have been associated with toxicity in neonates;355 408 409 410 411 412 413 414 each mL of amiodarone hydrochloride injection contains 20.2 mg of benzyl alcohol.355
Amiodarone hydrochloride injection leaches DEHP plasticizer from IV tubing;355 408 exposure to DEHP may adversely affect male reproductive tract development during fetal, infant, and toddler stages of development.408 415 Consider dosing methods to reduce potential exposure to DEHP.408
Geriatric Use
Response similar to that in younger adults.1 355
Possible increased susceptibility to bradycardia and conduction disturbances.301
Possible thyroid effects.283
Select dosage with caution, usually starting at low end of dosage range, because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.1 355
Hepatic Impairment
Effects of hepatic impairment on amiodarone elimination have not been evaluated;1 2 35 however, amiodarone is extensively metabolized,9 25 76 80 101 probably in the liver.9 35 64 76 81 Consider dosage reduction in patients with substantial hepatic impairment.35 283 284
Renal Impairment
Possible excessive accumulation of iodine and possible resultant thyroid effects.284 314 315
Common Adverse Effects
IV administration: hypotension.355
Oral therapy: adverse nervous system (e.g., malaise and fatigue,1 tremor and/or involuntary movements,1 3 9 10 25 70 75 153 175 178 180 268 lack of coordination,1 abnormal gait and/or ataxia,1 3 9 75 154 175 176 178 180 268 dizziness,1 3 10 paresthesia1 9 10 70 75 175 176 177 178 179 ) and GI (e.g., nausea,1 3 9 25 70 75 141 153 154 175 176 vomiting,1 3 175 constipation,1 9 25 70 75 141 153 154 175 176 anorexia1 3 9 25 70 75 141 153 176 ) effects.
Drug Interactions
Metabolized by CYP3A4 and CYP2C8.1 355
Elimination half-life of amiodarone is long and variable; potential for interactions exists with drugs administered after discontinuance of amiodarone therapy.1 35 208 215 355
Drugs, Foods, and Dietary or Herbal Supplements Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with substrates, inhibitors, or inducers of CYP3A4 are likely.1 355 Inhibits CYP isoenzymes 1A2, 2C9, 2D6, and 3A4;1 355 potential pharmacokinetic interaction with drugs metabolized by these isoenzymes (increased plasma concentrations).1 355 Amiodarone is a substrate for CYP3A4 and CYP2C8; drugs and other substances that inhibit these isoenzymes may decrease metabolism and increase serum concentrations of amiodarone.1 355
Drugs with P-Glycoprotein-Mediated Clearance
Amiodarone inhibits the P-glycoprotein transport system, which may result in unexpectedly high plasma concentrations of drugs that are substrates for this transport system.1 355
Drugs Affecting QT Interval
Potential pharmacodynamic interaction (additive effects on the QTc interval).1 355 433
Antiarrhythmic Agents
Cautious use and close monitoring for possible adverse effects recommended if amiodarone is used concomitantly with other antiarrhythmic agents,1 355 particularly class IA antiarrhythmic agents.207 228 255 264 265 266
Reserve concomitant use for the management of life-threatening arrhythmias unresponsive to monotherapy.1 355
In general, reduce dosage of other antiarrhythmic agent(s) by 30–50% several days after initiating amiodarone therapy;1 355 assess necessity of continuing the other antiarrhythmic agent(s) after antiarrhythmic effect of amiodarone has been established.1 355
In patients already receiving amiodarone, reduce initial dosage of other antiarrhythmic agent(s) by approximately 50%.1 355
Specific Drugs, Foods, and Dietary or Herbal Supplements
|
Drug, Food, or Supplement |
Interaction |
Comments |
|---|---|---|
|
Agalsidase beta |
Theoretical risk of inhibited intracellular α-galactosidase activity439 |
Some clinicians recommend avoidance of concurrent use of biosynthetic forms of α-galactosidase and amiodarone439 |
|
Anesthetics, general |
Potential serious cardiovascular (e.g., hypotension) and cardiac (e.g., sinus bradyarrhythmias, AV block) effects1 167 170 216 267 |
|
|
Anticoagulants, oral |
Decreased warfarin clearance; 203 204 207 208 316 increased PT in almost all patients.1 203 208 210 301 316 355 390 Can result in serious or fatal hemorrhage1 203 204 207 208 209 211 212 214 316 355 |
Reduce anticoagulant dosage by 33–50% when initiating amiodarone1 204 207 209 214 283 355 Frequent PT determinations and close observation for adverse effects recommended; adjust anticoagulant dosage as necessary1 203 204 207 209 316 390 355 PT may not return to normal for 1–4 months following discontinuance of amiodarone203 204 207 209 210 316 390 |
|
Azole antifungals |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) reported1 355 432 |
|
|
β-adrenergic blocking agents (e.g., propranolol) |
Possible potentiation of sinus bradycardia, sinus arrest, and AV block1 25 263 355 |
Concomitant therapy may be considered in patients with severe sinus bradycardia or sinus arrest following insertion of artificial pacemaker;1 355 monitor cardiac function432 |
|
Calcium-channel blocking agents (e.g., diltiazem, verapamil) |
Possible potentiation of sinus bradycardia, sinus arrest, and AV block1 35 256 301 355 |
Concomitant therapy may be considered in patients with severe sinus bradycardia or sinus arrest following insertion of artificial pacemaker1 355 |
|
Cardiac glycosides |
Increased serum digoxin concentrations and digoxin toxicity1 9 25 35 203 204 207 217 218 219 220 221 222 223 301 355 |
When initiating amiodarone therapy, reassess need for continued cardiac glycoside therapy; discontinue digoxin or reduce digoxin dosage by 50%1 25 35 207 217 223 355 Monitor serum digoxin concentrations carefully and reduce digoxin dosage as necessary1 9 35 204 218 219 222 223 355 432 Close observation for signs of cardiac glycoside toxicity recommended 1 9 204 218 355 Monitor thyroid function carefully due to potential for altered cardiac glycoside sensitivity in patients with amiodarone-induced changes in thyroid function218 224 225 |
|
Cholestyramine |
Decreased plasma amiodarone concentrations and half-life1 203 262 355 |
|
|
Cimetidine |
||
|
Cisapride (no longer commercially available in the US) |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes) reported432 |
Concurrent use contraindicated432 |
|
Clopidogrel |
Potential interaction resulting in ineffective inhibition of platelet aggregation by clopidogrel1 355 |
|
|
Cyclosporine |
Increased plasma cyclosporine concentrations resulting in elevated serum creatinine concentrations1 355 |
|
|
Dextromethorphan |
Possible inhibition of dextromethorphan metabolism with prolonged administration (>2 weeks) of oral amiodarone1 355 |
|
|
Disopyramide |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes)1 355 |
|
|
Dolasetron |
Use concomitantly with caution; monitor cardiac function432 438 |
|
|
Fentanyl |
Possible hypotension, bradycardia, and decreased cardiac output1 355 |
|
|
Flecainide |
Decreased flecainide clearance226 |
Reduce flecainide dosage by 30–50% several days after initiating amiodarone therapy1 226 355 Monitor patient and plasma flecainide concentrations closely; adjust flecainide dosage as necessary1 226 320 355 |
|
Fluoroquinolone anti-infectives (e.g., ciprofloxacin, gemifloxacin, levofloxacin, moxifloxacin) |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes)1 355 432 |
|
|
Grapefruit juice |
||
|
Halofantrine (no longer commercially available in the US) |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes)444 |
Avoid concomitant use444 |
|
HCV antivirals |
Regimen containing sofosbuvir with another DAA (e.g., ledipasvir, simeprevir, daclatasvir): May result in serious symptomatic bradycardia (mechanism unknown);453 454 455 456 457 effect on plasma concentrations of the drugs is unknown454 455 456 457 Simeprevir-containing regimen that does not include sofosbuvir: Modestly increased plasma concentrations of oral amiodarone due to intestinal CYP3A4 inhibition by simeprevir456 Fixed combination of ombitasvir, paritaprevir, and ritonavir (ombitasvir/paritaprevir/ritonavir) with dasabuvir: Increased plasma concentrations of amiodarone458 |
Regimen containing sofosbuvir with another DAA: Concomitant use not recommended;454 455 456 457 if concomitant use necessary, patient counseling and cardiac monitoring required454 455 456 457 Simeprevir-containing regimen that does not include sofosbuvir: Use concomitantly with caution;456 amiodarone therapeutic drug monitoring recommended, if available456 Ombitasvir/paritaprevir/ritonavir with dasabuvir: Use concomitantly with caution;458 amiodarone therapeutic drug monitoring recommended, if available458 |
|
HIV protease inhibitors |
HIV protease inhibitors used with low-dose ritonavir (ritonavir-boosted) or without low-dose ritonavir (unboosted): Possible increased plasma concentrations of amiodarone and the HIV protease inhibitor1 200 355 |
Ritonavir-boosted saquinavir or ritonavir-boosted tipranavir: Concomitant use not recommended200 Other ritonavir-boosted HIV protease inhibitors or unboosted HIV protease inhibitors: Use concomitantly with caution;200 monitor for amiodarone toxicity;200 consider monitoring ECG and amiodarone plasma concentrations200 |
|
HMG-CoA reductase inhibitors (statins) |
Increased risk of myopathy and/or rhabdomyolysis, particularly when used with higher dosages of certain statins (e.g., simvastatin)1 355 371 417 448 449 450 451 |
Reduce dosage of lovastatin (to ≤40 mg daily) or simvastatin (to ≤20 mg daily) during concomitant therapy with amiodarone371 417 448 |
|
Lidocaine |
Increased serum lidocaine concentrations; potential increase in adverse effects (e.g., sinus bradycardia, seizures)1 355 |
|
|
Loratadine |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes)1 355 |
|
|
Macrolide antibiotics |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes)1 355 |
|
|
Methotrexate |
Possible inhibition of methotrexate metabolism with prolonged administration (>2 weeks) of oral amiodarone1 355 |
|
|
Phenytoin |
Increased serum phenytoin concentrations;1 203 205 206 355 possible phenytoin toxicity (e.g., nystagmus, ataxia, lethargy)1 203 205 206 |
Monitor serum phenytoin concentrations and closely observe patient for signs of phenytoin toxicity; reduce phenytoin dosage as necessary1 205 |
|
Pimozide |
Additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes)433 |
Concomitant use contraindicated433 |
|
Procainamide |
Increased plasma procainamide and N-acetylprocainamide (NAPA) concentrations;1 203 227 possible increases in QTc and QRS intervals and acceleration of ventricular tachycardia313 |
Reduce procainamide dosage by 20–33% when amiodarone therapy is initiated or discontinue procainamide therapy1 227 313 355 |
|
Quinidine |
Increased serum quinidine concentrations;1 35 227 228 355 possible marked QT prolongation and torsades de pointes207 228 264 |
Reduce quinidine dosage by 33–50% when amiodarone therapy is initiated or discontinue quinidine therapy1 227 355 Monitor serum quinidine concentrations carefully and reduce quinidine dosage as necessary; observe patient closely for signs of toxicity, including QT prolongation1 227 228 355 |
|
Rifampin |
Decreased plasma amiodarone and desethylamiodarone concentrations1 355 |
|
|
St. John’s wort (Hypericum perforatum) |
||
|
Trazodone |
Additive effects in prolonging QTc interval; serious cardiac arrhythmias (e.g., torsades de pointes)1 355 |
|
|
Ziprasidone |
Possible additive effects in prolonging QTc interval; possible serious cardiac arrhythmias (e.g., torsades de pointes)437 |
Avoid concomitant use437 |
Amiodarone Hydrochloride Pharmacokinetics
Absorption
Bioavailability
Slowly1 2 10 25 35 40 49 55 58 59 61 62 65 78 79 80 81 99 and variably absorbed from the GI tract following oral administration;1 2 5 25 26 35 49 55 56 58 59 60 61 62 65 70 76 77 78 79 80 81 99 absolute bioavailability averages 50%1 25 55 58 59 60 61 78 79 80 355 (range: 22–86%).2 3 25 55 58 59 60 78 99 Considerable interindividual variation in plasma concentrations attained with a given dosage.1 5 56 60 70 75 Following oral administration, peak plasma concentrations usually occur within 3–7 hours.1 2 10 25 35 55 58 59 60 61 62 64 65 73 78 79 80 81 99
Onset
Following oral administration, onset of antiarrhythmic activity is highly variable;1 2 3 23 25 42 59 64 68 72 however, a therapeutic response generally is not evident until 1–3 weeks after beginning therapy, even when loading doses are administered.1 2 3 5 23 25 42 59 64 68 72
Duration
Antiarrhythmic effects generally persist for 10–150 days following withdrawal of long-term therapy;1 2 3 4 5 23 24 26 49 56 59 67 72 79 duration of antiarrhythmic activity is variable and unpredictable1 and appears to depend on length of therapy2 26 and type of arrhythmia.5 23
Food
Food increases rate and extent of absorption.1 283
Distribution
Extent
Following chronic oral administration, amiodarone and N-desethylamiodarone are distributed extensively into many body tissues and fluids.1 2 10 25 35 55 56 62 78 81 84 86 94 98 99 290 Tissue concentrations generally exceed concurrent plasma concentrations of the drug.2 10 35 55 62 78 82 84 85 After long-term therapy, concentrations of the metabolite usually are substantially higher than concentrations of unchanged drug in almost all tissues, except adipose tissue.2 5 35 55 78 81 82 84 86 99
Following IV administration, amiodarone is rapidly and widely distributed.85
Amiodarone and N-desethylamiodarone cross the placenta to a limited extent.1 2 78 88 89 91 355 Amiodarone and N-desethylamiodarone are distributed into milk.1 2 78 89 91 355
Plasma Protein Binding
Approximately 96%.1 2 87 90 355
Elimination
Metabolism
Extensively metabolized,9 25 76 80 101 probably in the liver9 35 64 76 81 and possibly in the intestinal lumen and/or GI mucosa,35 64 76 to at least one major metabolite,1 2 25 35 76 77 78 81 96 101 355 N-desethylamiodarone. This metabolite appears to possess substantial electrophysiologic and antiarrhythmic activity similar to amiodarone’s.1 86 99 100 101 273 285 355
Elimination Route
Excreted almost completely in feces as unchanged drug and N-desethylamiodarone, presumably via biliary elimination.1 3 9 25 35 59 77 78 80 95 98 355
Half-life
Half-life of amiodarone appears to be substantially more prolonged following multiple rather than single doses.2 4 9 26 55 58 59 64 65 78 81 99 291
Following a single IV dose, the terminal elimination phase half-life of amiodarone averages 25 days (range 9–47 days);2 5 55 355 elimination half-life of N-desethylamiodarone equals or exceeds that of amiodarone.355
Following chronic oral administration, amiodarone has an initial elimination half-life of about 2.5–10 days, followed by a terminal elimination half-life averaging 53 days;1 55 elimination half-life of N-desethylamiodarone averages 57–61 days.1 25 55 93 97 99 101
Clearance may be more rapid in pediatric patients.2 9 40 69
Clearance may be decreased in geriatric patients (>65 years of age).355
Stability
Storage
Oral
Tablets
Tightly sealed containers at 20–25°C; protect from light.1 443 The manufacturer of one commercially available amiodarone tablet preparation (Pacerone) states the tablets may be exposed to 15–30°C.443
Parenteral
Injection Concentrate
20–25°C; protect from light and excessive heat.355 Store ampuls in carton to protect from light until used.355 Light protection not necessary during administration.355 c
Compatibility
Parenteral
Do not use evacuated glass containers for amiodarone hydrochloride infusions (incompatibility with a buffer in the container may cause precipitation).c Polysorbate 80, a component of IV amiodarone injection, can cause leaching of diethylhexyl phthalate (DEHP) from IV tubing, including PVC tubing; leaching increases at lower than recommended flow rates and at higher than recommended infusion concentrations.355
Solution Compatibilityc
Manufacturer states physically compatible in PVC container with amiodarone loss of <10% at 2 hours at room temperature and physically compatible in polyolefin or glass container with no amiodarone loss at 24 hours at room temperature.c
|
Compatible |
|---|
|
Dextrose 5% in water |
|
Variable |
|
Sodium chloride 0.9% |
Drug Compatibility
|
Compatible |
|---|
|
Dobutamine HCl |
|
Lidocaine HCl |
|
Potassium chloride |
|
Procainamide HCl |
|
Verapamil HCl |
|
Variable |
|
Furosemide |
|
Quinidine gluconate |
|
Compatible |
|---|
|
Amikacin sulfate |
|
Amphotericin B |
|
Atracurium besylate |
|
Atropine sulfate |
|
Calcium chloride |
|
Calcium gluconate |
|
Caspofungin acetate |
|
Ceftaroline fosamil |
|
Ceftriaxone sodium |
|
Cefuroxime sodium |
|
Ciprofloxacin |
|
Clindamycin phosphate |
|
Dexmedetomidine HCl |
|
Dobutamine HCl |
|
Dopamine HCl |
|
Doripenem |
|
Doxycycline hyclate |
|
Epinephrine HCl |
|
Eptifibatide |
|
Erythromycin lactobionate |
|
Esmolol HCl |
|
Famotidine |
|
Fenoldopam mesylate |
|
Fentanyl citrate |
|
Fluconazole |
|
Gentamicin sulfate |
|
Hetastarch in lactated electrolyte injection (Hextend) |
|
Insulin, regular |
|
Isoproterenol HCl |
|
Labetalol HCl |
|
Lepirudin |
|
Lidocaine HCl |
|
Lorazepam |
|
Methylprednisolone sodium succinate |
|
Metoprolol tartrate |
|
Midazolam HCl |
|
Milrinone lactate |
|
Morphine sulfate |
|
Nesiritide |
|
Nitroglycerin |
|
Norepinephrine bitartrate |
|
Penicillin G potassium |
|
Phentolamine mesylate |
|
Phenylephrine HCl |
|
Potassium chloride |
|
Procainamide HCl |
|
Tirofiban HCl |
|
Tobramycin sulfate |
|
Vancomycin HCl |
|
Vasopressin |
|
Vecuronium bromide |
|
Incompatible |
|
Aminophylline |
|
Ampicillin sodium-sulbactam sodium |
|
Argatroban |
|
Bivalirudin |
|
Ceftazidime |
|
Digoxin |
|
Heparin sodium |
|
Imipenem-cilastatin sodium |
|
Micafungin sodium |
|
Piperacillin sodium-tazobactam |
|
Potassium phosphates |
|
Sodium bicarbonate |
|
Sodium phosphates |
|
Variable |
|
Cefazolin sodium |
|
Furosemide |
|
Magnesium sulfate |
|
Sodium nitroprusside |
Actions
-
Exhibits greater efficacy and a lower incidence of proarrhythmic effects than class I or other class III antiarrhythmic drugs. 406 407
-
Delays repolarization by prolonging the action potential duration and effective refractory period in cardiac tissue.1 2 3 4 5 6 7 12 13 17 18 19 21 22 25 26 38 355
-
Inhibits transmembrane influx of extracellular sodium ions via fast sodium channels.5 13 32 35 44 355 Combines with fast sodium channels in their inactive state and inhibits recovery after repolarization in a time- and voltage-dependent manner.21 25 32 35 44 46
-
Noncompetitively inhibits α- and β-adrenergic responses to sympathetic stimulation and catecholamine administration.1 3 4 5 6 9 10 11 13 14 15 16 19 21 24 25 34 35 51
-
Depresses sinus node function1 3 4 5 6 9 10 11 14 15 18 20 21 25 26 28 29 30 33 34 35 39 49 50 and automaticity.1 5 6 9 25
-
Relaxes cardiac and vascular smooth muscle, thereby dilating both systemic and coronary arteries.1 3 4 9 10 13 14 17 35 53 54
-
Inhibits extrathyroidal deiodinases,231 237 269 resulting in decreased peripheral conversion of thyroxine (T4) to triiodothyronine (T3).1 4 9 25 35 83 154 231 232 233 234 235 237 253 269 298 355
-
Contains 37.3% iodine; each 200-mg tablet or each mL of the injection contains approximately 75 or 18.7 mg of iodine, respectively.1 2 13 355
-
Inhibits phospholipase (e.g., phospholipase A1, A2, and C)150 270 activity in vitro;35 150 157 270 326 339 production of amiodarone-phospholipid complexes within certain organs may be involved in the development of adverse effects.9 25 35 150 156 157 158 159 161 162 163 164 177 179 183 185 186 187 191 192 193 196 270
-
Inhibits α-galactosidase activity.439
Advice to Patients
-
Importance of patients taking medication exactly as prescribed.431 Importance of not taking a double dose to make up for a missed dose but instead taking the next scheduled dose.431
-
Importance of not interrupting or discontinuing therapy without consulting a clinician, even if improvement is evident, as condition may worsen.431
-
Importance of seeking medical attention immediately or proceeding to a hospital emergency department if too many oral doses are ingested.431
-
If serious adverse effects occur, importance of informing a clinician before discontinuing the drug.431
-
Importance of patients informing clinician of history of BP abnormalities, lung, liver, or thyroid disorders prior to treatment initiation.431
-
Importance of clinicians informing patients of potential toxicities (e.g., lung, liver) that may occur during therapy.355
-
Importance of patients informing clinician of any episodes of shortness of breath, wheezing, coughing, spitting up blood, chest pain, any other breathing disorders, or aggravation of cardiovascular disease.4 431
-
Importance of patients informing clinician of symptoms of thyroid dysfunction such as weakness, weight gain or loss, heat or cold intolerance, hair thinning, sweating, menstrual cycle changes, swelling of the neck (goiter), nervousness, irritability, restlessness, decreased concentration, depression in geriatric patients, or tremor.431
-
Importance of patients contacting their clinician if nausea or vomiting, dark urine, fatigue, yellowing of the skin or whites of eyes, or stomach pain occurs.431
-
Importance of patients contacting their clinician if heart pounding, irregular heart beat, rapid or slow heartbeat, lightheadedness, or faintness occurs.431
-
Importance of patients contacting their clinician if visual disturbances (e.g., blurred vision, visual halos, ocular photosensitivity) occur.431
-
Importance of advising patients that most manufacturers of corneal refractive laser surgery devices consider the procedure to be contraindicated in patients receiving amiodarone.1 355
-
Importance of regular laboratory monitoring (e.g., pulmonary, thyroid, and liver function) and clinical (e.g., cardiac, ophthalmologic) evaluation.1 355
-
Importance of patients informing clinicians of existing or contemplated therapy, including prescription and OTC drugs, dietary supplements and/or herbal products, as well as any concomitant illnesses.1 355
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1 355 Importance of avoiding pregnancy during therapy.431
-
Importance of using sunscreen agents1 25 35 72 153 190 195 283 and protective clothing1 35 190 195 431 and of avoiding excessive exposure to sunlight or sun lamps.25 35 190 431
-
Importance of taking amiodarone in a consistent manner relative to food intake.1 431
-
Importance of not consuming grapefruit juice during oral amiodarone therapy.1 355 431
-
Importance of advising patients of other important precautionary information.1 355
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
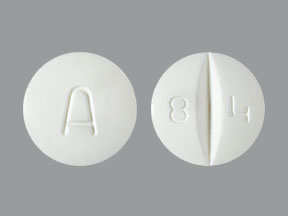
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
100 mg |
Pacerone |
Upsher-Smith |
|
200 mg* |
Amiodarone Hydrochloride Tablets |
|||
|
Cordarone (scored) |
Wyeth |
|||
|
Pacerone (scored) |
Upsher-Smith |
|||
|
400 mg* |
Amiodarone Hydrochloride Tablets |
|||
|
Pacerone (scored) |
Upsher-Smith |
|||
|
Parenteral |
Concentrate for injection, for IV infusion |
50 mg/mL* |
Amiodarone Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Wyeth Pharmaceuticals Inc. Cordarone (amiodarone hydrochloride) tablets prescribing information. Philadelphia, PA; 2008 Apr.
2. Latini R, Tognoni G, Kates RE. Clinical pharmacokinetics of amiodarone. Clin Pharmacokinet. 1984; 9:136-56. https://pubmed.ncbi.nlm.nih.gov/6370540
3. Anon. Amiodarone. Med Lett Drugs Ther. 1986; 28:49-50. https://pubmed.ncbi.nlm.nih.gov/3702807
4. Marcus FI, Fontaine GH, Frank R et al. Clinical pharmacology and therapeutic applications of the antiarrhythmic agent, amiodarone. Am Heart J. 1981; 101:480-93. https://pubmed.ncbi.nlm.nih.gov/7010975
5. Zipes DP, Prystowsky EN, Heger JJ. Amiodarone: electrophysiologic actions, pharmacokinetics and clinical effects. J Am Coll Cardiol. 1984; 3:1059-71. https://pubmed.ncbi.nlm.nih.gov/6368644
6. Singh BN. Amiodarone: historical development and pharmacologic profile. Am Heart J. 1983; 106(4 Part 2):788-97. https://pubmed.ncbi.nlm.nih.gov/6351575
7. Ikeda N, Nademanee K, Kannan R et al. Electrophysiologic effects of amiodarone: experimental and clinical observation relative to serum and tissue drug concentrations. Am Heart J. 1984; 108(4 Part 1):890-8. https://pubmed.ncbi.nlm.nih.gov/6485999
8. Vaughan Williams EM. A classification of antiarrhythmic actions reassessed after a decade of new drugs. J Clin Pharmacol. 1984; 24:129-47. https://pubmed.ncbi.nlm.nih.gov/6144698
9. Sloskey GE. Amiodarone: a unique antiarrhythmic agent. Clin Pharm. 1983; 2:330-40. https://pubmed.ncbi.nlm.nih.gov/6349912
10. Canada AT, Lesko LJ, Haffajee CI et al. Amiodarone for tachyarrhythmias: pharmacology, kinetics, and efficacy. Drug Intell Clin Pharm. 1983; 17:100-4. https://pubmed.ncbi.nlm.nih.gov/6337802
11. Gagnol JP, Devos C, Clinet M et al. Amiodarone: biochemical aspects and haemodynamic effects. Drugs. 1985; 29(Suppl 3):1-10. https://pubmed.ncbi.nlm.nih.gov/2986937
12. Olsson SB, Brorson L, Varnauskas E. Class 3 antiarrhythmic action in man: observations from monophasic action potential recordings and amiodarone treatment. Br Heart J. 1973; 35:1255-9. https://pubmed.ncbi.nlm.nih.gov/4586372
13. Singh BN, Vaughan Williams EM. The effect of amiodarone, a new anti-anginal drug, on cardiac muscle. Br J Pharmacol. 1970; 39:657-67. https://pubmed.ncbi.nlm.nih.gov/5485142
14. Charlier R, Deltour G, Baudine A et al. Pharmacology of amiodarone, an anti-anginal drug with a new biological profile. Arzneimittelforschung. 1968; 18:1408-17. https://pubmed.ncbi.nlm.nih.gov/5755904
15. Charlier R. Cardiac actions in the dog of a new antagonist of adrenergic excitation which does not produce competitive blockade of adrenoreceptors. Br J Pharmacol. 1970; 39:668-74. https://pubmed.ncbi.nlm.nih.gov/5485143
16. Polster P, Broekhuysen J. The adrenergic antagonism of amiodarone. Biochem Pharmacol. 1976; 25:131-4. https://pubmed.ncbi.nlm.nih.gov/1259774
17. Coté P, Bourassa MG, Delaye J et al. Effects of amiodarone on cardiac and coronary hemodynamics and on myocardial metabolism in patients with coronary artery disease. Circulation. 1979; 59:1165-72. https://pubmed.ncbi.nlm.nih.gov/436209
18. Finerman WB Jr, Hamer A, Peter T et al. Electrophysiologic effects of chronic amiodarone therapy in patients with ventricular arrhythmias. Am Heart J. 1982; 104(5 Part 1):987-96. https://pubmed.ncbi.nlm.nih.gov/7137016
19. Bauthier J, Broekhuysen J, Charlier R et al. Nature of the inhibition by amiodarone of isoproterenol-induced tachycardia in the dog. Arch Int Pharmacodyn Ther. 1976; 219:45-51. https://pubmed.ncbi.nlm.nih.gov/1267541
20. Touboul P, Atallah G, Gressard A et al. Effects of amiodarone on sinus node in man. Br Heart J. 1979; 42:573-8. https://pubmed.ncbi.nlm.nih.gov/518781
21. Rosen MR, Wit AL. Electropharmacology of antiarrhythmic drugs. Am Heart J. 1983; 106(4 Part 2):829-39. https://pubmed.ncbi.nlm.nih.gov/6412533
22. Venkatesh N, Somani P, Bersohn M et al. Electropharmacology of amiodarone: absence of relationship to serum, myocardial, and cardiac sarcolemmal drug concentrations. Am Heart J. 1986; 112:916-22. https://pubmed.ncbi.nlm.nih.gov/3776818
23. Nademanee K, Singh BN, Hendrickson JA et al. Pharmacokinetic significance of serum reverse T3 levels during amiodarone treatment: a potential method for monitoring chronic drug therapy. Circulation. 1982; 66:202-11. https://pubmed.ncbi.nlm.nih.gov/7083508
24. Bigger JT Jr, Hoffman BF. Antiarrhythmic drugs. In: Gilman AG, Goodman LS, Rall TW et al, eds. Goodman and Gilman’s the pharmacological basis of therapeutics. 7th ed. New York: The Macmillan Company; 1985:748-83.
25. Naccarelli GV, Rinkenberger RL, Dougherty AH et al. Amiodarone: pharmacology and antiarrhythmic and adverse effects. Pharmacotherapy. 1985; 5:298-313. https://pubmed.ncbi.nlm.nih.gov/2934688
26. Rosenbaum MB, Chiale PA, Halpern MS et al. Clinical efficacy of amiodarone as an antiarrhythmic agent. Am J Cardiol. 1976; 38:934-44. https://pubmed.ncbi.nlm.nih.gov/793369
27. Rowland E, Krikler DM. Electrophysiological assessment of amiodarone in treatment of resistant supraventricular arrhythmias. Br Heart J. 1980; 44:82-90. https://pubmed.ncbi.nlm.nih.gov/7426165
28. Rasmussen V, Berning J. Effect of amiodarone in the Wolff-Parkinson-White snydrome. Acta Med Scand. 1979; 205:31-7. https://pubmed.ncbi.nlm.nih.gov/367085
29. Wellens HJJ, Brugada P, Abdollah H et al. A comparison of the electrophysiologic effects of intravenous and oral amiodarone in the same patient. Circulation. 1984; 69:120-4. https://pubmed.ncbi.nlm.nih.gov/6689635
30. Heger JJ, Prystowsky EN, Jackman WM et al. Amiodarone: clinical efficacy and electrophysiology during long-term therapy for recurrent ventricular tachycardia or ventricular fibrillation. N Engl J Med. 1981; 305:539-45. https://pubmed.ncbi.nlm.nih.gov/6789201
31. Schwartz PJ, Vanoli E. An experimental approach to the choice of antiarrhythmic therapy. Eur Heart J. 1986; 7(Suppl A):135-44. https://pubmed.ncbi.nlm.nih.gov/3720768
32. Mason JW, Hondeghem LM, Katzung BG. Amiodarone blocks inactivated cardiac sodium channels. Pfluegers Arch. 1983; 396:79-81.
33. Gloor HO, Urthaler F, James TN. Acute effects of amiodarone upon the canine sinus node and atrioventricular junctional region. J Clin Invest. 1983; 71:1457-66. https://pubmed.ncbi.nlm.nih.gov/6853721
34. Goupil N, Lenfant J. The effects of amiodarone on the sinus node activity of the rabbit heart. Eur J Pharmacol. 1976; 39:23-31. https://pubmed.ncbi.nlm.nih.gov/964302
35. Mason JW. Amiodarone. N Engl J Med. 1987; 316:455-666. https://pubmed.ncbi.nlm.nih.gov/3543680
36. Morady F, DiCarlo LA Jr, Krol RB et al. Acute and chronic effects of amiodarone on ventricular refractoriness, intraventricular conduction and ventricular tachycardia induction. J Am Coll Cardiol. 1986; 7:148-57. https://pubmed.ncbi.nlm.nih.gov/3941203
37. Wellens HJJ, Lie KI, Bar FW et al. Effect of amiodarone in the Wolff-Parkinson-White syndrome. Am J Cardiol. 1976; 38:189-94. https://pubmed.ncbi.nlm.nih.gov/952262
38. Waleffe A, Bruninx P, Kulbertus HE. Effects of amiodarone studied by programmed electrical stimulation of the heart in patients with paroxysmal re-entrant supraventricular tachycardia. J Electrocardiol. 1978; 11:253-60. https://pubmed.ncbi.nlm.nih.gov/308527
39. Rosenbaum MB, Chiale PA, Ryba D et al. Control of tachyarrhythmias associated with Wolff-Parkinson-White syndrome by amiodarone hydrochloride. Am J Cardiol. 1974; 34:215-23. https://pubmed.ncbi.nlm.nih.gov/4843156
40. Shahar E, Barzilay Z, Frand M et al. Amiodarone in control of sustained tachyarrhythmias in children with Wolff-Parkinson-White syndrome. Pediatrics. 1983; 72:813-6. https://pubmed.ncbi.nlm.nih.gov/6646922
41. Wellens HJJ, Brugada P, Abdollah H. Effect of amiodarone in paroxysmal supraventricular tachycardia with or without Wolff-Parkinson-White syndrome. Am Heart J. 1983; 106(4 Part 2):876-80. https://pubmed.ncbi.nlm.nih.gov/6613833
42. Nademanee K, Hendrickson JA, Cannom DS et al. Control of refractory life-threatening ventricular tachyarrhythmias by amiodarone. Am Heart J. 1981; 101:759-68. https://pubmed.ncbi.nlm.nih.gov/7234654
43. Shenasa M, Denker S. Mahmud R et al. Effect of amiodarone on conduction and refractoriness of the His-Purkinje system in the human heart. J Am Coll Cardiol. 1984; 4:105-10. https://pubmed.ncbi.nlm.nih.gov/6736436
44. Mason JW, Hondeghem LM, Katzung BG. Block of inactivated sodium channels and of depolarization-induced automaticity in guinea pig papillary muscle by amiodarone. Circ Res. 1984; 55:277-85.
45. Morady F, DiCarlo LA Jr, Baerman JM et al. Rate-dependent effects of intravenous lidocaine, procainamide and amiodarone on intraventricular conduction. J Am Coll Cardiol. 1985; 6:179-85. https://pubmed.ncbi.nlm.nih.gov/4008772
46. Yabek SM, Kato R, Singh BN. Acute effects of amiodarone on the electrophysiologic properties of isolated neonatal and adult cardiac fibers. J Am Coll Cardiol. 1985; 5:1109-15. https://pubmed.ncbi.nlm.nih.gov/3989122
47. Wellens HJJ, Bar FW, Dassen WRM et al. Effect of drugs in the Wolff-Parkinson-White syndrome: importance of initial length of effective refractory period of the accessory pathway. Am J Cardiol. 1980; 46:665-9. https://pubmed.ncbi.nlm.nih.gov/7416026
48. Alboni P, Shantha N, Pirani R et al. Effects of amiodarone on supraventricular tachycardia involving bypass tracts. Am J Cardiol. 1984; 53:93-8. https://pubmed.ncbi.nlm.nih.gov/6691283
49. Nademanee K, Hendrickson J, Kannan R et al. Antiarrhythmic efficacy and electrophysiologic actions of amiodarone in patients with life-threatening ventricular arrhythmias: potent suppression of spontaneously occurring tachyarrhythmias versus inconsistent abolition of induced ventricular tachycardia. Am Heart J. 1982; 103:950-9. https://pubmed.ncbi.nlm.nih.gov/7081035
50. Pritchard DA, Singh BN, Hurley PJ. Effects of amiodarone on thyroid function in patients with ischaemic heart disease. Br Heart J. 1975; 37:856-60. https://pubmed.ncbi.nlm.nih.gov/1191447
51. Nokin P, Clinet M, Schoenfeld P. Cardiac β-adrenoceptor modulation by amiodarone. Biochem Pharmacol. 1983; 32:2473-7. https://pubmed.ncbi.nlm.nih.gov/6311220
52. DeBoer LWV, Nosta JJ, Kloner RA et al. Studies of amiodarone during experimental myocardial infarction: beneficial effects on hemodynamics and infarct size. Circulation. 1982; 65:508-12. https://pubmed.ncbi.nlm.nih.gov/7055872
53. Remme WJ, van Hoogenhuyze DCA, Kruyssen DACM et al. Amiodarone: haemodynamic profile during intravenous administration and effect on pacing-induced ischaemia in man. Drugs. 1985; 29(Suppl 3):11-22. https://pubmed.ncbi.nlm.nih.gov/3996243
54. Schwartz A, Shen E, Morady F et al. Hemodynamic effects of intravenous amiodarone in patients with depressed left ventricular function and recurrent ventricular tachycardia. Am Heart J. 1983; 106(4 Part 2):848-56. https://pubmed.ncbi.nlm.nih.gov/6613831
55. Holt DW, Tucker GT, Jackson PR et al. Amiodarone pharmacokinetics. Am Heart J. 1983; 106(4 Part 2):840-7. https://pubmed.ncbi.nlm.nih.gov/6613830
56. Heger JJ, Prystowsky EN, Zipes DP. Relationships between amiodarone dosage, drug concentrations, and adverse side effects. Am Heart J. 1983; 106(4 Part 2):931-5. https://pubmed.ncbi.nlm.nih.gov/6613839
57. Staubli M, Bircher J, Galeazzi RL et al. Serum concentrations of amiodarone during long term therapy: relation to dose, efficacy, and toxicity. Eur J Clin Pharmacol. 1983; 24:485-94. https://pubmed.ncbi.nlm.nih.gov/6861863
58. Riva E, Gerna M, Latini R et al. Pharmacokinetics of amiodarone in man. J Cardiovasc Pharmacol. 1982; 4:264-9. https://pubmed.ncbi.nlm.nih.gov/6175810
59. Andreasen F, Agerbaek H, Bjerregaard P et al. Pharmacokinetics of amiodarone after intravenous and oral administration. Eur J Clin Pharmacol. 1981; 19:293-9. https://pubmed.ncbi.nlm.nih.gov/7286032
60. Anatasiou-Nana M, Levis GM, Moulopoulos S. Pharmacokinetics of amiodarone after intravenous and oral administration. Int J Clin Pharmacol Ther Toxicol. 1982; 20:524-9. https://pubmed.ncbi.nlm.nih.gov/7174155
61. Pourbaix S, Berger Y, Desager JP et al. Absolute bioavailability of amiodarone in normal subjects. Clin Pharmacol Ther. 1985; 37:118-23. https://pubmed.ncbi.nlm.nih.gov/3967454
62. Haffajee CI, Love JC, Canada AT et al. Clinical pharmacokinetics and efficacy of amiodarone for refractory tachyarrhythmias. Circulation. 1983; 67:1347-55. https://pubmed.ncbi.nlm.nih.gov/6851030
63. Boppana VK, Greenspan A, Swanson BN et al. Clinical efficacy and serum concentrations of amiodarone. Clin Pharmacol Ther. 1983; 33:209.
64. Siddoway LA, McAllister CB, Wilkinson GR et al. Amiodarone dosing: a proposal based on its pharmacokinetics. Am Heart J. 1983; 106(4 Part 2):951-6. https://pubmed.ncbi.nlm.nih.gov/6613842
65. Kannan R, Nademanee K, Hendrickson JA et al. Amiodarone kinetics after oral doses. Clin Pharmacol Ther. 1982; 31:438-44. https://pubmed.ncbi.nlm.nih.gov/7060325
66. Ward DE, Camm AJ, Spurrell RAJ. Clinical antiarrhythmic effects of amiodarone in patients with resistant paroxysmal tachycardias. Br Heart J. 1980; 44:91-5. https://pubmed.ncbi.nlm.nih.gov/7426166
67. Kaski JC, Girotti LA, Messuti H et al. Long-term management of sustained, recurrent, symptomatic ventricular tachycardia with amiodarone. Circulation. 1981; 64:273-9. https://pubmed.ncbi.nlm.nih.gov/6788399
68. Rakita L, Sobol SM. Amiodarone in the treatment of refractory ventricular arrhythmias. JAMA. 1983; 250:1293-5. https://pubmed.ncbi.nlm.nih.gov/6348310
69. Coumel P, Lucet V, Do Ngoc D. The use of amiodarone in children. PACE. 1983; 6:930-9. https://pubmed.ncbi.nlm.nih.gov/6195613
70. Haffajee CI, Love JC, Alpert JS et al. Efficacy and safety of long-term amiodarone in treatment of cardiac arrhythmias: dosage experience. Am Heart J. 1983; 106(4 Part 2):935-43. https://pubmed.ncbi.nlm.nih.gov/6613840
71. Graboys TB, Podrid PJ, Lown B. Efficacy of amiodarone for refractory supraventricular tachyarrhythmias. Am Heart J. 1983; 106(4 Part 2):870-6. https://pubmed.ncbi.nlm.nih.gov/6613832
72. Rosenbaum MB, Chiale PA, Haedo A et al. Ten years of experience with amiodarone. Am Heart J. 1983; 106(4 Part 2):957-64. https://pubmed.ncbi.nlm.nih.gov/6613843
73. Mostow ND, Vrobel TR, Noon D et al. Rapid suppression of complex ventricular arrhythmias with high-dose oral amiodarone. Circulation. 1986; 73:1231-8. https://pubmed.ncbi.nlm.nih.gov/3698254
74. Nademanee K, Singh BN, Hendrickson J et al. Amiodarone in refractory life-threatening ventricular arrhythmias. Ann Intern Med. 1983; 98(5 Part 1):577-84. https://pubmed.ncbi.nlm.nih.gov/6846970
75. Rotmensch HH, Belhassen B, Swanson BN et al. Steady-state serum amiodarone concentrations: relationships with antiarrhythmic efficacy and toxicity. Ann Intern Med. 1984; 101:462-9. https://pubmed.ncbi.nlm.nih.gov/6476633
76. Berdeaux A, Roche A, Labaille T et al. Tissue extraction of amiodarone and N-desethylamiodarone in man after a single oral dose. Br J Clin Pharmacol. 1984; 18:759-63. https://pubmed.ncbi.nlm.nih.gov/6508984
77. Staubli M, Troendle A, Schmid B et al. Pharmacokinetics of amiodarone, desethylamiodarone and other iodine-containing amiodarone metabolites. Eur J Clin Pharmacol. 1985; 29:417-23. https://pubmed.ncbi.nlm.nih.gov/4092724
78. Paton DM, Webster DR, Neutze JM. A review of the clinical pharmacokinetics of amiodarone. Methods Find Exp Clin Pharmacol. 1984; 6:41-9. https://pubmed.ncbi.nlm.nih.gov/6371407
79. Canada AT, Lesko LJ, Haffajee CI. Disposition of amiodarone in patients with tachyarrhythmias. Curr Ther Res. 1981; 30:968-74.
80. Broekhuysen J, Laruel R, Sion R. Recherches dans la série des benzofurannes XXXVII: étude comparée du transit et du métabolisme de l’amiodarone chez diverses espèces animales et chez l’homme. (French; with English abstract.) Arch Int Pharmacodyn Ther. 1969; 177:340-59.
81. Rotmensch HH, Swanson BN, Greenspon AJ et al. Amiodarone: individualizing dosage with serum concentrations. PACE. 1983; 6:1327-35. https://pubmed.ncbi.nlm.nih.gov/6196742
82. Debbas NMG, Bexton RS, du Cailar C et al. Relation between myocardial amiodarone concentration and QT interval. Br Heart J. 1983; 49:297.
83. Harris L, McKenna WJ, Rowland E et al. Side effects of long-term amiodarone therapy. Circulation. 1983; 67:45-51. https://pubmed.ncbi.nlm.nih.gov/6291807
84. Adams PC, Holt DW, Storey GCA et al. Amiodarone and its desethyl metabolite: tissue distribution and morphologic changes during long-term therapy. Circulation. 1985; 72:1064-75. https://pubmed.ncbi.nlm.nih.gov/3930086
85. Riva E, Gerna M, Neyroz P et al. Pharmacokinetics of amiodarone in rats. J Cardiovasc Pharmacol. 1982; 4:270-5. https://pubmed.ncbi.nlm.nih.gov/6175811
86. Barbieri E, Conti F, Zampieri P et al. Amiodarone and desethylamiodarone distribution in the atrium and adipose tissue of patients undergoing short- and long-term treatment with amiodarone. J Am Coll Cardiol. 1986; 8:210-3. https://pubmed.ncbi.nlm.nih.gov/3711518
87. Neyroz P, Bonati M. In vitro amiodarone protein binding and its interaction with warfarin. Experientia. 1985; 41:361-3. https://pubmed.ncbi.nlm.nih.gov/3972082
88. Candelpergher G, Buchberger R, Suzzi GL et al. Passagio trans-placentare dell’amiodarone: evidenza elettrocardiografica e documentazione farmacologica in un neonato. (Italian; with English abstract.) G Ital Cardiol. 1982; 12:79-82.
89. Pitcher D, Leather HM, Storey GCA et al. Amiodarone in pregnancy. Lancet. 1983; 1:597-8. https://pubmed.ncbi.nlm.nih.gov/6131292
90. Lalloz MRA, Byfield PGH, Greenwood RM et al. Binding of amiodarone by serum proteins and the effects of drugs, hormones and other interacting ligands. J Pharm Pharmacol. 1984; 36:366-72. https://pubmed.ncbi.nlm.nih.gov/6146666
91. McKenna WJ, Harris L, Rowland E et al. Amiodarone therapy during pregnancy. Am J Cardiol. 1983; 51:1231-3. https://pubmed.ncbi.nlm.nih.gov/6837469
92. Bonati M, Galletti F, Volpi A et al. Amiodarone in patients on long-term dialysis. N Engl J Med. 1983; 308:906. https://pubmed.ncbi.nlm.nih.gov/6835293
93. Wilkinson PR, Rees JR, Storey GCA et al. Amiodarone: prolonged elimination following cessation of chronic therapy. Am Heart J. 1984; 107:787-8. https://pubmed.ncbi.nlm.nih.gov/6322563
94. Adams PC, Holt P, Holt DW. Amiodarone in testis and semen. Lancet. 1985; 1:341. https://pubmed.ncbi.nlm.nih.gov/2857390
95. Harris L, McKenna WJ, Krikler SJ et al. Renal elimination of amiodarone and its desethyl metabolite. Postgrad Med J. 1983; 59:440-2. https://pubmed.ncbi.nlm.nih.gov/6622326
96. Flanagan RJ, Storey GCA, Holt DW et al. Identification and measurement of desethylamiodarone in blood plasma specimens from amiodarone-treated patients. J Pharm Pharmacol. 1982; 34:638-43. https://pubmed.ncbi.nlm.nih.gov/6128385
97. Harris L, McKenna WJ, Rowland E et al. Plasma amiodarone and desethyl amiodarone levels in chronic oral therapy. Circulation. 1981; 64(Suppl IV):A263.
98. Maggioni AP, Maggi A, Volpi A et al. Amiodarone distribution in human tissues after sudden death during Holter recording. Am J Cardiol. 1983; 52:217-8. https://pubmed.ncbi.nlm.nih.gov/6858920
99. Plomp TA, van Rossum JM, Robles de Medina EO et al. Pharmacokinetics and body distribution of amiodarone in man. Arzneimittelforschung. 1984; 34:513-20. https://pubmed.ncbi.nlm.nih.gov/6540111
100. Woosley RL, Echt DS, Roden DM. Effects of congestive heart failure on the pharmacokinetics and pharmacodynamics of antiarrhythmic agents. Am J Cardiol. 1986; 57:25-33B.
101. Kates RE. Metabolites of cardiac antiarrhythmic drugs: their clinical role. Ann N Y Acad Sci. 1984; 432:75-89. https://pubmed.ncbi.nlm.nih.gov/6441496
102. Latini R, Reginato R, Burlingame AL et al. High-performance liquid chromatographic isolation and fast atom bombardment mass spectrometric identification of di-N-desethylamiodarone, a new metabolite of amiodarone in the dog. Biomed Mass Spectrom. 1984; 11:466-71. https://pubmed.ncbi.nlm.nih.gov/6509156
103. Holt DW, Tucker GT, Jackson PR et al. Amiodarone pharmacokinetics. Br J Clin Pract. 1986; 44(Suppl):109-14.
104. Rao RH, McCready VR, Spathis GS. Iodine kinetic studies during amiodarone treatment. J Clin Endocrinol Metab. 1986; 62:563-8. https://pubmed.ncbi.nlm.nih.gov/3944239
105. Cruzan SM. Orphan drugs 1985 records. FDA Talk Paper T86-11. Rockville, MD: Food and Drug Administration; 1986 Feb 13.
106. Woosley RL. Risk/benefit considerations in antiarrhythmic therapy. JAMA. 1986; 256:82-4. https://pubmed.ncbi.nlm.nih.gov/3712719
107. Solares G, Ramos F, Martin-Duran R et al. Is amiodarone an alternative to beta-blockers to treat supraventricular tachycardias in pheochromocytoma? Arch Intern Med. 1986; 146:2085. Letter.
108. Waxman HL, Groh WC, Marchlinski FE et al. Amiodarone for control of sustained ventricular tachyarrhythmia: clinical and electrophysiologic effects in 51 patients. Am J Cardiol. 1982; 50:1066-74. https://pubmed.ncbi.nlm.nih.gov/6291368
109. Leak D, Eydt JN. Amiodarone for refractory cardiac arrhythmias: 10-year study. CMAJ. 1986; 134:495-501. https://pubmed.ncbi.nlm.nih.gov/3948063
110. Wheeler PJ, Puritz R, Ingram DV et al. Amiodarone in the treatment of refractory supraventricular and ventricular arrhythmias. Postgrad Med J. 1979; 55:1-9. https://pubmed.ncbi.nlm.nih.gov/432163
111. Best JF, Rinkenberger R, Lynch L et al. Amiodarone: an effective alternative for recalcitrant supraventricular and ventricular tachycardias. Clin Cardiol. 1986; 9:268-71. https://pubmed.ncbi.nlm.nih.gov/2424656
112. Swan JH, Chisholm AW. Control of recurrent supraventricular tachycardia with amiodarone hydrochloride. Can Med Assoc J. 1976; 114:43-4. https://pubmed.ncbi.nlm.nih.gov/943223
113. Podrid PJ, Lown B. Amiodarone therapy in symptomatic, sustained refractory atrial and ventricular tachyarrhythmias. Am Heart J. 1981; 101:374-9. https://pubmed.ncbi.nlm.nih.gov/7211665
114. Blandford RL, Crampton J, Kudlac H. Intravenous amiodarone in atrial fibrillation complicating myocardial infarction. BMJ. 1982; 284:16-7. https://pubmed.ncbi.nlm.nih.gov/6797619
115. Staubli M, Studer H. The effects of amiodarone on the electrocardiogram of the guineau pig are not explained by interaction with thyroid hormone metabolism alone. Br J Pharmacol. 1986; 88:405-10. https://pubmed.ncbi.nlm.nih.gov/3730700
116. Vitolo E, Tronci M, Larovere MT et al. Amiodarone versus quinidine in the prophylaxis of atrial fibrillation. Acta Cardiol. 1981; 36:431-4. https://pubmed.ncbi.nlm.nih.gov/7039195
117. Faniel R, Schoenfeld P. Efficacy of i.v. amiodarone in converting rapid atrial fibrillation and flutter to sinus rhythm in intensive care patients. Eur Heart J. 1983; 4:180-5. https://pubmed.ncbi.nlm.nih.gov/6861767
118. Santos AL, Aleixo AM, Landeiro J et al. Conversion of atrial fibrillation to sinus rhythm with amiodarone. Acta Med Port. 1979; 1:15-23. https://pubmed.ncbi.nlm.nih.gov/549456
119. Gold RL, Haffajee CI, Charos G et al. Amiodarone for refractory atrial fibrillation. Am J Cardiol. 1986; 57:124-7. https://pubmed.ncbi.nlm.nih.gov/3942054
120. Horowitz LN, Spielman SR, Greenspan AM et al. Use of amiodarone in the treatment of persistent and paroxysmal atrial fibrillation resistant to quinidine therapy. J Am Coll Cardiol. 1985; 6:1402-7. https://pubmed.ncbi.nlm.nih.gov/4067122
121. Solares G, Ramos F, Martin-Duran R et al. Amiodarone, phaeochromocytoma and cardiomyopathy. Anaesthesia. 1986; 41:186-90. https://pubmed.ncbi.nlm.nih.gov/3953991
122. Lubbe WF, Mercer CJ, Roche AHG et al. Amiodarone in long term management of refractory cardiac tachyarrhythmias. N Z Med J. 1981; 93:31-5. https://pubmed.ncbi.nlm.nih.gov/6940024
123. Cowan JC, Gardiner P, Reid DS et al. A comparison of amiodarone and digoxin in the treatment of atrial fibrillation complicating suspected acute myocardial infarction. J Cardiovasc Pharmacol. 1986; 8:252-6. https://pubmed.ncbi.nlm.nih.gov/2422461
124. Varma MPS, Geddes JS, Pantridge JF. D.C. conversion in patients on amiodarone. Eur J Cardiol. 1981; 12:271-4. https://pubmed.ncbi.nlm.nih.gov/7250169
125. Coumel P, Chouty F, Slama R. Logic and empiricism in the selection of antiarrhythmic agents: the role of drug combinations. Drugs. 1985; 29(Suppl 4):68-76. https://pubmed.ncbi.nlm.nih.gov/4006782
126. Brodsky M, Allen B, Ferguson C et al. Amiodarone plus type 1A anti-arrhythmic drugs for the treatment of refractory atrial fibrillation. J Am Coll Cardiol. 1985; 5:480.
127. Kappenberger LJ, Fromer MA, Steinbrunn W et al. Efficacy of amiodarone in the Wolff-Parkinson-White syndrome with rapid ventricular response via accessory pathway during atrial fibrillation. Am J Cardiol. 1984; 54:330-5. https://pubmed.ncbi.nlm.nih.gov/6465013
128. Leak D, Eydt JN. Control of refractory cardiac arrhythmia with amiodarone. Arch Intern Med. 1979; 139:425-8. https://pubmed.ncbi.nlm.nih.gov/434996
129. Brown AK, Primhak RA, Newton P. Use of amiodarone in bradycardia-tachycardia syndrome. Br Heart J. 1978; 40:1149-52. https://pubmed.ncbi.nlm.nih.gov/708517
130. Posse RA, Zuelgaray JTG. Use of amiodarone in bradycardia-tachycardia syndrome. Br Heart J. 1979; 42:369. https://pubmed.ncbi.nlm.nih.gov/508465
131. Brown AK. Use of amiodarone in bradycardia-tachycardia syndrome. Br Heart J. 1979; 42:369. https://pubmed.ncbi.nlm.nih.gov/508465
132. McComb JM, Logan KR, Khan MM et al. Amiodarone-induced ventricular fibrillation. Eur J Cardiol. 1980; 11:381-5. https://pubmed.ncbi.nlm.nih.gov/7398728
133. Lesbre JP, Eloy JP. An open comparison of amiodarone with diltiazem and glyceryl trinitrate in patients with stable exertional angina. Drugs. 1985; 29(Suppl 3):31-6. https://pubmed.ncbi.nlm.nih.gov/3922733
134. Rutilzsky B, Girotti AL, Rosenbaum MB. Efficacy of chronic amiodarone therapy in patients with variant angina and inhibition of ergonovine coronary constriction. Am Heart J. 1982; 103:38-43. https://pubmed.ncbi.nlm.nih.gov/6459732
135. Maheswaran R, Bramble MG, Hardisty CA. Massive digoxin overdose: successful treatment with intravenous amiodarone. BMJ. 1983; 287:392-3. https://pubmed.ncbi.nlm.nih.gov/6409318
136. Kennedy JI, Myers JL, Plumb VJ et al. Amiodarone pulmonary toxicity: clinical, radiologic, and pathologic correlations. Arch Intern Med. 1987; 147:50-5. https://pubmed.ncbi.nlm.nih.gov/3800529
137. Heger JJ, Prystowsky EN, Zipes DP. Clinical efficacy of amiodarone in treatment of recurrent ventricular tachycardia and ventricular fibrillation. Am Heart J. 1983; 106(4 Part 2):887-94. https://pubmed.ncbi.nlm.nih.gov/6613835
138. Kudenchuk PJ, Pierson DJ, Greene HL et al. Prospective evaluation of amiodarone pulmonary toxicity. Chest. 1984; 86:541-8. https://pubmed.ncbi.nlm.nih.gov/6478892
139. Rotmensch HH, Liron M, Tupilski M et al. Possible association of pneumonitis with amiodarone therapy. Am Heart J. 1980; 100:412-3. https://pubmed.ncbi.nlm.nih.gov/7405817
140. Sobol SM, Rakita L. Pneumonitis and pulmonary fibrosis associated with amiodarone treatment: a possible complication of a new antiarrhythmic drug. Circulation. 1982; 65:819-24. https://pubmed.ncbi.nlm.nih.gov/7060263
141. McGovern B, Garan H, Kelly E et al. Adverse reactions during treatment with amiodarone hydrochloride. BMJ. 1983; 287:175-80. https://pubmed.ncbi.nlm.nih.gov/6409240
142. Colgan T, Simon GT, Kay JM et al. Amiodarone pulmonary toxicity. Ultrastruct Pathol. 1984; 6:199-207. https://pubmed.ncbi.nlm.nih.gov/6087525
143. Wright AJ, Brackenridge RG. Pulmonary infiltration and bone marrow depression complicating treatment with amiodarone. BMJ. 1982; 284:1303. https://pubmed.ncbi.nlm.nih.gov/6803952
144. Zaher C, Hamer A, Peter T et al. Low-dose steroid therapy for prophylaxis of amiodarone-induced pulmonary infiltrates. N Engl J Med. 1983; 308:779. https://pubmed.ncbi.nlm.nih.gov/6828130
145. Dake MD, Golden JA. Amiodarone and pulmonary effects. Ann Intern Med. 1983; 98:1028. https://pubmed.ncbi.nlm.nih.gov/6859696
146. Dan M, Greif J. Amiodarone and pneumonitis. Ann Intern Med. 1983; 99:732. https://pubmed.ncbi.nlm.nih.gov/6638735
147. Pollak PT, Sami M. Acute necrotizing pneumonitis and hyperglycemia after amiodarone therapy: case report and review of amiodarone-associated pulmonary disease. Am J Med. 1984; 76:935-9. https://pubmed.ncbi.nlm.nih.gov/6720733
148. Marchlinski FE, Gansler TS, Waxman HL et al. Amiodarone pulmonary toxicity. Ann Intern Med. 1982; 97:839-45. https://pubmed.ncbi.nlm.nih.gov/7149492
149. Riley SA, Williams SE, Cooke NJ. Alveolitis after treatment with amiodarone. BMJ. 1982; 284:161-2. https://pubmed.ncbi.nlm.nih.gov/6799079
150. Hostetler KY, Reasor MJ, Walker ER et al. Role of phospholipase A inhibition in amiodarone pulmonary toxicity in rats. Biochim Biophys Acta. 1986; 875:400-5. https://pubmed.ncbi.nlm.nih.gov/3942773
151. Gibb P, Melendez LJ. Segmental pulmonary consolidation due to amiodarone. CMAJ. 1986; 134:611-3. https://pubmed.ncbi.nlm.nih.gov/3948074
152. Rakita L, Sobol SM, Mostow N et al. Amiodarone pulmonary toxicity. Am Heart J. 1983; 106(4 Part 2):906-16. https://pubmed.ncbi.nlm.nih.gov/6310979
153. Harris L, McKenna WJ, Rowland E et al. Side effects and possible contraindications of amiodarone use. Am Heart J. 1983; 106(4 Part 2):916-23. https://pubmed.ncbi.nlm.nih.gov/6613838
154. Raeder EA, Podrid PJ, Lown B. Side effects and complications of amiodarone therapy. Am Heart J. 1985; 109(5 Part 1):975-83. https://pubmed.ncbi.nlm.nih.gov/3158188
155. Rinder HM, Love JC, Wexler R et al. Amiodarone hepatotoxicity. N Engl J Med. 1986; 314:318-9. https://pubmed.ncbi.nlm.nih.gov/3941726
156. Tordjman K, Katz I, Bursztyn M et al. Amiodarone and the liver. Ann Intern Med. 1985; 102:411-2. https://pubmed.ncbi.nlm.nih.gov/3970484
157. Poucell S, Ireton J, Valencia-Mayoral P et al. Amiodarone-associated phospholipidosis and fibrosis of the liver. Gastroenterology. 1984; 86:926-36. https://pubmed.ncbi.nlm.nih.gov/6706074
158. Simon JB, Manley PN, Brien JF et al. Amiodarone hepatotoxicity simulating alcoholic liver disease. N Engl J Med. 1984; 311:167-72. https://pubmed.ncbi.nlm.nih.gov/6738602
159. Rigas B, Rosenfeld LE, Barwick KW et al. Amiodarone hepatotoxicity: a clinicopathologic study of five patients. Ann Intern Med. 1986; 104:348-51. https://pubmed.ncbi.nlm.nih.gov/3946978
160. Yagupsky P, Gazala E, Sofer S et al. Fatal hepatic failure and encephalopathy associated with amiodarone therapy. J Pediatr. 1985; 107:967-70. https://pubmed.ncbi.nlm.nih.gov/4067758
161. Varma RR, Troup PJ, Komorowski RA et al. Clinical and morphologic effects of amiodarone on the liver. Gastroenterology. 1985; 88:1091-2. https://pubmed.ncbi.nlm.nih.gov/3972228
162. Lim PK, Trewby PN, Storey GCA et al. Neuropathy and fatal hepatitis in a patient receiving amiodarone. BMJ. 1984; 288:1638-9. https://pubmed.ncbi.nlm.nih.gov/6326931
163. Babany G, Mallat A, Zafrani ES et al. Chronic liver disease after low daily doses of amiodarone: report of three cases. J Hepatol. 1986; 3:228-32. https://pubmed.ncbi.nlm.nih.gov/3794303
164. Elving LD, Hoefnagels WHL, Van Haelst UJGM et al. Amiodarone hepatotoxicity. Neth J Med. 1986; 29:303-7. https://pubmed.ncbi.nlm.nih.gov/3796766
165. Sheinman BD, Evans T. Acceleration of ventricular rate by amiodarone in atrial fibrillation associated with the Wolff-Parkinson-White syndrome. BMJ. 1982; 285:999-1000. https://pubmed.ncbi.nlm.nih.gov/6812745
166. McGovern B, Garan H, Ruskin JN. Sinus arrest during treatment with amiodarone. BMJ. 1982; 284:160-1. https://pubmed.ncbi.nlm.nih.gov/6799078
167. McGovern B, Garan H, Ruskin JN. Sinus arrest during treatment with amiodarone. BMJ. 1982; 284:1120. https://pubmed.ncbi.nlm.nih.gov/6802437
168. Veltri EP, Reid PR. Sinus arrest with intravenous amiodarone. Am J Cardiol. 1986; 58:1110-1. https://pubmed.ncbi.nlm.nih.gov/3776867
169. Navalgund AA, Alifimoff JK, Jakymec AJ et al. Amiodarone-induced sinus arrest successfully treated with ephedrine and isoproterenol. Anesth Analg. 1986; 65:414-6. https://pubmed.ncbi.nlm.nih.gov/3954116
170. Liberman BA, Teasdale SJ. Anaesthesia and amiodarone. Can Anaesth Soc J. 1985; 32:629-38. https://pubmed.ncbi.nlm.nih.gov/4075214
171. Moro C, Romero J, Corres Peiretti MA. Amiodarone and hypokalemia: a dangerous combination. Int J Cardiol. 1986; 13:365-8. https://pubmed.ncbi.nlm.nih.gov/3793289
172. Chiale PA, Halpern S, Nau GJ et al. Efficacy of amiodarone during long-term treatment of malignant ventricular arrhythmias in patients with chronic chagasic myocarditis. Am Heart J. 1984; 107:656-65. https://pubmed.ncbi.nlm.nih.gov/6702559
173. Westveer DC, Gadowski GA, Gordon S et al. Amiodarone-induced ventricular tachycardia. Ann Intern Med. 1982; 97:561-2. https://pubmed.ncbi.nlm.nih.gov/7125414
174. Nademanee K, Singh BN. Amiodarone and ventricular tachycardia. Ann Intern Med. 1983; 98:110-1. https://pubmed.ncbi.nlm.nih.gov/6848028
175. Fogoros RN, Anderson KP, Winkle RA et al. Amiodarone: clinical efficacy and toxicity in 96 patients with recurrent, drug-refractory arrhythmias. Circulation. 1983; 68:88-94. https://pubmed.ncbi.nlm.nih.gov/6851057
176. Anastasiou-Nana MI, Anderson JL, Nanas JN et al. High incidence of clinical and subclinical toxicity associated with amiodarone treatment of refractory tachyarrhythmias. Can J Cardiol. 1986; 2:138-45. https://pubmed.ncbi.nlm.nih.gov/2941121
177. Meier C, Kauer B, Müller U et al. Neuromyopathy during chronic amiodarone treatment: a case report: J Neurol. 1979; 220:231-9. (IDIS 211459)
178. Lustman F, Monseu G. Amiodarone and neurological side-effects. Lancet. 1974; 1:568. https://pubmed.ncbi.nlm.nih.gov/4132014
179. Lemaire JF, Autret A, Biziere K et al. Amiodaron neuropathy: further arguments for human drug-induced neurolipidosis. Eur Neurol. 1982; 21:65-8. https://pubmed.ncbi.nlm.nih.gov/7094952
180. Charness ME, Morady F, Scheinman MM. Frequent neurologic toxicity associated with amiodarone therapy. Neurology. 1984; 34:669-71. https://pubmed.ncbi.nlm.nih.gov/6538658
181. Van Zandijcke M, Dewachter A. Pseudotumor cerebri with amiodarone. J Neurol Neurosurg Psych. 1986; 49:1463-4.
182. Alves LE, Rose EP, Klingele TG et al. Adverse effects of amiodarone. JAMA. 1982; 248:1448. https://pubmed.ncbi.nlm.nih.gov/7109162
183. Kaplan LJ, Cappaert WE. Amiodarone keratopathy: correlation to dosage and duration. Arch Ophthalmol. 1982; 100:601-2. https://pubmed.ncbi.nlm.nih.gov/7073573
184. Feiler-Ofry V, Lazar M, Solomon A et al. Amiodarone keratopathy. Ophthalmologica. 1980; 180:257-61. https://pubmed.ncbi.nlm.nih.gov/7207963
185. D’Amico DJ, Kenyon KR, Ruskin JN. Amiodarone keratopathy: drug-induced lipid storage disease. Arch Ophthalmol. 1981; 99:257-61. https://pubmed.ncbi.nlm.nih.gov/6258544
186. Ingram DV. Ocular effects in long-term amiodarone therapy. Am Heart J. 1983; 106(4 Part 2):902-5. https://pubmed.ncbi.nlm.nih.gov/6613837
187. Ingram DV, Jaggarao NSV, Chamberlain DA. Ocular changes resulting from therapy with amiodarone. Br J Ophthalmol. 1982; 66:676-9. https://pubmed.ncbi.nlm.nih.gov/7115651
188. Klingele TG, Alves LE, Rose EP. Amiodarone for ventricular arrhythmias. N Engl J Med. 1981; 305:1587-8. https://pubmed.ncbi.nlm.nih.gov/7312002
189. Coumel P, Fidelle J. Amiodarone in the treatment of cardiac arrhythmias in children: one hundred thirty-five cases. Am Heart J. 1980; 100(6 Part 2):1063-9. https://pubmed.ncbi.nlm.nih.gov/7446409
190. Chalmers RJG, Muston HL, Srinivas V et al. High incidence of amiodarone-induced photosensitivity in north-west England. BMJ. 1982; 285:341. https://pubmed.ncbi.nlm.nih.gov/6212095
191. Delage C, Lagacé R, Huard J. Pseudocyanotic pigmentation of the skin induced by amiodarone: a light and electron microscopic study. Can Med Assoc J. 1975; 112:1205-8. https://pubmed.ncbi.nlm.nih.gov/47784
192. Vos AK, van Ramshorst AGS, Grosfeld JCM et al. A peculiar cutaneous pigmentation from Cordarone. Dermatologica. 1972; 145:297-303. https://pubmed.ncbi.nlm.nih.gov/4654409
193. Matheis H. Amiodarone-Pigmentierung. (German; with English abstract). Dermatologica. 1972; 145:304-18. https://pubmed.ncbi.nlm.nih.gov/4654410
194. Mulrow JP, Mulrow CD, McKenna WJ. Pyridoxine and amiodarone-induced photosensitivity. Ann Intern Med. 1985; 103:68-9. https://pubmed.ncbi.nlm.nih.gov/3890657
195. Ferguson J, de Vane PJ, Wirth M. Prevention of amiodarone-induced photosensitivity. Lancet. 1984; 2:414. https://pubmed.ncbi.nlm.nih.gov/6147496
196. Rappersberger K, Konrad K, Wieser E et al. Morphological changes in peripheral blood cells and skin in amiodarone-treated patients. Br J Dermatol. 1986; 114:189-96. https://pubmed.ncbi.nlm.nih.gov/3947537
197. Kaufmann G. Pyridoxine against amiodarone-induced photosensitivity. Lancet. 1984; 1:51-2. https://pubmed.ncbi.nlm.nih.gov/6140378
198. Guerciolini R, Del Favero A, Cannistraro S. Amiodarone-induced photosensitivity and pyridoxine. Lancet. 1984; 1:962. https://pubmed.ncbi.nlm.nih.gov/6143893
199. Bencini PL, Crosti C, Sala F et al. Toxic epidermal necrolysis and amiodarone treatment. Arch Dermatol. 1985; 121:838. https://pubmed.ncbi.nlm.nih.gov/4015131
200. Panel on Antiretroviral Guidelines for Adults and Adolescents, US Department of Health and Human Services (HHS). Guidelines for the use of antiretroviral agents in HIV-1-infected adults and adolescents (April 8, 2015). Updates may be available at HIV.gov website. https://clinicalinfo.hiv.gov/en/guidelines
201. Rumack BH, ed. Poisindex: Amiodarone. Micromedex, Inc; 1987 May.
202. Bonati M, D’Aranno V, Galletti F et al. Acute overdosage of amiodarone in a suicide attempt. J Toxicol Clin Toxicol. 1983; 20:181-6. https://pubmed.ncbi.nlm.nih.gov/6887311
203. Hansten PD, Horn JR, eds. Amiodarone drug interactions. Drug Interact Newsl. 1987; 7:13-6.
204. Hansten PD. Amiodarone drug interactions. Drug Interact Newsl. 1983; 3:23-6.
205. McGovern B, Geer VR, LaRaia PJ et al. Possible interaction between amiodarone and phenytoin. Ann Intern Med. 1984; 101:650-1. https://pubmed.ncbi.nlm.nih.gov/6486598
206. Gore JM, Haffajee CI, Alpert JS. Interaction of amiodarone and diphenylhydantoin. Am J Cardiol. 1984; 54:1145. https://pubmed.ncbi.nlm.nih.gov/6496340
207. Marcus FI. Drug interactions with amiodarone. Am Heart J. 1983; 106(4 Part 2):924-30. https://pubmed.ncbi.nlm.nih.gov/6137140
208. Watt AH, Stephens MR, Buss DC et al. Amiodarone reduces plasma warfarin clearance in man. Br J Clin Pharmacol. 1985; 20:707-9. https://pubmed.ncbi.nlm.nih.gov/4092002
209. Martinowitz U, Rabinovici J, Goldfarb D et al. Interaction between warfarin sodium and amiodarone. N Engl J Med. 1981; 304:671-2. https://pubmed.ncbi.nlm.nih.gov/7453749
210. Almog S, Shafran N, Halkin H et al. Mechanism of warfarin potentiation by amiodarone: dose- and concentration-dependent inhibition of warfarin elimination. Eur J Clin Pharmacol. 1985; 28:257-61. https://pubmed.ncbi.nlm.nih.gov/4007030
211. Rees A, Dalal JJ, Reid PG et al. Dangers of amiodarone and anticoagulant treatment. BMJ. 1981; 282:1756-7. https://pubmed.ncbi.nlm.nih.gov/6786610
212. Serlin MJ, Sibeon RG, Green GJ. Dangers of amiodarone and anticoagulant treatment. BMJ. 1981; 283:58. https://pubmed.ncbi.nlm.nih.gov/6788267
213. Richard C, Riou B, Fournier C et al. Depression of vitamin K-dependent coagulation by amiodarone. Circulation. 1983; 68(Suppl III):III-278.
214. Hamer A, Peter T, Mandel WJ et al. The potentiation of warfarin anticoagulation by amiodarone. Circulation. 1982; 65:1025-9. https://pubmed.ncbi.nlm.nih.gov/7074739
215. Staiger C, Jauernig R, De Vries J et al. Influence of amiodarone on antipyrine pharmacokinetics in three patients with ventricular tachycardia. Br J Clin Pharmacol. 1984; 18:263-4. https://pubmed.ncbi.nlm.nih.gov/6487468
216. Gallagher JD, Lieberman RW, Meranze J et al. Amiodarone-induced complications during coronary artery surgery. Anesthesiology. 1981; 55:186-8. https://pubmed.ncbi.nlm.nih.gov/6973297
217. Moysey JO, Jaggarao NSV, Grundy EN et al. Amiodarone increases plasma digoxin concentrations. BMJ. 1981; 282:272. https://pubmed.ncbi.nlm.nih.gov/6779981
218. Nademanee K, Kannan R, Hendrickson J et al. Amiodarone-digoxin interaction: clinical significance, time course of development, potential pharmacokinetic mechanisms and therapeutic implications. J Am Coll Cardiol. 1984; 4:111-6. https://pubmed.ncbi.nlm.nih.gov/6736437
219. Fenster PE, White NW, Hanson CD. Pharmacokinetic evaluation of the digoxin-amiodarone interaction. J Am Coll Cardiol. 1985; 5:108-12. https://pubmed.ncbi.nlm.nih.gov/3964797
220. Maragno I, Santastasi G, Gaion RM et al. Influence of amiodarone on oral digoxin bioavailability in healthy volunteers. Int J Clin Pharm Res. 1984; 4:149-53.
221. Hooymans PM, Merkus FWHM. Current status of cardiac glycoside drug interactions. Clin Pharm. 1985; 4:404-13. https://pubmed.ncbi.nlm.nih.gov/2412751
222. Koren G, Hesslein PS, MacLeod SM. Digoxin toxicity associated with amiodarone therapy in children. J Pediatr. 1984; 104:467-70. https://pubmed.ncbi.nlm.nih.gov/6707801
223. Oetgen WJ, Sobol SM, Tri TB et al. Amiodarone-digoxin interaction: clinical and experimental observations. Chest. 1984; 86:75-9. https://pubmed.ncbi.nlm.nih.gov/6734297
224. Ben-Chetrit E, Ackerman Z, Eliakim M. Case report: amiodarone-associated hypothyroidism—a possible cause of digoxin intoxication. Am J Med Sci. 1985; 289:114-6. https://pubmed.ncbi.nlm.nih.gov/3976714
225. Marcus FI. Commentary: digoxin-amiodarone-hypothyroidism interaction. Am J Med Sci. 1985; 289:117-8. https://pubmed.ncbi.nlm.nih.gov/3976715
226. Shea P, Lal R, Kim SS et al. Flecainide and amiodarone interaction. J Am Coll Cardiol. 1986; 7:127-30.
227. Saal AK, Werner JA, Greene HL et al. Effect of amiodarone on serum quinidine and procainamide levels. Am J Cardiol. 1984; 53:1264-7. https://pubmed.ncbi.nlm.nih.gov/6711425
228. Tartini R, Kappenberger L, Steinbrunn W et al. Dangerous interaction between amiodarone and quinidine. Lancet. 1982; 1:1327-9. https://pubmed.ncbi.nlm.nih.gov/6123639
229. Pfisterer M, Burkart F. Effect of short and long term administration of amiodarone on ischaemia-induced left ventricular dysfunction: implications for combined antianginal drug therapy. Drugs. 1985; 29(Suppl 3):23-9. https://pubmed.ncbi.nlm.nih.gov/3922732
230. Borowski GD, Garofano CD, Rose LI et al. Effect of long-term amiodarone therapy on thyroid hormone levels and thyroid function. Am J Med. 1985; 78:443-50. https://pubmed.ncbi.nlm.nih.gov/3976702
231. Mazonson PD, Williams ML, Cantley LK et al. Myxedema coma during long-term amiodarone therapy. Am J Med. 1984; 77:751-4. https://pubmed.ncbi.nlm.nih.gov/6486153
232. Burger A, Dinichert D, Nicod P et al. Effect of amiodarone on serum triiodothyronine, reverse triiodothyronine, thyroxin, and thyrotropin: a drug influencing peripheral metabolism of thyroid hormones. J Clin Invest. 1976; 58:255-9. https://pubmed.ncbi.nlm.nih.gov/783194
233. Jonckheer MH, Blockx P, Broeckaert I et al. “Low T3 syndrome” in patients chronically treated with an iodine-containing drug, amiodarone. Clin Endocrinol. 1978; 9:27-35.
234. Amico JA, Richardson V, Alpert B et al. Clinical and chemical assessment of thyroid function during therapy with amiodarone. Arch Intern Med. 1984; 144:487-90. https://pubmed.ncbi.nlm.nih.gov/6703817
235. Albert SG, Alves LE, Rose EP. Thyroid dysfunction during chronic amiodarone therapy. J Am Coll Cardiol. 1987; 9:175-83. https://pubmed.ncbi.nlm.nih.gov/3794094
236. Hawthorne GC, Campbell NPS, Geddes JS et al. Amiodarone-induced hypothyroidism. A common complication of prolonged therapy: a report of eight cases. Arch Intern Med. 1985; 145:1016-9. https://pubmed.ncbi.nlm.nih.gov/2988473
237. Martino E, Safran M, Aghini-Lombardi F et al. Environmental iodine intake and thyroid dysfunction during chronic amiodarone therapy. Ann Intern Med. 1984; 101:28-34. https://pubmed.ncbi.nlm.nih.gov/6428291
238. Martino E, Aghini-Lombardi F, Mariotti S et al. Treatment of amiodarone associated thyrotoxicosis by simultaneous administration of potassium perchlorate and methimazole. J Endocrinol Invest. 1986; 9:201-7. https://pubmed.ncbi.nlm.nih.gov/3020113
239. Wimpfheimer C, Staubli M, Schadelin J et al. Prednisone in amiodarone-induced thyrotoxicosis. BMJ. 1982; 284:1835-6. https://pubmed.ncbi.nlm.nih.gov/6805719
240. Jonckheer MH, Blockx P, Kaivers R et al. Hyperthyroidism as a possible complication of the treatment of ischemic heart disease with amiodarone. Acta Cardiol. 1973; 238:192-200.
241. Bonati M, Gaspari F, D’Aranno V et al. Physicochemical and analytical characteristics of amiodarone. J Pharm Sci. 1984; 73:829-31. https://pubmed.ncbi.nlm.nih.gov/6737273
242. USP DI: drug information for the health care provider. Johnson KW, ed. 20th ed. Englewood, CO: Micromedex, Inc; 2000:89-94.
243. Greene HL, Graham EL, Werner JA et al. Toxic and therapeutic effects of amiodarone in the treatment of cardiac arrhythmias. J Am Coll Cardiol. 1983; 2:1114-28. https://pubmed.ncbi.nlm.nih.gov/6685151
244. Weinberger I, Rotenberg Z, Fuchs J et al. Amiodarone-induced thrombocytopenia. Arch Intern Med. 1987; 147:735-6. https://pubmed.ncbi.nlm.nih.gov/3827461
245. Antonelli D, Luboshitzky R, Gelbendorf A et al. Amiodarone-induced gynecomastia. N Engl J Med. 1986; 315:1553. https://pubmed.ncbi.nlm.nih.gov/3785317
246. Gasparich JP, Mason JT, Greene HL et al. Non-infectious epididymitis associated with amiodarone therapy. Lancet. 1984; 2:1211-2. https://pubmed.ncbi.nlm.nih.gov/6150253
247. Sonnenblick M, Gottlieb S, Goldstein R et al. Effect of amiodarone on blood lipids. Cardiology. 1986; 73:147-50. https://pubmed.ncbi.nlm.nih.gov/3719600
248. Kannan R, Pollak A, Singh BN. Elevation of serum lipids after chronic administration of amiodarone in rabbits. Atherosclerosis. 1982; 44:19-26. https://pubmed.ncbi.nlm.nih.gov/7115477
249. Santinelli V, Chiariello M, Condorelli M. Chronic amiodarone therapy and hypokalemia. Eur Heart J. 1985; 5:92.
250. Mostow ND, Rakita L, Vrobel TR et al. Amiodarone: intravenous loading for rapid suppression of complex ventricular arrhythmias. J Am Coll Cardiol. 1984; 4:97-104. https://pubmed.ncbi.nlm.nih.gov/6736461
251. Politi A, Poggio G, Margiotta A. Can amiodarone induce hyperglycaemia and hypertriglyceridaemia? Br Med J. 1984; 288:285. (IDIS 181694)
252. Hunt D, Kertes P, Venables S et al. Exacerbation of bronchial asthma following treatment with amiodarone: demonstration of an antiadrenergic effect in vitro . Chest. 1984; 86:492-4. https://pubmed.ncbi.nlm.nih.gov/6088179
253. Rumolo R, Vitolo E, Tronci M et al. Alterations in thyroid function induced by chronic administration of amiodarone. Drugs Exp Clin Res. 1987; 13:29-35. https://pubmed.ncbi.nlm.nih.gov/3595442
254. Escoubet B, Jaillon P, Berger Y et al. Amiodarone and N-desethylamiodarone in plasma, red blood cells, and myocardium after a single oral dose: relation to hemodynamic effects in surgical patients. Am Heart J. 1986; 111:280-5. https://pubmed.ncbi.nlm.nih.gov/3946169
255. Tzivoni D, Keren A, Stern S et al. Disopyramide-induced torsade de pointes . Arch Intern Med. 1981; 141:946-7. https://pubmed.ncbi.nlm.nih.gov/7235820
256. Lee TH, Friedman PL, Goldman L et al. Sinus arrest and hypotension with combined amiodarone-diltiazem therapy. Am Heart J. 1985; 109:163-4. https://pubmed.ncbi.nlm.nih.gov/3966317
257. Nicholls DP, Murtagh JG, Holt DW. Use of amiodarone and digoxin specific Fab antibodies in digoxin overdosage. Br Heart J. 1985; 53:462-4. https://pubmed.ncbi.nlm.nih.gov/3986060
258. Maron BJ, Bonow RO, Cannon RO III et al. Hypertrophic cardiomyopathy: interrelations of clinical manifestations, pathophysiology, and therapy (second of two parts). N Engl J Med. 1987; 316:844-52. https://pubmed.ncbi.nlm.nih.gov/3547135
259. McKenna WJ, Harris L, Perez G et al. Arrhythmia in hypertrophic cardiomyopathy. II: comparison of amiodarone and verapamil in treatment. Br Heart J. 1981; 46:173-8. https://pubmed.ncbi.nlm.nih.gov/7196769
260. Neri R, Mestroni L, Salvi A et al. Ventricular arrhythmias in dilated cardiomyopathy: efficacy of amiodarone. Am Heart J. 1987; 113:707-15. https://pubmed.ncbi.nlm.nih.gov/3825860
261. Fortunati MT, Morandi F, Santarone M et al. Farmacocinetica dell’amiodarone in un caso di intossicazione acuta (8 grammi per os). (Italian; with English abstract.) G Ital Cardiol. 1983; 13:385-8.
262. Nitsch J, Lüderitz B. Beschleunigte Elimination von Amiodaron durch Colestyramin. (German; with English abstract.) Deutsche Med Wochenschr. 1986; 111:1241-4.
263. Derrida JP, Ollagnier J, Benaim R et al. Amiodarone et propranolol: une association dangereuse? Nouv Presse Med. 1979; 8:1429. Letter.
264. Tartini R, Kappenberger L, Steinbrunn W et al. Gefahrliche Interaktionen zwischen Amiodaron und Antiarrhythmika der Klasse I. (German; with English abstract.) Schweiz Med Wochenschr. 1982; 112:1585-7.
265. Raehl CL, Patel AK, LeRoy M. Drug-induced torsade de pointes. Clin Pharm. 1985; 4:675-90. https://pubmed.ncbi.nlm.nih.gov/2416504
266. Keren A, Tzivoni D, Gavish D et al. Etiology, warning signs and therapy of torsade de pointes. Circulation. 1981; 64:1167-74. https://pubmed.ncbi.nlm.nih.gov/7296791
267. Meulendyk J. Anesthetic considerations with amiodarone: report of a case. J Am Osteopath Assoc. 1984; 83:585-8. https://pubmed.ncbi.nlm.nih.gov/6609913
268. Palakurthy PR, Iyer V, Meckler RJ. Unusual neurotoxicity associated with amiodarone therapy. Arch Intern Med. 1987; 147:881-4. https://pubmed.ncbi.nlm.nih.gov/3034178
269. Aanderud S, Sundsfjord J, Aarbakke J. Amiodarone inhibits the conversion of thyroxine to triiodothyronine in isolated rat hepacytes. Endocrinology. 1984; 115:1605-8. https://pubmed.ncbi.nlm.nih.gov/6479103
270. Downar E, Shaikh N, Butany J. Amiodarone—a potent phospholipase inhibitor. J Am Coll Cardiol. 1984; 3:604.
271. Fikkers BG, Bogousslavsky J, Regli F et al. Pseudotumor cerebri with amiodarone. J Neurol Neurosurg Psych. 1986; 49:606.
272. Veltri EP, Reid PR. Amiodarone pulmonary toxicity: early changes in pulmonary function tests during amiodarone rechallenge. J Am Coll Cardiol. 1985; 6:802-5. https://pubmed.ncbi.nlm.nih.gov/4031295
273. Nattel S. The pharmacodynamics of amiodarone and desethylamiodarone. J Am Coll Cardiol. 1985; 5:466.
274. Torres V, Tepper D, Flowers D et al. QT prolongation and the antiarrhythmic efficacy of amiodarone. J Am Coll Cardiol. 1986; 7:142-7. https://pubmed.ncbi.nlm.nih.gov/3941202
275. Gough WB, Zeiler RH, Barreca P et al. Hypotensive action of commercial intravenous amiodarone and polysorbate 80 in dogs. J Cardiovasc Pharmacol. 1982; 4:375-80. https://pubmed.ncbi.nlm.nih.gov/6177932
276. Cohen-Armon M, Schreiber G, Sokolovsky M. Interaction of the antiarrhythmic drug amiodarone with the muscarinic receptor in rat heart and brain. J Cardiovasc Pharmacol. 1984; 6:1148-55. https://pubmed.ncbi.nlm.nih.gov/6084773
277. Sharma AD, Corr PB. Modulation by amiodarone of cardiac adrenergic receptors and their electrophysiologic responsivity to catecholamines. Circulation. 1983; 68(Suppl III):III-99. https://pubmed.ncbi.nlm.nih.gov/6305533
278. Leon MB, Rosing DR, Maron BJ et al. Amiodarone in patients with hypertrophic cardiomyopathy and refractory cardiac symptoms: an alternative to current medical therapy. Circulation. 1984; 70(4 Part II):II-18.
279. Elliott PL, Schauble JF, Rogers MC et al. Risk of decompensation during anesthesia in presence of amiodarone. Circulation. 1983; 68(4 Part II):III-280.
280. Keeton BR, Bucknall CA, Curry PVL et al. Use of amiodarone in childhood. Br J Clin Pract. 1984; 40(Suppl 44):115-20.
281. Garson A Jr, Gillette PC, McVey P et al. Amiodarone treatment of critical arrhythmias in children and young adults. J Am Coll Cardiol. 1984; 4:749-55. https://pubmed.ncbi.nlm.nih.gov/6384328
282. Bucknall CA, Keeton BR, Curry PVL et al. Intravenous and oral amiodarone for arrhythmias in children. Br Heart J. 1986; 56:278-84. https://pubmed.ncbi.nlm.nih.gov/3756044
283. Wyeth-Ayerst Laboratories Inc, Philadelphia, PA: Personal communication.
284. Reviewers’ comments (personal observations); 1987 Aug.
285. Talajic M, DeRoode MR, Nattel S. Comparative electrophysiologic effects of intravenous amiodarone and desethylamiodarone in dogs: evidence for clinically relevant activity of the metabolite. Circulation. 1987; 75:265-71. https://pubmed.ncbi.nlm.nih.gov/3791608
286. Campbell TJ. Kinetics of onset of rate-dependent effects of class I antiarrhythmic drugs are important in determining their effects on refractoriness in guinea-pig ventricle, and provide a theoretical basis for their subclassification. Cardiovasc Res. 1983; 17:344-52. https://pubmed.ncbi.nlm.nih.gov/6883410
287. Mostow ND, Vrobel TR, Rakita L. Transient exacerbation followed by control of ventricular tachycardia with amiodarone. Am Heart J. 1986; 111:178-80. https://pubmed.ncbi.nlm.nih.gov/3946146
288. Nitsch J, Lüderitz B. Amiodarone. N Engl J Med. 1987; 317:452.
289. Mostow ND, Rakita L, Vrobel TR et al. Amiodarone: correlation of serum concentration with suppression of complex ventricular ectopic activity. Am J Cardiol. 1984; 54:569-74. https://pubmed.ncbi.nlm.nih.gov/6475775
290. Shenasa M, Vaisman U, Wojciechowski M et al. Abnormal abdominal computerized tomography with amiodarone therapy and clinical significance. Am Heart J. 1984; 107:929-33. https://pubmed.ncbi.nlm.nih.gov/6720524
291. Mostow ND, Vrobel TR, Noon D et al. Intravenous amiodarone: hemodynamics, pharmacokinetics, electrophysiology, and clinical utility. Clin Prog Electrophysiol Pacing. 1986; 4:342-57.
292. McKenna WJ, Oakley CM, Krikler DM et al. Improved survival with amiodarone in patients with hypertrophic cardiomyopathy and ventricular tachycardia. Br Heart J. 1985; 53:412-6. https://pubmed.ncbi.nlm.nih.gov/4039188
293. Naccarelli GV, Fineberg NS, Zipes DP et al. Amiodarone: risk factors for recurrence of symptomatic ventricular tachycardia identified at electrophysiologic study. J Am Coll Cardiol. 1985; 6:814-21. https://pubmed.ncbi.nlm.nih.gov/3928727
294. Wood DL, Kazmier FJ, Osborn MJ et al. Ischemic optic neuritis as a manifest reaction of amiodarone. Circulation. 1986; 74(Suppl II):II-226.
295. Baerman JM, Annesley T, DiCarlo LA Jr et al. Interrelationships between serum levels of amiodarone, desethylamiodarone, reverse T3 and the QT interval during long-term amiodarone treatment. Am Heart J. 1986; 111:644-8. https://pubmed.ncbi.nlm.nih.gov/3953386
296. Kay GN, Pryor DB, Lee KL et al. Comparison of survival of amiodarone-treated patients with coronary artery disease and malignant ventricular arrhythmias with that of a control group with coronary artery disease. J Am Coll Cardiol. 1987; 9:877-81. https://pubmed.ncbi.nlm.nih.gov/3558986
297. Latham KR, Sellitti DF, Goldstein RE. Interaction of amiodarone and desethylamiodarone with solubilized nuclear thyroid hormone receptors. J Am Coll Cardiol. 1987; 9:872-6. https://pubmed.ncbi.nlm.nih.gov/3558985
298. Mechlis S, Lubin E, Laor J et al. Amiodarone-induced thyroid gland dysfunction. Am J Cardiol. 1987; 59:833-5. https://pubmed.ncbi.nlm.nih.gov/3825945
299. DePaola AAV, Horowitz LN, Spielman SR et al. Development of congestive heart failure and alterations in left ventricular function in patients with sustained ventricular tachyarrhythmias treated with amiodarone. Am J Cardiol. 1987; 60:276-80. https://pubmed.ncbi.nlm.nih.gov/3303888
300. Kasim SE, Bagchi N, Brown TR et al. Effect of amiodarone on serum lipids, lipoprotein lipase, and hepatic triglyceride lipase. Endocrinology. 1987; 120:1991-5. https://pubmed.ncbi.nlm.nih.gov/3569123
301. Labaz Sanofi UK Ltd. Cordarone X Intravenous (amiodarone hydrochloride) prescribing information. Manchester, England; 1986 Feb.
302. Quattromani A, Birge S, Smith P et al. Early effects of amiodarone therapy on thyroid function. Circulation. 1986; 74(Suppl 2):II-225. https://pubmed.ncbi.nlm.nih.gov/3742762
303. Horowitz LN, Greenspan AM, Spielman SR et al. Usefulness of electrophysiologic testing in evaluation of amiodarone therapy for sustained ventricular tachyarrhythmias associated with coronary heart disease. Am J Cardiol. 1985; 55:367-71. https://pubmed.ncbi.nlm.nih.gov/3969870
304. Fogoros RN. Amiodarone-induced refractoriness to cardioversion. Ann Intern Med. 1984; 100:699-700. https://pubmed.ncbi.nlm.nih.gov/6712033
305. Wiersinga WM, Endert E, Trip MD et al. Immunoradiometric assay of thyrotropin in plasma: its value in predicting response to thyroliberin stimulation and assessing thyroid function in amiodarone-treated patients. Clin Chem. 1986; 32:433-6. https://pubmed.ncbi.nlm.nih.gov/3081279
306. Mason JW, Amiodarone Toxicity Study Group. Toxicity of amiodarone. Circulation. 1985; 72(4 Part II):III-270.
307. Liu FL, Cohen RD, Downar E et al. Amiodarone pulmonary toxicity: functional and ultrastructural evaluation. Thorax. 1986; 41:100-5. https://pubmed.ncbi.nlm.nih.gov/3010484
308. Adams PC, Gibson GJ, Morley AR et al. Amiodarone pulmonary toxicity: clinical and subclinical features. Quart J Med. 1986; 59:449-71. https://pubmed.ncbi.nlm.nih.gov/3763811
309. Nalos PC, Kass RM, Gang ES et al. Life-threatening postoperative pulmonary complications in patients with previous amiodarone pulmonary toxicity undergoing cardiothoracic operations. J Thorac Cardiovasc Surg. 1987; 93:904-12. https://pubmed.ncbi.nlm.nih.gov/3573800
310. Staubli M, Studer H. Amiodarone-treated patients with TSH test are at risk of thyrotoxicosis. Klin Wochenschr. 1985; 63:168-75. https://pubmed.ncbi.nlm.nih.gov/3920432
311. Feiner LA, Younge BR, Kazmier FJ et al. Optic neuropathy and amiodarone therapy. Mayo Clin Proc. 1987; 62:702-17. https://pubmed.ncbi.nlm.nih.gov/3600041
312. Oreto G, Lapresa V, Melluso C et al. Intoxication aiguë par l’amiodarone: description d’un cas. (French; with English abstract.) Arch Mal Coeur. 1980; 73:857-61.
313. Windle J, Prystowsky EN, Miles WM et al. Pharmacokinetic and electrophysiologic interactions of amiodarone and procainamide. Clin Pharmacol Ther. 1987; 41:603-10. https://pubmed.ncbi.nlm.nih.gov/3581646
314. Enia G, Caralano C, Zoccali C et al. Amiodarone. N Engl J Med. 1987; 317:452.
315. Enia G, Costante G, Caralano C et al. Severe hypothyroidism induced by amiodarone in a dialysis patient. Nephron. 1987; 46:206-7. https://pubmed.ncbi.nlm.nih.gov/3600929
316. O’Reilly RA, Trager WF, Rettie AE et al. Interaction of amiodarone with racemic warfarin and its separated enantiomorphs in humans. Clin Pharmacol Ther. 1987; 42:290-4. https://pubmed.ncbi.nlm.nih.gov/3621782
317. Nattel S, Talajic M, Quantz M et al. Frequency-dependent effects of amiodarone on atrioventricular nodal function and slow-channel action potentials: evidence for calcium channel-blocking activity. Circulation. 1987; 76:442-9. https://pubmed.ncbi.nlm.nih.gov/3608127
318. Feld GK, Nademanee K, Stevenson W et al. Clinical and electrophysiologic effects of amiodarone in patients with atrial fibrillation complicating the Wolff-Parkinson-White syndrome. Am Heart J. 1988; 115(1 Part 1):102-7. https://pubmed.ncbi.nlm.nih.gov/3336964
319. Fan K, Bell R, Eudy S et al. Amiodarone-associated pulmonary fibrosis: evidence of an immunologically mediated mechanism. Chest. 1987; 92:625-30. https://pubmed.ncbi.nlm.nih.gov/3308345
320. Riker Laboratories Inc. Tambocor (flecainide acetate) B.I.D. prescribing information. St. Paul, MN; 1986 Nov.
321. Moots RJ, Banerjee A. Exfoliative dermatitis after amiodarone treatment. BMJ. 1988; 296:1332-3. https://pubmed.ncbi.nlm.nih.gov/2968133
322. Lazzara R. Amiodarone and torsade de pointes. Ann Intern Med. 1989; 111:549-51. https://pubmed.ncbi.nlm.nih.gov/2672929
323. Mattioni TA, Zheutlin TA, Sarmiento JJ et al. Amiodarone in patients with previous drug-mediated torsade de pointes: long-term safety and efficacy. Ann Intern Med. 1989; 111:574-80. https://pubmed.ncbi.nlm.nih.gov/2774388
324. Dusman RE, Stanton MS, Miles WM et al. Clinical features of amiodarone-induced pulmonary toxicity. Circulation. 1990; 82:51-9. https://pubmed.ncbi.nlm.nih.gov/2364524
325. Counihan PJ, McKenna WJ. Risk-benefit assessment of amiodarone in the treatment of cardiac arrhythmias. Drug Safety. 1990; 5:285-304.
326. Wilson JS, Podrid PJ. Side effects from amiodarone. Am Heart J. 1991; 121:158-71. https://pubmed.ncbi.nlm.nih.gov/1985357
327. Naccarelli GV, Rinkenberger RL, Dougherty AH et al. Adverse effects of amiodarone: pathogenesis, incidence and management. Med Toxicol Adverse Drug Exp. 1989; 4:246-53. https://pubmed.ncbi.nlm.nih.gov/2671595
328. Adams GD, Kehoe R, Lesch M et al. Amiodarone-induced pneumonitis: assessment of risk factors and possible risk reduction. Chest. 1988; 93:254-62. https://pubmed.ncbi.nlm.nih.gov/3338292
329. Arnon R, Raz I, Chajek-Shaul T et al. Amiodarone pulmonary toxicity presenting as a solitary lung mass. Chest. 1988; 93:425-7. https://pubmed.ncbi.nlm.nih.gov/3338315
330. De Wolf D, De Schepper J, Verhaaren H et al. Congenital hypothyroid and goiter and amiodarone. Acta Paediatr Scand. 1988; 77:616-8. https://pubmed.ncbi.nlm.nih.gov/3394521
331. Ohar JA, Jackson F Jr, Redd RM et al. Usefulness of serial pulmonary function testing as an indicator of amiodarone toxicity. Am J Cardiol. 1989; 64:1322-6. https://pubmed.ncbi.nlm.nih.gov/2589198
332. Akoun GM, Gauthier-Rahman S, Liote HA et al. Leukocyte migration inhibition in amiodarone-associated pneumonitis. Chest. 1988; 94:1050-3. https://pubmed.ncbi.nlm.nih.gov/3053057
333. Manolis AS, Tordjman T, Mack KD et al. Atypical pulmonary and neurologic complications of amiodarone in the same patient: report of a case and review of the literature. Arch Intern Med. 1987; 147:1805-9. https://pubmed.ncbi.nlm.nih.gov/3310943
334. Kay GN, Epstein AE, Kirklin JK et al. Fatal postoperative amiodarone pulmonary toxicity. Am J Cardiol. 1988; 62:490-2. https://pubmed.ncbi.nlm.nih.gov/3414530
335. Horowitz LN. Detection of amiodarone pulmonary toxicity: to screen or not to screen, that is the question! J Am Coll Cardiol. 1988; 12:789-90. Editorial.
336. Magro SA, Lawrence EC, Wheeler SH et al. Amiodarone pulmonary toxicity: prospective evaluation of serial pulmonary function tests. J Am Coll Cardiol. 1988; 12:781-8. https://pubmed.ncbi.nlm.nih.gov/3403839
337. Zhu YY, Botvinick E, Dae M et al. Gallium lung scintigraphy in amiodarone pulmonary toxicity. Chest. 1988; 93:1126-31. https://pubmed.ncbi.nlm.nih.gov/3371091
338. Martin WJ II, Rosenow EC III. Amiodarone pulmonary toxicity: I. Recognition and pathogenesis. Chest. 1988; 93:1067-75. https://pubmed.ncbi.nlm.nih.gov/3282816
339. Martin WJ II, Rosenow EC III. Amiodarone pulmonary toxicity: II. Recognition and pathogenesis. Chest. 1988; 93:1242-8. https://pubmed.ncbi.nlm.nih.gov/3286141
340. Figge J, Dluhy RG. Amiodarone-induced elevation of thyroid stimulating hormone in patients receiving levothyroxine for primary hypothyroidism. Ann Intern Med. 1990; 113:553-5. https://pubmed.ncbi.nlm.nih.gov/2393210
341. Morse RM, Valenzuela GA, Greenwald TP et al. Amiodarone-induced liver toxicity. Ann Intern Med. 1988; 109:838-40. https://pubmed.ncbi.nlm.nih.gov/3190031
342. Robinson K, Mulrow JP, Rowland E et al. Long-term effects of amiodarone on hepatic function. Am J Cardiol. 1989; 64:95-6. https://pubmed.ncbi.nlm.nih.gov/2741820
343. Keung EC. Antiarrhythmic treatment and myocardial infarction. J Am Coll Cardiol. 1990; 16:1719-21. https://pubmed.ncbi.nlm.nih.gov/2254559
344. Burkart F, Pfisterer M, Kiowski W et al. Effect of antiarrhythmic therapy on mortality in survivors of myocardial infarction with asymptomatic complex ventricular arrhythmias: Basel antiarrhythmic study of infarct survival (BASIS). J Am Coll Cardiol. 1990; 16:1711-8. https://pubmed.ncbi.nlm.nih.gov/2254558
345. Martin WJ II. Mechanisms of amiodarone pulmonary toxicity. Clin Chest Med. 1990; 11:131-8. https://pubmed.ncbi.nlm.nih.gov/2182274
346. Haas C, Hugues FC, Le Jeunne C. Drup-induced pleural pathology (excluding antineoplastic chemotherapy). (French; with English abstract.) Ann Med Interne. (Paris) 1989; 140:589-92.
347. Olivieri D, Pesci A, Bertorelli G. Eosinophilic alveolitis in immunologic interstitial lung disorder. Lung. 1990; 168(Suppl):964-73. https://pubmed.ncbi.nlm.nih.gov/2117217
348. Terra Filho M, Vargas FS, Cukier A et al. Pneumonitis induced by amiodarone. (Portuguese; with English abstract.) Arq Bras Cardiol. 1989; 53:201-5.
349. Akoun GM, Milleron BJ, Badaro DM et al. Pleural T-lymphocyte subsets in amiodarone-associated pleuropneumonitis. Chest. 1989; 95:596-7. https://pubmed.ncbi.nlm.nih.gov/2784094
350. Chrysanthopoulos C, Siablis D, Kounis NG. Amiodarone-induced recurrent allergic pneumonitis. Ann Allergy. 1988; 60:111-4. https://pubmed.ncbi.nlm.nih.gov/3341613
351. Israel-Biet D, Venet A, Caubarrere I et al. Bronchoalveolar lavage in amiodarone pneumonitis: cellular abnormalities and their relevance to pathogenesis. Chest. 1987; 91:214-21. https://pubmed.ncbi.nlm.nih.gov/3802932
352. Caubarrere I, Bonan G, Venet A et al. Pneumopathies caused by hypersensitivity to amiodarone and associated nephropathies: study by alveolar lavage. (French; with English abstract.) Ann Med Interne. (Paris) 1985; 136:311-5.
353. Venet A, Caubarrere I, Bonan G. Five cases of immune-mediated amiodarone pneumonitis. Lancet. 1984; 1:962-3. https://pubmed.ncbi.nlm.nih.gov/6143896
354. Laurent M, Betremieux P, Biron Y et al. Neonatal hypothyroidism after treatment by amiodarone during pregnancy. Am J Cardiol. 1987; 60:942. https://pubmed.ncbi.nlm.nih.gov/3661421
355. Abraxis Pharmaceutical Products. Amiodarone hydrochloride injection prescribing information. Schaumburg, IL; 2006 Sep.
356. Food and Drug Administration. Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97-414), to June 28, 1996. Rockville, MD; 1996 Jul.
357. Deitch MW. Dear doctor letter regarding appropriate use of Cordarone. Philadelphia, PA: Wyeth-Ayerst Laboratories; undated. (received 1997 June 30.)
358. Food and Drug Administration. Enkaid and Tambocor use in non-life-threatening arrhythmias halted. FDA Talk Paper. 1989 Apr 25.
359. The Cardiac Arrhythmia Suppression Trial (CAST) investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989; 321:406-12. https://pubmed.ncbi.nlm.nih.gov/2473403
360. Ruskin JN. The Cardiac Arrhythmia Suppression Trial (CAST). N Engl J Med. 1989; 321:386-8. https://pubmed.ncbi.nlm.nih.gov/2501683
361. Pratt CM, Brater DC, Harrell FE Jr et al. Clinical and regulatory implications of the Cardiac Arrhythmia Suppression Trial. Am J Cardiol. 1990; 65:103-5. https://pubmed.ncbi.nlm.nih.gov/1688479
362. Anon. Restrictions on use of flecainide, encainide. FDA Drug Bull. 1989; 16.
363. Nightingale SL. Flecainide and encainide not to be used in non-life-threatening arrhythmias. JAMA. 1989; 261:3368. https://pubmed.ncbi.nlm.nih.gov/2498536
364. Ryan TJ, Antman EM, Brooks NH et al. ACC/AHA guidelines for the management of patients with acute myocardial infarction: 1999 update: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Management of Acute Myocardial Infarction).
365. Scheinman MM, Levine JH, Cannom DS et al. Dose-ranging study of intravenous amiodarone in patients with life-threatening ventricular tachyarrhythmias. Circulation. 1995; 92:3264-72. https://pubmed.ncbi.nlm.nih.gov/7586313
366. Janssen Pharmaceuticals Inc. Levaquin (levofloxacin) tablets, oral solution, concentrate for IV use, and solution for IV use prescribing information. Titusville, NJ; 2014 May.
367. Muir AD, Wilson M. Amiodarone and psoriasis. N Z Med J. 1982; 95:711. https://pubmed.ncbi.nlm.nih.gov/6959024
368. Cairns JA, Connolly SJ, Roberts R et al. Randomised trial of outcome after myocardial infarction in patients with frequent or repetitive ventricular premature depolarisation: CAMIAT. Lancet. 1997; 349:675-82. https://pubmed.ncbi.nlm.nih.gov/9078198
369. Sim I, McDonald KM, Lavori PW et al. Quantitative overview of randomized trials of amiodarone to prevent sudden cardiac death. Circulation. 1997; 96:2823-9. https://pubmed.ncbi.nlm.nih.gov/9386144
370. Julian DG, Camm AJ, Frangin G et al. Randomised trial of effect of amiodarone on mortality in patients with left-ventricular dysfunction after recent myocardial infarction: EMIAT. Lancet. 1997; 349:667-74. https://pubmed.ncbi.nlm.nih.gov/9078197
371. Merck & Co, Inc. Zocor (simvastatin) tablets prescribing information. Whitehouse Station, NJ; 2008 Jun.
372. Doval HC, Nul DR, Grancelli HO et al. Randomised trial of low-dose amiodarone in severe congestive heart failure. Lancet. 1994; 344:493-8. https://pubmed.ncbi.nlm.nih.gov/7914611
373. Garguichevich JJ, Ramos JL, Gambarte A et al. Effect of amiodarone therapy on mortality in patients with left ventricular dysfunction and asymptomatic complex ventricular arrhythmias: Argentine pilot study of sudden death and amiodarone (EPAMSA). Am Heart J. 1995; 130:494-500. https://pubmed.ncbi.nlm.nih.gov/7661066
374. Amiodarone Trials Meta-Analysis Investigators. Effect of prophylactic amiodarone on mortality after acute myocardial infarction and in congestive heart failure: meta-analysis of individual data from 6500 patients in randomised trials. Lancet. 1997; 350:1417-24. https://pubmed.ncbi.nlm.nih.gov/9371164
375. Teo KK, Yusuf S, Furberg CD. Effects of prophylactic antiarrhytmic drug therapy in acute myocardial infarction. JAMA. 1993; 270:1589-95. https://pubmed.ncbi.nlm.nih.gov/8371471
376. Norris RM. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1767. https://pubmed.ncbi.nlm.nih.gov/9193396
377. Cleland JGF, Erhardt L. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1767. https://pubmed.ncbi.nlm.nih.gov/9193397
378. Malik M, Camm AJ. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1767-8. https://pubmed.ncbi.nlm.nih.gov/9193398
379. Incalzi RA. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1768. https://pubmed.ncbi.nlm.nih.gov/9193399
380. Pinski SL. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1768. https://pubmed.ncbi.nlm.nih.gov/9193400
381. Julian DG, Camm AJ. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1769.
382. Cairns JA, Connolly SJ, Roberts R et al. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1769-70.
383. Gottlieb SS. Amiodarone after myocardial infarction: EMIAT and CAMIAT trials. Lancet. 1997; 349:1770. https://pubmed.ncbi.nlm.nih.gov/9193401
384. Camm AJ, Julian D, Janse G et al. The European Myocardial Infarct (EMIAT). Am J Cardiol. 1993; 72:95-98F. https://pubmed.ncbi.nlm.nih.gov/8517437
385. Singh SN, Fletcher RD, Fisher SG et al. Amiodarone in patients with congestive heart failure and asymptomatic ventricular arrhythmia. N Engl J Med. 1995; 333:77-82. https://pubmed.ncbi.nlm.nih.gov/7539890
386. Silver MJ, Young J, Topol EJ. Amiodarone in congestive heart failure. N Engl J Med. 1995; 333:1639-40. https://pubmed.ncbi.nlm.nih.gov/7477207
387. Breithardt G. . Amiodarone in patients with heart failure. N Engl J Med. 1995; 333:121-2. https://pubmed.ncbi.nlm.nih.gov/7777017
388. Bosch X, Bernadich. Acute pancreatitis during treatment with amiodarone. Lancet. 1997; 350:1300. https://pubmed.ncbi.nlm.nih.gov/9357418
389. Vizioli LD, Cho S. Amiodarone-associated hemoptysis. Chest. 1994; 105:305-6. https://pubmed.ncbi.nlm.nih.gov/8275760
390. Cheung B, Lam FM, Kumana CR. Insidiously evolving, occult drug interaction involving warfarin and amiodarone. BMJ. 1996; 312:106-7.
391. Gottlieb SS. Dead is dead—artificial definitions are no substitute. it/Lancet. 1997; 349:662-3. (IDIS 381353) ,RT>392.Richer M, Robert S. Fatal hepatoxicity following oral administration of amiodarone. Ann Pharmacother. 1995; 29:582-6. https://pubmed.ncbi.nlm.nih.gov/7663029
393. Ceremuzynski L, Kleczar E, Krzeminska-Pakula M et al. Effect of amiodarone on mortality after myocardial infarction: a double-bliond, placebo-controlled, pilot study. J Am Coll Cardiol. 1992; 20:1056-62. https://pubmed.ncbi.nlm.nih.gov/1401602
394. Cairns JA, Connolly SJ, Roberts R et al. Canadian amiodarone myocardial infarction arrhythmia trial (CAMIAT): rationale and protocol. Am J Cardiol. 1993; 72:87-94F.
395. Kudenchuk PJ, Cobb LA, Copass MK et al. Amiodarone for resuscitation after out-of-hosptal cardiac arrest due to venricular fibrillation. N Engl J Med. 1999; 341:871-8. https://pubmed.ncbi.nlm.nih.gov/10486418
396. Desai AD, Chun S, Sung RJ. The role of intravenous amiodarone in the management of cardiac arrhythmias. Ann Intern Med. 1997; 127:294-303. https://pubmed.ncbi.nlm.nih.gov/9265430
397. American College of Cardiology and American Heart Association. ACC/AHA guidelines for the management of patients with acute myocardial infarction: executive summary and recommendations. Circulation. 1999; 100:1016-1030. https://pubmed.ncbi.nlm.nih.gov/10468535
398. Wyeth-Ayerst Laboratories. American Home Products Corporation’s Cordarone (amiodarone HCl) improved survival to hospital by 29%: published data offers hope to patients with life-threatening condition both insode and outside hospital setting. Press release. Madison, NJ; 1999 Sep 15.
401. Lui CY, Franchina JJ. Verapamil and multifocal atrial tachycardia. Ann Intern Med. 1988; 108:485-6.
402. Roy D, Talajic M, Dorian P et al. Amiodarone to prevent recurrence of atrial fibrillation. N Engl J Med. 2000; 342:913-20. https://pubmed.ncbi.nlm.nih.gov/10738049
403. Arsura EL, Scher DL. Verapamil and multifocal atrial tachycardia. Ann Intern Med. 1988; 108:486. Letter.
404. Scher DL, Arsura EL. Multifocal atrial tachycardia: mechanisms, clinical correlates, and treatment. Am Heart J. 1989; 118:574-80.
405. Arsura E, Lefkin AS, Scher DL et al. A randomized, double-blind, placebo-controlled study of verapamil and metoprolol in treatment of multifocal atrial tachycardia. Am J Med. 1988; 85:519-24. [Errtum: Am J Med. 1989; 86:142.]
406. Hohnloser SH, Singh BN. Proarrhythmia with class III antiarrhythmic drugs: definition, electrophysiologic mechanisms, incidence, predisposing factors, and clinical implications. J Cardiovasc Electrophysiol. 1995; 6:920-36. https://pubmed.ncbi.nlm.nih.gov/8548113
407. Goldschlager N, Epstein AE, Naccarelli G et al. Practical guidelines for clinicans who treat patients with amiodarone. Arch Intern Med. 2000; 160:1741-8. https://pubmed.ncbi.nlm.nih.gov/10871966
408. de Vane PJ. Dear doctor letter regarding off-label use of Cordarone IV in pediatric patients. Philadelphia, PA: Wyeth-Ayerst Laboratories; 2001 March 21.
409. American Academy of Pediatrics Committee on Fetus and Newborn and Committee on Drugs. Benzyl alcohol: toxic agent in neonatal units. Pediatrics. 1983; 72:356-8. https://pubmed.ncbi.nlm.nih.gov/6889041
410. Anon. Benzyl alcohol may be toxic to newborns. FDA Drug Bull. 1982; 12(2):10-11. https://pubmed.ncbi.nlm.nih.gov/7188569
411. Centers for Disease Control. Neonatal deaths associated with use of benzyl alcohol. MMWR Morb Mortal Wkly Rep. 1982; 31:290-1. https://pubmed.ncbi.nlm.nih.gov/6810084
412. Gershanik J, Boecler B, Ensley H et al. The gasping syndrome and benzyl alcohol poisoning. N Engl J Med. 1982; 307:1384-8. https://pubmed.ncbi.nlm.nih.gov/7133084
413. Menon PA, Thach BT, Smith CH et al. Benzyl alcohol toxicity in a neonatal intensive care unit: incidence, symptomatology, and mortality. Am J Perinatol. 1984; 1:288-92. https://pubmed.ncbi.nlm.nih.gov/6440575
414. Anderson CW, Ng KJ, Andresen B et al. Benzyl alcohol poisoning in a premature newborn infant. Am J Obstet Gynecol. 1984; 148:344-6. https://pubmed.ncbi.nlm.nih.gov/6695984
415. NTP-CERHR expert panel report on di(2-ethylhexyl) phthalate. From the National Toxicology Program website:. https://ntp.niehs.nih.gov
416. Perry JC, Fenrich AL, Hulse JE et al. Pediatric use of intravenous amiodarone: efficacy and safety in critically ill patients from a multicenter protocol. J Am Coll Cardiol. 1996; 27:1246-50. https://pubmed.ncbi.nlm.nih.gov/8609351
417. Merck & Co, Inc. Mevacor (lovastatin) tablets prescribing information. Whitehouse Station, NJ; 2008 Sep.
418. Landers MD, Reiter MJ. General principles of antiarrhythmic therapy for ventricular tachyarrhythmias. Am J Cardiol. 1997; 80(Suppl 8A):31-44G.
419. Huikuri HV, Castellanos A, Myerburg RJ. Sudden death due to cardica arrhythmias. N Engl J Med. 2001; 345:1473-82. https://pubmed.ncbi.nlm.nih.gov/11794197
420. Dorian P, Cass D, Schwartz B et al. Amiodarone as Compared with Lidocaine for Shock-Resistant Ventricular Fibrillation. N Engl J Med. 2002; 346:884-890. https://pubmed.ncbi.nlm.nih.gov/11907287
421. Bigger JT. Expanding indications for implantable cardiac defibrillators. N Engl J Med. 2002; 346:931-3. https://pubmed.ncbi.nlm.nih.gov/11907294
422. Moss AJ, Zareba W, Hall WJ et al. Prophylactic implantation of a defibrillator in patients with myocardial infarction and reduced ejection fraction. N Engl J Med. 2002; 346:877-83. https://pubmed.ncbi.nlm.nih.gov/11907286
423. Connolly SJ, Hallstrom AP, Cappato R et al. Meta-analysis of the implantable cardioverter defibrillator secondary prevention trials. AVID, CASH and CIDS studies. Antiarrhythmics vs Implantable Defibrillator study. Cardiac Arrest Study Hamburg. Canadian Implantable Defibrillator Study. Eur Heart J. 2000; 21:2071-8. https://pubmed.ncbi.nlm.nih.gov/11102258
424. The Antiarrhythmics versus Implantable Defibrillators (AVID) Investigators. A comparison of antiarrhythmic-drug therapy with implantable defibrillators in patients resuscitated from near-fatal ventricular arrhythmias. N Engl J Med. 1997; 337:1576-83. https://pubmed.ncbi.nlm.nih.gov/9411221
425. Connolly SJ, Gent M, Roberts RS et al. Canadian implantable defibrillator study (CIDS) : a randomized trial of the implantable cardioverter defibrillator against amiodarone. Circulation. 2000; 101:1297-302. https://pubmed.ncbi.nlm.nih.gov/10725290
426. Hallstrom AP, McAnulty JH, Wilkoff BL et al. Patients at lower risk of arrhythmia recurrence: a subgroup in whom implantable defibrillators may not offer benefit. Antiarrhythmics Versus Implantable Defibrillator (AVID) Trial Investigators. J Am Coll Cardiol. 2001; 37:1093-9. https://pubmed.ncbi.nlm.nih.gov/11263614
427. Gregoratos G, Cheitlin MD, Conill A et al. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). J Am Coll Cardiol. 1998; 31:1175-209. https://pubmed.ncbi.nlm.nih.gov/9562026
429. Johne A, Brockmoller J, Bauer S et al. Pharmacokinetic interaction of digoxin with an herbal extract from St John’s wort (Hypericum perforatum). Clin Pharmacol Ther. 1999; 66:338-45. https://pubmed.ncbi.nlm.nih.gov/10546917
430. Ruschitzka F, Meier PJ, Turina M et al. Acute heart transplant rejection due to Saint John’s wort. Lancet. 2000; 355:548-9. https://pubmed.ncbi.nlm.nih.gov/10683008
431. Wyeth Pharmaceuticals. Cordarone (amiodarone hydrochloride) medication guide. Philadelphia, PA; 2008 Apr.
432. Yamreudeewong W, DeBisschop M, Martin LG, Lower DL. Potentially significant drug interactions of class III antiarrhythmic drugs. Drug Safety. 2003; 26:421-38. https://pubmed.ncbi.nlm.nih.gov/12688833
433. Gate Pharmaceuticals. Orap (pimozide) tablets prescribing information. Sellersville, PA; 2004 Jun.
434. Schering-Plough. Avelox (moxifloxacin hydrochloride) tablets and injection prescribing information. Kenilworth, NJ; 2005 Dec.
435. Bayer HealthCare Pharmaceuticals Inc. Cipro (ciprofloxacin hydrochloride) tablets and Cipro (ciprofloxacin) for oral suspension prescribing information. Whippany, NJ; 2015 Feb.
436. Oscient Pharmaceuticals. Factive (gemifloxacin mesylate) tablets prescribing information. Waltham, MA; 2004 Aug.
437. Pfizer Inc. Geodon (ziprasidone hydrochloride) capsules and injection prescribing information. New York, NY; 2005 May.
438. Aventis Pharmaceuticals Inc. Anzemet (dolasetron mesylate) tablets prescribing information. Kansas City, MO; 2005 Jun.
439. Desnick RJ, Brady R, Barranger J et al. Fabry disease, an under-recognized multisystemic disorder: expert recommendations for diagnosis, management, and enzyme replacement therapy. Ann Intern Med. 2003; 138:338-46.
441. Eigel B. (American Heart Association, Dallas, TX): Personal communication; 2006 Apr 13.
442. Antman EM, Anbe DT, Armstrong PW et al. ACC/AHA guidelines for the management of patients with ST-elevation myocardial infarction; A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee to Revise the 1999 Guidelines for the Management of patients with acute myocardial infarction). J Am Coll Cardiol. 2004; 44:671-719. https://pubmed.ncbi.nlm.nih.gov/15358045
443. Upsher-Smith Laboratories, Inc. Pacerone (amiodarone hydrochloride) tablets prescribing information. Minneapolis, MN. 2006 Apr.
444. SmithKline Beecham Pharmaceuticals. Halfan (halofantrine hydrochloride) tablets prescribing information. Philadelphia, PA. 2001 Oct.
445. Larsen PR, Kronenberg HM, Melmed S et al. Williams Textbook of Endocrinology. 10th ed. Philadelphia, PA: Saunders, 2003. 354, 411-2.
446. Basaria S, Cooper DS. Amiodarone and the thyroid. Am J Med. 2005; 118:706-14. https://pubmed.ncbi.nlm.nih.gov/15989900
447. Field JM, Hazinski MF, Gilmore D, eds. Handbook of emergency cardiovascular care: for healthcare providers. Dallas, TX: American Heart Association; 2006:89.
448. Food and Drug Administration. Information for healthcare professionals: Simvastatin (marketed as Zocor and generics), ezetimibe/simvastatin (marketed as Vytorin), niacin extended-release/simvastatin (marketed as Simcor), used with amiodarone (Cordarone, Pacerone). 2008 Aug 8. Accessed 2008 Aug 12. http://www.fda.gov/Drugs/DrugSafety/PostmarketDrugSafetyInformationforPatientsandProviders/ucm124362.htm
449. Schmidt GA, Hoehns JD, Purcell JL et al. Severe rhabdomyolysis and acute renal failure secondary to concomitant use of simvastatin, amiodarone, and atazanavir. J Am Board Fam Med. 2007 Jul-Aug; 20:411-6.
450. Ricaurte B, Guirguis A, Taylor HC et al. Simvastatin-amiodarone interaction resulting in rhabdomyolysis, azotemia, and possible hepatotoxicity. Ann Pharmacother. 2006; 40:753-7. https://pubmed.ncbi.nlm.nih.gov/16537817
451. Roten L, Schoenenberger RA, Krähenbühl S et al. Rhabdomyolysis in association with simvastatin and amiodarone. Ann Pharmacother. 2004; 38:978-81. https://pubmed.ncbi.nlm.nih.gov/15069169
453. US Food and Drug Administration. FDA drug safety communication: FDA warns of serious slowing of the heart rate when antiarrhythmic drug amiodarone is used with hepatitis C treatments containing sofosbuvir (Harvoni) or Sovaldi in combination with another direct acting antiviral. 2015 Mar 24. From FDA website. http://www.fda.gov/downloads/Drugs/DrugSafety/UCM439492.pdf
454. Gilead Sciences, Inc. Harvoni (ledipasvir and sofosbuvir) tablets prescribing information. Foster City, CA; 2015 Mar.
455. Gilead Sciences, Inc. Sovaldi (sofosbuvir) tablets prescribing information. Foster City, CA; 2015 Mar.
456. Janssen Therapeutics. Olysio (simeprevir) capsules prescribing information. Titusville, NJ; 2015 Apr.
457. Bristol-Myers Squibb Company. Daklinza (daclatasvir) tablets prescribing information. Princeton, NJ; 2015 Jul.
458. AbbVie, Inc. Viekira Pak (ombitasvir, paritaprevir, and ritonavir copackaged with dasabuvir ) tablets prescribing information. North Chicago, IL; 2015 Mar.
459. Valdes SO, Donoghue AJ, Hoyme DB et al. Outcomes associated with amiodarone and lidocaine in the treatment of in-hospital pediatric cardiac arrest with pulseless ventricular tachycardia or ventricular fibrillation. Resuscitation. 2014; 85:381-6. https://pubmed.ncbi.nlm.nih.gov/24361455
460. ASHP. Standardize 4 Safety: pediatric continuous infusion standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
461. ASHP. Standardize 4 Safety: adult continuous infusion standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
462. ASHP. Standardize 4 Safety: compounded oral liquid standard. Updated 2024 Mar. From ASHP website. Updates may be available at ASHP website. https://www.ashp.org/standardize4safety
463. Nahata MC. Stability of amiodarone in an oral suspension stored under refrigeration and at room temperature. Ann Pharmacother. 1997 Jul-Aug;31(7-8):851-2. doi: 10.1177/106002809703100707. PMID: 9220043.
464. Nahata MC, Morosco RS, Hipple TF. Stability of amiodarone in extemporaneous oral suspensions prepared from commercially available vehicles. J Pediatr Pharm Pract. 1999; 4:186-9.
500. Link MS, Berkow LC, Kudenchuk PJ et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132(18 Suppl 2):S444-64.
501. Neumar RW, Otto CW, Link MS et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18 Suppl 3):S729-67.
502. de Caen AR, Berg MD, Chameides L et al. Part 12: Pediatric Advanced Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132(18 Suppl 2):S526-42. https://pubmed.ncbi.nlm.nih.gov/26473000
503. Kleinman ME, Chameides L, Schexnayder SM et al. Part 14: pediatric advanced life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18 Suppl 3):S876-908.
700. Page RL, Joglar JA, Caldwell MA et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016; 67:e27-e115.
701. January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1-76. https://pubmed.ncbi.nlm.nih.gov/24685669
c. Trissel LA. Handbook of injectable drugs. 17th ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2013:80-4.
h. Eigel B. (American Heart Association, Dallas, TX): Personal communication; 2006 Apr 13.
Related/similar drugs
Cardizem
Cardizem is used to treat hypertension (high blood pressure), angina (chest pain), and heart rhythm ...
Adenosine
Adenosine is used for atrial tachycardia, radionuclide myocardial perfusion study, supraventricular ...
Botox
Botox is used for cosmetic purposes and to treat overactive bladder symptoms, urinary incontinence ...
Propafenone
Propafenone is used for atrial fibrillation, atrial flutter, ventricular tachycardia ...
Phenylephrine
Oral and nasal phenylephrine are used as nasal decongestants to temporarily unblock a nose or ...
Flecainide
Flecainide is used for atrial fibrillation, atrial flutter, paroxysmal supraventricular ...
Verapamil
Verapamil is used to treat hypertension (high blood pressure), angina (chest pain), and certain ...
Bisoprolol
Bisoprolol belongs to a group of drugs called beta-blockers and is used to treat hypertension (high ...
More about amiodarone
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (95)
- Drug images
- Latest FDA alerts (4)
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
Patient resources
Professional resources
Other brands
Pacerone, Cordarone, Nexterone