Brexpiprazole Disease Interactions
There are 14 disease interactions with brexpiprazole.
- Suicidality
- Dementia
- NMS
- Aspiration
- Seizure
- Hematologic abnormalities
- Hyperglycemia/diabetes
- Hypotension
- Lipid alterations
- Renal impairment
- Weight gain
- Hepatic impairment
- Hyperprolactinemia
- Tardive dyskinesia
Antidepressants (applies to brexpiprazole) suicidality
Major Potential Hazard, Moderate plausibility. Applicable conditions: Depression, Bipolar Disorder
Antidepressants increased the risk of suicidal thoughts and behavior in children, adolescents, and young adults in short-term trials; these trials did not show increased risk in patients older than 24 years and risk was reduced in patients 65 years and older. Adult and pediatric patients with major depressive disorder may experience worsening of their depression and/or the emergence of suicidal ideation and behavior (suicidality) or unusual changes in behavior, whether or not they are taking antidepressants; this risk may persist until significant remission occurs. Suicide is a known risk of depression and certain other psychiatric disorders; such disorders are the strongest predictors of suicide. Patients of all ages treated with antidepressants for any indication should be monitored appropriately and observed closely for clinical worsening, suicidality, and unusual changes in behavior, especially during the first few months of drug therapy, and at times of dose changes. Family members/caregivers should be advised to monitor for changes in behavior and to notify the health care provider. Changing the therapeutic regimen (including discontinuing the medication) should be considered in patients whose depression is persistently worse, or who are experiencing emergent suicidal thoughts or behaviors.
Atypical antipsychotic agents (applies to brexpiprazole) dementia
Major Potential Hazard, High plausibility.
Antipsychotic drugs are not approved for the treatment of patients with dementia-related psychosis. Older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death; although the causes were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. A causal relationship with antipsychotic use has not been established. In controlled trials in older patients with dementia-related psychosis, patients randomized to risperidone, aripiprazole, and olanzapine had higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, compared to patients treated with placebo.
Neuroleptics (applies to brexpiprazole) NMS
Major Potential Hazard, High plausibility. Applicable conditions: Neuroleptic Malignant Syndrome
The central dopaminergic blocking effects of neuroleptic agents may precipitate or aggravate a potentially fatal symptom complex known as neuroleptic malignant syndrome (NMS). NMS is observed most frequently when high-potency agents like haloperidol are administered intramuscularly, but may occur with any neuroleptic agent given for any length of time. Clinical manifestations of NMS include hyperpyrexia, muscle rigidity, altered mental status and autonomic instability (irregular pulse or blood pressure, tachycardia, diaphoresis and cardiac arrhythmias). Additional signs may include elevated creatine phosphokinase, myoglobinuria, and acute renal failure. Neuroleptic agents should not be given to patients with active NMS and should be immediately discontinued if currently being administered in such patients. In patients with a history of NMS, introduction or reintroduction of neuroleptic agents should be carefully considered, since NMS may recur.
Antipsychotic agents (applies to brexpiprazole) aspiration
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Dysphagia
Esophageal dysmotility and aspiration have been associated with the use of antipsychotic drugs. These drugs should be administered cautiously in patients at risk for aspiration pneumonia.
Antipsychotic/neuroleptic agents (applies to brexpiprazole) seizure
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Seizures, Head Injury, Alcoholism
Antipsychotic and neuroleptic drugs can lower the seizure threshold and trigger seizures in a dose-dependent manner. This risk is greatest in patients with a history of seizures or with conditions that lower the seizure threshold. Therapy with these drugs should be administered cautiously in patients with a history of seizures or other predisposing factors, such as head trauma, CNS abnormalities, and alcoholism.
Atypical antipsychotic agents (applies to brexpiprazole) hematologic abnormalities
Moderate Potential Hazard, High plausibility. Applicable conditions: Neutropenia
Cases of leukopenia, neutropenia, and agranulocytosis have been reported with the use of atypical antipsychotic agents. Patients with preexisting low white blood cell count may be at increased risk. Therapy with these agents should be administered cautiously in patients with a history of, or predisposition to, decreased white blood cell or neutrophil counts. Clinical monitoring of hematopoietic function is recommended. At the first sign of a clinically significant decline in white blood cells, discontinuation of atypical antipsychotic therapy should be considered in the absence of other causative factors, and the patient closely monitored for fever or other signs and symptoms of infection.
Atypical antipsychotic agents (applies to brexpiprazole) hyperglycemia/diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus, Obesity
Hyperglycemia, in some cases extreme and associated with ketoacidosis or hyperosmolar coma or death, has been reported with the use of atypical antipsychotic agents. Patients with diabetes should be monitored for worsening control of blood glucose when treated with these agents. It is recommended that patients with risk factors for diabetes mellitus starting treatment with atypical antipsychotics should undergo fasting blood glucose testing at the beginning of treatment, and periodically thereafter. Any patient treated with atypical antipsychotics should be monitored for symptoms of hyperglycemia including polydipsia, polyuria, polyphagia, and weakness. Patients who develop symptoms of hyperglycemia during treatment with atypical antipsychotics should undergo fasting blood glucose testing. In some cases, hyperglycemia has resolved when treatment with these agents was discontinued; however, some patients required continuation of anti-diabetic treatment despite discontinuation of the atypical antipsychotic drug.
Atypical antipsychotic agents (applies to brexpiprazole) hypotension
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Syncope, Dehydration, Ischemic Heart Disease, Diarrhea, Vomiting, Congestive Heart Failure, History - Myocardial Infarction, Arrhythmias, Cerebrovascular Insufficiency
The use of atypical antipsychotic agents has been associated with orthostatic hypotension and syncope. Therapy with atypical antipsychotics should be administered cautiously in patients with hypotension or conditions that could be exacerbated by hypotension, such as a history of myocardial infarction, angina, or ischemic stroke. Patients with dehydration (e.g., due to severe diarrhea or vomiting) may be predisposed to hypotension and should also be managed carefully during therapy with atypical antipsychotics. Blood pressure should be monitored at regular intervals, particularly during dosage escalation or whenever dosage has been altered, and patients should be advised not to rise abruptly from a sitting or recumbent position.
Atypical antipsychotic agents (applies to brexpiprazole) lipid alterations
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperlipidemia
Atypical antipsychotic drugs have been associated with undesirable alterations in lipid levels. While all agents in the class have been shown to produce some changes, each drug has its own specific risk profile. Before or soon after initiation of antipsychotic medications, a fasting lipid profile should be obtained at baseline and monitored periodically during treatment.
Atypical antipsychotic agents (applies to brexpiprazole) renal impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
Therapy with some atypical antipsychotic agents should be administered cautiously in patients with renal impairment and the dosage should be reduced accordingly. These agents are not recommended in patients with severe renal impairment.
Atypical antipsychotic agents (applies to brexpiprazole) weight gain
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Obesity
Weight gain has been observed with atypical antipsychotic use. While all agents in the class have been shown to produce some changes, each drug has its own specific risk profile. When treating pediatric patients with atypical antipsychotic agents, weight gain should be monitored and assessed against that expected for normal growth. Monitor weight at baseline and frequently thereafter.
Brexpiprazole (applies to brexpiprazole) hepatic impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
Brexpiprazole is primarily metabolized by the liver. It is recommended to reduce the dose of brexpiprazole in patients with moderate to severe hepatic impairment (Child-Pugh score greater than or equal to 7) as these patients might have a higher exposure to brexpiprazole than patients with normal hepatic function.
Neuroleptics (applies to brexpiprazole) hyperprolactinemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Breast Cancer
The chronic use of neuroleptic agents can cause persistent elevations in prolactin levels due to antagonism of dopamine D2 receptors. Based on in vitro data, approximately one-third of human breast cancers are thought to be prolactin-dependent. The clinical significance of this observation with respect to long-term neuroleptic therapy is unknown. Chronic administration of neuroleptic drugs has been associated with mammary tumorigenesis in rodent studies but not in human clinical or epidemiologic studies. Until further data are available, therapy with neuroleptic agents should be administered cautiously in patients with a previously detected breast cancer. Caution is also advised in patients with preexisting hyperprolactinemia. Hyperprolactinemia may suppress hypothalamic gonadotrophin releasing hormone (GnRH), resulting in reduced pituitary gonadotropin secretion. This, in turn, may inhibit reproductive function by impairing gonadal steroidogenesis in both female and male patients. Galactorrhea, amenorrhea, gynecomastia, and impotence have been reported in patients receiving prolactin-elevating compounds; however, the clinical significance of elevated serum prolactin levels is unknown for most patients. Long-standing hyperprolactinemia when associated with hypogonadism may lead to decreased bone density in both female and male patients.
Neuroleptics (applies to brexpiprazole) tardive dyskinesia
Moderate Potential Hazard, High plausibility.
Tardive dyskinesia (TD) has occurred in patients treated with antipsychotic drugs; the syndrome consists of potentially irreversible, involuntary, dyskinetic movements. The risk appears highest in older patients (particularly older women) but it is not possible to predict which patients are likely to develop TD; whether antipsychotic drugs differ in their potential to cause TD is unknown. The risk of TD and the likelihood that it will become irreversible increase with the duration of therapy and the total cumulative dose. The syndrome can develop after relatively brief treatment periods, even at low dosages; it may also occur after discontinuation of therapy. TD may remit (partially or completely) upon discontinuation of antipsychotic therapy, although antipsychotic therapy itself may suppress (or partially suppress) signs/symptoms of TD, possibly masking the underlying process; the effect of symptomatic suppression on the long-term course of TD is unknown. In patients with preexisting drug-induced TD, initiating or increasing the dosage of antipsychotic therapy may temporarily mask the symptoms of TD but could eventually worsen the condition. In patients requiring chronic therapy, the lowest dose and shortest duration of therapy producing a satisfactory clinical response are recommended; the need for continued therapy should be reassessed periodically. If signs/symptoms of TD occur during antipsychotic therapy, discontinuation of the offending agent should be considered; however, some patients may require treatment despite the presence of TD.
Switch to professional interaction data
Brexpiprazole drug interactions
There are 604 drug interactions with brexpiprazole.
Brexpiprazole alcohol/food interactions
There are 4 alcohol/food interactions with brexpiprazole.
More about brexpiprazole
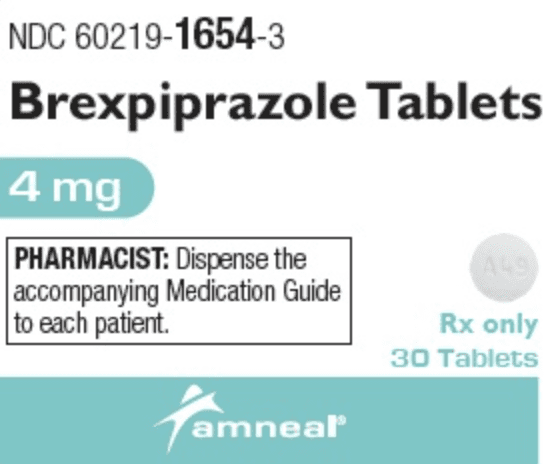
- brexpiprazole consumer information
- Check interactions
- Compare alternatives
- Reviews (536)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Drug class: atypical antipsychotics
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.