Ethinyl estradiol/levonorgestrel Disease Interactions
There are 24 disease interactions with ethinyl estradiol / levonorgestrel.
- Smoking
- Abnormal genital bleeding
- Abnormal vaginal bleeding
- Carcinomas (estrogenic)
- Hypercalcemia in breast cancer
- Hypertension
- Thromboembolism/cardiovascular
- Hepatic neoplasms
- Breast malignancy
- Liver disease
- Angioedema
- Gallbladder disease
- Hypercalcemia
- Hyperlipidemia
- Liver disease
- Melasma
- Depression
- Fluid retention
- Glucose intolerance
- Retinal thrombosis
- Thyroid function tests
- Cardiovascular disease
- Hyperlipidemia
- Weight gain
Combined oral contraceptives (applies to ethinyl estradiol/levonorgestrel) smoking
Major Potential Hazard, Moderate plausibility.
Cigarette smoking increases the risk of serious cardiovascular events from estrogen-containing combination oral contraceptives (COC). This risk increases with age, particularly in females over 35 years of age, and with the number of cigarettes smoked. For this reason, COCs are contraindicated in females who are over 35 years of age and smoke.
Contraceptives (applies to ethinyl estradiol/levonorgestrel) abnormal genital bleeding
Major Potential Hazard, Moderate plausibility. Applicable conditions: Abnormal Uterine Bleeding
The use of contraceptives is contraindicated when there is an undiagnosed abnormal genital bleeding. Adequate diagnostic measures should be undertaken to rule out the presence of any malignancy.
Estrogens (applies to ethinyl estradiol/levonorgestrel) abnormal vaginal bleeding
Major Potential Hazard, High plausibility. Applicable conditions: Abnormal Uterine Bleeding
The use of estrogens is contraindicated in patients with undiagnosed, abnormal vaginal bleeding. Prolonged (> 1 year), unopposed estrogen use (i.e. estrogen without concomitant progestin therapy) has been associated with a significant, dose-related risk of endometrial carcinoma. The risk may be offset substantially by the addition of a progestin but may not be completely abolished. Prior to initiating estrogen therapy, appropriate diagnostic tests should be performed in patients with abnormal vaginal bleeding to rule out endometrial malignancy. The same applies if recurrent or persistent bleeding develops during estrogen therapy.
Estrogens (applies to ethinyl estradiol/levonorgestrel) carcinomas (estrogenic)
Major Potential Hazard, High plausibility. Applicable conditions: Neoplasia -- Estrogen Dependent
The use of estrogens is generally contraindicated in patients with known or suspected estrogen-dependent neoplasia such as breast and endometrial cancer, since it may stimulate tumor proliferation. High dosages of estrogens may be used for the palliative treatment of inoperable, metastatic breast cancer, but only in appropriately selected men and postmenopausal women.
Estrogens (applies to ethinyl estradiol/levonorgestrel) hypercalcemia in breast cancer
Major Potential Hazard, Moderate plausibility.
When treated with an estrogen, patients with breast cancer and bone metastases may develop severe hypercalcemia, in which case the drug should be stopped and measures be taken to reduce serum calcium levels.
Estrogens (applies to ethinyl estradiol/levonorgestrel) hypertension
Major Potential Hazard, High plausibility.
The risk of myocardial infarction and strokes, including those associated with oral contraceptive use and some estrogen use, is increased in patients with hypertension. Moreover, estrogens (and progestogens) may elevate blood pressure and worsen the hypertension, thus compounding the risk. Clinically significant blood pressure increases have been reported during estrogen therapy, particularly in patients receiving high dosages or treated with oral contraceptive combinations having high progestational activity. These effects also increase with duration of therapy and patient age. Therapy with estrogens should be administered cautiously in patients with preexisting hypertension. Patients should be monitored for changes in cardiovascular status, and their antihypertensive regimen adjusted or estrogen therapy withdrawn as necessary. In patients requiring contraception, alternative methods should be considered for those who are hypertensive, over age 35, and smoke.
Estrogens (applies to ethinyl estradiol/levonorgestrel) thromboembolism/cardiovascular
Major Potential Hazard, Moderate plausibility. Applicable conditions: Migraine, History - Thrombotic/Thromboembolic Disorder, Cerebral Vascular Disorder, Thrombotic/Thromboembolic Disorder, Ischemic Heart Disease
The use of estrogens is considered by manufacturers and some authorities to be contraindicated in patients with active thrombotic or thromboembolic disorders. The use of estrogen-containing oral contraceptives is additionally deemed contraindicated in patients with a history of such disorders and/or current cerebrovascular or coronary artery disease. Females with a history of migraines with aura are at an increased risk for stroke and this stroke risk may be further increased in females who have migraines with aura with use of combination oral contraceptives. Hypercoagulability and changes in various clotting factors and blood components have been observed in women receiving estrogen therapy. Although the clinical significance of these effects is unknown, epidemiological data suggest it may be dose-dependent. The risk is probably slight with the use of newer, low-dose oral contraceptives in the absence of known risk factors (e.g., smoker, particularly over the age of 35; hypertension; hyperlipidemia; obesity; diabetes; age over 40). However, a much more significant risk has been reported with higher dosages, such as those used to treat prostate or metastatic breast cancer or those used in older formulations of birth control pills. Therapy with estrogens should be administered cautiously in the lowest effective dosage and only after careful consideration of risks and benefits. Estrogens should be avoided in patients with a history of thrombotic and thromboembolic disorders associated with estrogen use, except when used in the treatment of breast or prostatic malignancy.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) hepatic neoplasms
Major Potential Hazard, High plausibility. Applicable conditions: Hepatic Tumor, Hepatic Tumor
The use of oral contraceptives is contraindicated in patients with liver tumors. An increased risk of benign hepatic adenomas and hepatocellular carcinomas has been associated with long-term, oral estrogen- progestin contraceptive use of at least 4 years and 8 years, respectively. Although these tumors are rare and have not been reported with other types of estrogen or progestogen therapies, any preparation containing estrogens and/or progestogens should probably be avoided in patients with existing tumors of the liver. Hepatic hemangiomas and nodular hyperplasia of the liver have been reported with isolated estrogen therapy.
Progestogens (applies to ethinyl estradiol/levonorgestrel) breast malignancy
Major Potential Hazard, High plausibility. Applicable conditions: Breast Cancer
The use of progestogens is considered by manufacturers to be contraindicated in patients with existing or suspected malignancy of the breast. Some supportive data are available for medroxyprogesterone. Specifically, medroxyprogesterone treatment may be associated with breast cancer, primarily when the drug is administered intramuscularly. A pooled analysis of two case-control studies, one from the World Health Organization and the other from New Zealand, revealed a small overall relative risk of breast cancer in women who have ever used intramuscular medroxyprogesterone acetate. The relative risk was higher in the subgroup of women who had initiated therapy within the previous 5 years. Thus, an increased risk (approximately 2-fold) is associated with intramuscular medroxyprogesterone use in the first 5 years. A more recent U.S. study also found a statistically significant increase in breast cancer risk among recent users (defined as last use within the past five years) who used depo-medroxyprogesterone acetate for 12 months or longer.
Progestogens (applies to ethinyl estradiol/levonorgestrel) liver disease
Major Potential Hazard, High plausibility.
The use of progestogens, in general, is contraindicated in patients with impaired hepatic function or liver disease. There are little or no data concerning the pharmacokinetic disposition of the different progestogens in patients with hepatic disease. However, most hormones, including progestational hormones, are known to be extensively metabolized by the liver. Medroxyprogesterone should not be used by women with significant liver disease and should be discontinued if jaundice or disturbances of liver function occur.
Estrogens (applies to ethinyl estradiol/levonorgestrel) angioedema
Moderate Potential Hazard, Moderate plausibility.
The use of exogenous estrogens may induce or exacerbate symptoms of angioedema, particularly in women with hereditary angioedema. Close monitoring is recommended when prescribing these agents to patients predisposed to angioedema.
Estrogens (applies to ethinyl estradiol/levonorgestrel) gallbladder disease
Moderate Potential Hazard, Moderate plausibility.
A two- to four-fold increase in risk of gallbladder disease has been noted in women receiving postmenopausal estrogen therapy. The risk for gallbladder disease may be less for premenopausal women using oral contraceptives containing low-dose estrogens and/or progestins. Therapy with estrogens should be administered cautiously in patients with preexisting gallbladder disease.
Estrogens (applies to ethinyl estradiol/levonorgestrel) hypercalcemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperparathyroidism, Renal Dysfunction
Estrogens influence the metabolism of calcium and phosphorus. Intestinal absorption and retention of calcium are increased, which may occasionally result in hypercalcemia. Therapy with estrogens should be administered cautiously in patients with preexisting hypercalcemia, renal dysfunction, or metabolic bone diseases that are associated with hypercalcemia.
Estrogens (applies to ethinyl estradiol/levonorgestrel) hyperlipidemia
Moderate Potential Hazard, Moderate plausibility.
Although estrogens have generally favorable effects on plasma lipids, including increases in HDL and decreases in total cholesterol and LDL, they have also been associated with significant elevations in triglyceride levels, particularly when high dosages are used. Severe hyperlipidemia is known to sometimes cause pancreatitis. Patients with preexisting hyperlipidemia may require closer monitoring during estrogen therapy, and adjustments made accordingly in their lipid-lowering regimen.
Estrogens (applies to ethinyl estradiol/levonorgestrel) liver disease
Moderate Potential Hazard, High plausibility.
Estrogens are primarily metabolized by the liver. Patients with impaired hepatic function may be at increased risk for adverse effects associated with estrogen administration due to decreased drug clearance. Therapy with estrogens should be administered cautiously in patients with liver disease. In addition, clinicians should be aware that estrogen therapy may affect liver function tests. Increased sulfobromophthalein retention has been reported with the use of estrogen-containing oral contraceptives and may be expected with larger doses of estrogens.
Estrogens (applies to ethinyl estradiol/levonorgestrel) melasma
Moderate Potential Hazard, Moderate plausibility.
The use of exogenous estrogens may occasionally cause chloasma, especially in women with a history of chloasma gravidarum. Women with a tendency to chloasma should avoid exposure to the sun or ultraviolet radiation while taking combination oral contraceptives.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) depression
Moderate Potential Hazard, Moderate plausibility.
The use of oral contraceptives has been associated with an increased incidence of depression. It is uncertain whether this effect is related to the estrogenic or the progestogenic component of the contraceptive, although excess progesterone activity is associated with depression. Patients with a history of depression receiving estrogen and/or progestogen therapy should be followed closely. The manufacturer of medroxyprogesterone recommends monitoring patients who have a history of depression and to not re- administer medroxyprogesterone if depression recurs.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) fluid retention
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Migraine, Asthma, Seizures, Congestive Heart Failure, Renal Dysfunction, Renal Dysfunction, Migraine, Asthma, Seizures, Congestive Heart Failure, Hypertension
Estrogens and progestogens may cause fluid retention, particularly when given in high dosages or for prolonged periods. Therapy with these agents should be administered cautiously in patients who have preexisting problems with excess fluid. In addition, patients with conditions that may be adversely affected by fluid accumulation, such as asthma, epilepsy, migraine, and cardiovascular or renal dysfunction, should be observed for exacerbation of their condition during estrogen and/or progestogen therapy.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) glucose intolerance
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus, Diabetes Mellitus
Impaired glucose tolerance has been observed in some patients administered oral contraceptives and appears to be related primarily to the estrogen dose. However, progestogens can increase insulin secretion and produce insulin resistance to varying degrees, depending on the agent. Patients with diabetes mellitus should be monitored more closely during therapy with estrogens and/or progestogens, and adjustments made accordingly in their antidiabetic regimen.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) retinal thrombosis
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Visual Defect/Disturbance, Visual Defect/Disturbance
Estrogens and progestogens may cause retinal thrombosis. Oral contraceptives should be discontinued if there is unexplained partial or complete loss of vision; onset of proptosis or diplopia; papilledema; or retinal vascular lesions. Therapy with these agents should be administered cautiously in patients who have preexisting ocular problems and appropriate diagnostic and therapeutic measures should be instituted. Contact lens wearers who develop visual changes or changes in lens tolerance should be assessed by an ophthalmologist.
Estrogens/progestogens (applies to ethinyl estradiol/levonorgestrel) thyroid function tests
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Thyroid Disease, Thyroid Disease
When administering estrogen and/or progestogen therapy in patients with thyroid disorders, clinicians should be aware that these hormones may affect thyroid function tests. Changes have mostly been reported with the use of combination oral contraceptives. Specifically, thyroid-binding globulin (TBG) may be increased, resulting in elevated circulating total thyroid hormone, as measured by PBI (protein-bound iodine), T4 by column or radioimmunoassay, or T3 by radioimmunoassay. Free T3 resin uptake may be decreased. On the contrary, a decrease in TBG and, consequently, thyroxine concentration, has been reported by the manufacturers of the progestin-only (norethindrone) oral contraceptives.
Levonorgestrel (applies to ethinyl estradiol/levonorgestrel) cardiovascular disease
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Cerebral Vascular Disorder, History - Thrombotic/Thromboembolic Disorder, Thrombotic/Thromboembolic Disorder
The use of levonorgestrel requires careful assessment and caution in conditions of arterial disease, including stroke and myocardial infarction, and also, in patients with increased blood pressure and coagulopathies.
Progestogens (applies to ethinyl estradiol/levonorgestrel) hyperlipidemia
Moderate Potential Hazard, Moderate plausibility.
Some progestogenic agents may elevate plasma LDL levels and/or lower HDL levels, although data have been inconsistent. Patients with preexisting hyperlipidemia may require closer monitoring during progestogen therapy, and adjustments made accordingly in their lipid-lowering regimen.
Progestogens (applies to ethinyl estradiol/levonorgestrel) weight gain
Minor Potential Hazard, Moderate plausibility. Applicable conditions: Obesity
Progestogens can cause weight gain, which may be significant (as is the case with parenteral medroxyprogesterone) and undesirable in obese patients attempting to lose weight.
Switch to professional interaction data
Ethinyl estradiol/levonorgestrel drug interactions
There are 501 drug interactions with ethinyl estradiol / levonorgestrel.
Ethinyl estradiol/levonorgestrel alcohol/food interactions
There are 9 alcohol/food interactions with ethinyl estradiol / levonorgestrel.
More about ethinyl estradiol / levonorgestrel
- ethinyl estradiol/levonorgestrel consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (5,089)
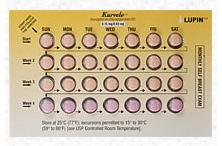
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: contraceptives
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.