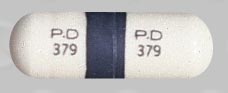
Chloramphenicol Dosage
Applies to the following strengths: 250 mg; 1000 mg; palmitate
Usual Adult Dose for:
- Bacteremia
- Meningitis
- Rickettsial Infection
- Bacterial Infection
- Cystic Fibrosis
- Typhoid Fever
- Gram Negative Infection
- Psittacosis
- Ornithosis
- Inhalation Bacillus anthracis
- Cutaneous Bacillus anthracis
- Plague
- Tularemia
Usual Pediatric Dose for:
- Bacteremia
- Meningitis
- Rickettsial Infection
- Bacterial Infection
- Cystic Fibrosis
- Typhoid Fever
- Gram Negative Infection
- Psittacosis
- Ornithosis
- Inhalation Bacillus anthracis
- Cutaneous Bacillus anthracis
- Plague
- Tularemia
Additional dosage information:
Usual Adult Dose for Bacteremia
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Meningitis
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Rickettsial Infection
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Bacterial Infection
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Cystic Fibrosis
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Typhoid Fever
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Gram Negative Infection
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Psittacosis
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Ornithosis
12.5 to 25 mg/kg IV every 6 hours
Comments:
- Most susceptible microorganisms will respond to the blood levels achieved with 50 mg/kg/day.
- In exceptional cases, infections due to moderately-resistant organisms may require up to 100 mg/kg/day to reach blood levels that inhibit the pathogen; such high doses should be reduced as soon as possible.
- According to some authorities: When used to treat typhoid fever, this drug should be administered at therapeutic levels for 8 to 10 days after patient is afebrile to reduce risk of relapse.
- This drug should be switched to an oral formulation of another appropriate antibacterial agent as soon as feasible.
- This drug is not recommended for routine treatment of typhoid carrier state.
Uses:
- Acute infections due to Salmonella typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; Haemophilus influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
Infectious Diseases Society of America (IDSA) Recommendations for Bacterial Meningitis: 1 to 1.5 g IV every 6 hours
Comments:
- Recommended as alternative therapy for bacterial meningitis due to Neisseria meningitidis, Haemophilus influenzae, or Streptococcus pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- Higher dose recommended for pneumococcal meningitis.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Inhalation Bacillus anthracis
US CDC Recommendations: 1 g IV every 6 to 8 hours
Duration of Therapy: At least 2 to 3 weeks or until patient is clinically stable (whichever is longer)
- Patients exposed to aerosolized spores will require prophylaxis with a different agent to complete an antimicrobial regimen of 60 days from onset of illness.
Comments:
- This drug should only be used if other options are not available, due to toxicity concerns.
- Recommended as an alternative protein synthesis inhibitor for use with a bactericidal fluoroquinolone plus a bactericidal beta-lactam for systemic anthrax with possible/confirmed meningitis
- Systemic anthrax includes anthrax meningitis; inhalation, injection, and gastrointestinal anthrax; and cutaneous anthrax with systemic involvement, extensive edema, or lesions of the head or neck.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Cutaneous Bacillus anthracis
US CDC Recommendations: 1 g IV every 6 to 8 hours
Duration of Therapy: At least 2 to 3 weeks or until patient is clinically stable (whichever is longer)
- Patients exposed to aerosolized spores will require prophylaxis with a different agent to complete an antimicrobial regimen of 60 days from onset of illness.
Comments:
- This drug should only be used if other options are not available, due to toxicity concerns.
- Recommended as an alternative protein synthesis inhibitor for use with a bactericidal fluoroquinolone plus a bactericidal beta-lactam for systemic anthrax with possible/confirmed meningitis
- Systemic anthrax includes anthrax meningitis; inhalation, injection, and gastrointestinal anthrax; and cutaneous anthrax with systemic involvement, extensive edema, or lesions of the head or neck.
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Plague
US CDC Recommendations: 25 mg/kg IV every 6 hours
Duration of therapy: 10 to 14 days (or until 2 days after fever subsides)
Comments:
- Recommended as an alternative regimen for the treatment of plague
- IV therapy should be started as soon as plague suspected; may switch to oral therapy once patient improves
- Current guidelines should be consulted for additional information.
Usual Adult Dose for Tularemia
Working Group on Civilian Biodefense Recommendations: 15 mg/kg IV 4 times a day
Duration of therapy: 14 to 21 days
Comments:
- Recommended as an alternative regimen for the treatment of tularemia in a contained-casualty setting
- May switch to oral therapy when clinically indicated
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Bacteremia
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Meningitis
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Rickettsial Infection
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Bacterial Infection
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Cystic Fibrosis
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Typhoid Fever
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Gram Negative Infection
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Psittacosis
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Ornithosis
Premature neonates and full-term neonates under 2 weeks of age: 6.25 mg/kg IV every 6 hours
Full-term neonates at least 2 weeks of age: Up to 12.5 mg/kg IV every 6 hours
Children: 12.5 to 25 mg/kg IV every 6 hours
Comments:
- NEONATES:
- A total of 25 mg/kg/day generally produces and maintains levels in blood and tissues sufficient to control most indicated infections; increased dose in these patients (required by severe infections) should be administered only to maintain blood level within a therapeutically effective range.
- After the first 2 weeks of life, full-term neonates typically may receive up to 50 mg/kg/day.
- These dosing recommendations are extremely important as blood level in all premature and full-term neonates under 2 weeks of age differs from blood level in other infant neonates; such difference is due to variations in maturity of the metabolic functions of the liver and kidneys.
- CHILDREN:
- A total of 50 mg/kg/day produces blood levels effective against most susceptible organisms.
- Severe infections (e.g., bacteremia, meningitis), particularly with sufficient CSF levels are desired, may require up to 100 mg/kg/day; dose should be reduced to 50 mg/kg/day as soon as possible.
Uses:
- Acute infections due to S typhi
- Serious infections due to susceptible strains of the following organisms when less potentially hazardous agents are ineffective/contraindicated: Salmonella species; H influenzae (especially meningeal infections); Rickettsia; lymphogranuloma-psittacosis group; various gram-negative bacteria causing bacteremia, meningitis, other serious gram-negative infections; other susceptible organisms which have shown resistance to all other appropriate antibacterial agents
- Cystic fibrosis regimens
American Academy of Pediatrics (AAP) Recommendations:
1 month or older: 12.5 to 25 mg/kg IV 4 times a day
IDSA Recommendations for Bacterial Meningitis:
Neonates 0 to 7 days: 25 mg/kg IV every 24 hours
Neonates 8 to 28 days: 50 mg/kg/day IV in divided doses every 12 to 24 hours
Infants and children: 18.75 to 25 mg/kg IV every 6 hours
Comments:
- AAP: Reserved for serious infections (due to rare risk of aplastic anemia); IV is preferred over oral as oral may increase risk of aplastic anemia.
- AAP: Dose should be adjusted based on target serum levels (15 to 25 mg/L).
- IDSA: Recommended as alternative therapy for bacterial meningitis due to N meningitidis, H influenzae, or S pneumoniae (penicillin MIC less than 0.1 mcg/mL)
- IDSA: Smaller doses and longer dosing intervals may be advisable for very low birth weight neonates (less than 2 kg).
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Inhalation Bacillus anthracis
AAP Recommendations:
Neonates up to 4 weeks of age:
- Gestational age 32 to 37 weeks and term neonate, up to 1 week of age: 25 mg/kg IV every 24 hours
- Gestational age 32 to 37 weeks and term neonate, 1 to 4 weeks of age: 25 mg/kg IV every 12 hours
Children 1 month or older: 25 mg/kg IV every 6 hours
Duration of Therapy: At least 2 to 3 weeks or until patient is clinically stable (whichever is longer)
- Patients will require prophylaxis with a different agent to complete an antimicrobial regimen of up to 60 days from onset of illness.
Comments:
- This drug should only be used if other options are not available, due to toxicity concerns; serum drug levels should be obtained in neonates, if possible.
- Recommended as an alternative protein synthesis inhibitor for use with a bactericidal fluoroquinolone plus a bactericidal beta-lactam (or glycopeptide in children 1 month or older) for severe/systemic anthrax with possible/confirmed meningitis
- Systemic/severe anthrax includes anthrax meningitis, inhalation anthrax, injection anthrax, gastrointestinal anthrax, and cutaneous anthrax with systemic involvement, extensive edema, or lesions of the head or neck.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Cutaneous Bacillus anthracis
AAP Recommendations:
Neonates up to 4 weeks of age:
- Gestational age 32 to 37 weeks and term neonate, up to 1 week of age: 25 mg/kg IV every 24 hours
- Gestational age 32 to 37 weeks and term neonate, 1 to 4 weeks of age: 25 mg/kg IV every 12 hours
Children 1 month or older: 25 mg/kg IV every 6 hours
Duration of Therapy: At least 2 to 3 weeks or until patient is clinically stable (whichever is longer)
- Patients will require prophylaxis with a different agent to complete an antimicrobial regimen of up to 60 days from onset of illness.
Comments:
- This drug should only be used if other options are not available, due to toxicity concerns; serum drug levels should be obtained in neonates, if possible.
- Recommended as an alternative protein synthesis inhibitor for use with a bactericidal fluoroquinolone plus a bactericidal beta-lactam (or glycopeptide in children 1 month or older) for severe/systemic anthrax with possible/confirmed meningitis
- Systemic/severe anthrax includes anthrax meningitis, inhalation anthrax, injection anthrax, gastrointestinal anthrax, and cutaneous anthrax with systemic involvement, extensive edema, or lesions of the head or neck.
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Plague
US CDC Recommendations:
Children over 2 years: 25 mg/kg IV every 6 hours
Maximum dose: 4 g/day
Duration of therapy: 10 to 14 days (or until 2 days after fever subsides)
Comments:
- Recommended as an alternative regimen for the treatment of plague
- IV therapy should be started as soon as plague suspected; may switch to oral therapy once patient improves
- Current guidelines should be consulted for additional information.
Usual Pediatric Dose for Tularemia
Working Group on Civilian Biodefense Recommendations:
Children: 15 mg/kg IV 4 times a day
Duration of therapy: 14 to 21 days
Comments:
- Recommended as an alternative regimen for the treatment of tularemia in a contained-casualty setting
- May switch to oral therapy when clinically indicated
- Current guidelines should be consulted for additional information.
Renal Dose Adjustments
Renal dysfunction: Dose adjustments may be required; however, no specific guidelines have been suggested.
Comments:
- The dose should be based on serum drug levels.
- When metabolic functions of the kidneys are immature/seriously impaired, high drug levels are attained which tend to increase with successive doses.
- Children with renal dysfunction may retain excessive amounts of this drug.
Liver Dose Adjustments
Liver dysfunction: Dose adjustments may be required; however, no specific guidelines have been suggested.
Comments:
- The dose should be based on serum drug levels.
- When metabolic functions of the liver are immature/seriously impaired, high drug levels are attained which tend to increase with successive doses.
- Children with liver dysfunction may retain excessive amounts of this drug.
Dose Adjustments
Adults with impaired metabolic processes: Dose should be adjusted accordingly; blood level should be determined at appropriate intervals.
Pediatric patients with immature metabolic processes: In young infants and other pediatric patients with suspected immature metabolic functions, a total of 25 mg/kg/day generally produces therapeutic drug levels in the blood; the blood level of this drug should be carefully monitored in these patients.
Precautions
US BOXED WARNING:
- BLOOD DYSCRASIAS: Serious and fatal blood dyscrasias (aplastic anemia, hypoplastic anemia, thrombocytopenia, granulocytopenia) reported after use of this drug; reports of drug-related aplastic anemia ended in leukemia. Blood dyscrasias reported after both short-term and prolonged therapy. This drug must not be used when less potentially hazardous agents will be effective and are not contraindicated. This drug must not be used to treat trivial infections or when it is not indicated (e.g., colds, influenza, throat infections); it must not be used as a prophylactic agent to prevent bacterial infections. It is crucial that adequate blood studies be conducted during therapy with this drug; while blood studies may detect early peripheral blood changes (e.g., leukopenia, reticulocytopenia, granulocytopenia) before they become irreversible, these studies cannot be relied upon to detect bone marrow depression before development of aplastic anemia. To enable appropriate studies and observation during therapy, it is preferable for patients to be hospitalized.
CONTRAINDICATIONS:
- History of previous hypersensitivity and/or toxic reaction to this drug
- For use in the treatment of trivial infections or where it is not indicated (e.g., colds, influenza, throat infections)
- As a prophylactic agent to prevent bacterial infections
Consult WARNINGS section for additional precautions.
Dialysis
Data not available
Other Comments
Administration advice:
- Reserve for serious infections due to susceptible organisms when less potentially dangerous therapeutic agents are ineffective/contraindicated.
- Intended for IV use only (ineffective when administered IM); inject as 10% solution IV over at least 1 minute.
- Switch patients started on this IV drug to the oral formulation of another appropriate antibacterial as soon as clinically feasible.
- If possible, avoid repeated courses of this drug; do not continue therapy longer than necessary to cure the infection with little/no risk of relapse.
General:
- Sensitivity testing is vital to determine indicated use but may be done at the same time therapy is started if clinical judgment is that an indicated condition exists; this drug should be discontinued as soon as possible if sensitivity testing indicates less potentially hazardous agents are effective.
- The decision to continue using this drug instead of another antibacterial when in vitro studies indicate both are effective against a specific pathogen should be based on severity of infection, susceptibility of pathogen to the various antimicrobial agents, efficacy of the various agents in the infection, and consideration of potential side effects.
- Sodium content is about 52 mg (2.25 mEq)/g of this drug.
Monitoring:
- General: Drug levels in blood
- Hematologic: Blood studies (at baseline and about every 2 days during therapy)
- Renal: Renal function in elderly patients
More about chloramphenicol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (2)
- Side effects
- During pregnancy
- Drug class: miscellaneous antibiotics
- Breastfeeding
Patient resources
Other brands
Chloromycetin Sodium Succinate
Professional resources
Other brands
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.