Etrafon Forte Disease Interactions
There are 32 disease interactions with Etrafon Forte (amitriptyline / perphenazine).
- Dementia
- Brain damage
- Liver damage
- Acute alcohol intoxication
- CNS depression
- Hematologic toxicity
- Hypotension
- Liver disease
- Anticholinergic effects
- Cardiovascular disease
- Pheochromocytoma
- Acute myocardial infarction recovery
- Cardiovascular disease
- Seizure disorders
- Breast cancer
- NMS
- Renal dysfunction
- Seizure disorders
- Bone marrow suppression
- Diabetes
- Renal/liver disease
- Schizophrenia/bipolar disorder
- Tardive dyskinesia
- Acute alcohol intoxication
- Bipolar disorder screening
- Glaucoma
- Hyper/hypoglycemia
- Liver/renal disease
- Neutropenia
- Schizophrenia
- Thyroid disorders
- Urinary retention
Atypical antipsychotic agents (applies to Etrafon Forte) dementia
Major Potential Hazard, High plausibility.
Antipsychotic drugs are not approved for the treatment of patients with dementia-related psychosis. Older patients with dementia-related psychosis treated with antipsychotic drugs are at an increased risk of death; although the causes were varied, most of the deaths appeared to be either cardiovascular (e.g., heart failure, sudden death) or infectious (e.g., pneumonia) in nature. A causal relationship with antipsychotic use has not been established. In controlled trials in older patients with dementia-related psychosis, patients randomized to risperidone, aripiprazole, and olanzapine had higher incidence of cerebrovascular adverse events (e.g., stroke, transient ischemic attack), including fatalities, compared to patients treated with placebo.
Perphenazine (applies to Etrafon Forte) brain damage
Major Potential Hazard, High plausibility. Applicable conditions: Head Injury, History - Cerebrovascular Disease
Perphenazine is contraindicated in patients with suspected or established subcortical brain damage, with or without hypothalamic involvement. Perphenazine can interfere with thermoregulatory mechanisms, and a hyperthermic reaction with temperatures in excess of 40C (104F) may occur in such patients, sometimes not until 14 to 16 hours after drug administration.
Perphenazine (applies to Etrafon Forte) liver damage
Major Potential Hazard, High plausibility. Applicable conditions: Liver Disease
The manufacturer considers the use of perphenazine to be contraindicated in patients with preexisting liver damage. Phenothiazines are extensively metabolized by the liver and may accumulate in patients with hepatic impairment.
Phenothiazines (applies to Etrafon Forte) acute alcohol intoxication
Major Potential Hazard, High plausibility. Applicable conditions: Alcoholism
Phenothiazines are contraindicated in the presence of large amounts of central nervous system depressants such as alcohol. The risk of suicide and the danger of overdose may be increased in patients who use alcohol excessively. Phenothiazines should be used with caution in patients experiencing alcohol withdrawal.
Phenothiazines (applies to Etrafon Forte) CNS depression
Major Potential Hazard, High plausibility. Applicable conditions: Altered Consciousness, Respiratory Arrest
The use of phenothiazines is contraindicated in comatose patients and patients with severe central nervous system depression. Phenothiazines may potentiate the CNS and respiratory depression in these patients.
Phenothiazines (applies to Etrafon Forte) hematologic toxicity
Major Potential Hazard, Moderate plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
Phenothiazines may cause hematologic toxicity. In patients with preexisting blood dyscrasias, bone marrow suppression, or a history of drug-induced leukopenia or neutropenia, phenothiazines should not be used or are contraindicated. Complete blood counts should be regularly monitored in patients with risk factors for blood dyscrasias. If white blood cell counts indicate cellular depression, discontinue treatment and institute appropriate therapy.
Phenothiazines (applies to Etrafon Forte) hypotension
Major Potential Hazard, Moderate plausibility. Applicable conditions: Cardiovascular Disease, Cerebrovascular Insufficiency, History - Cerebrovascular Disease, History - Myocardial Infarction, Pheochromocytoma, Arrhythmias, Valvular Heart Disease, Hypertension
Phenothiazines may cause hypotension. Patients with pheochromocytoma, cerebral vascular or renal insufficiency, cardiovascular disease, or a severe cardiac reserve deficiency (e.g., mitral insufficiency) may be more prone to hypotensive reactions. Close monitoring is recommended during treatment if used in at-risk patients; some products may be contraindicated (e.g., thioridazine). Large doses and parenteral administration should be used cautiously, or avoided, in patients with impaired cardiovascular systems.
Phenothiazines (applies to Etrafon Forte) liver disease
Major Potential Hazard, Moderate plausibility.
Therapy with phenothiazines should be administered cautiously or are contraindicated in patients with preexisting liver disease or with a history of jaundice due to phenothiazine hypersensitivity. Patients with a history of hepatic encephalopathy due to cirrhosis may have increased sensitivity to the central nervous system effects of some phenothiazines (e.g., chlorpromazine). Treatment should be discontinued if jaundice occurs.
TCAs (applies to Etrafon Forte) anticholinergic effects
Major Potential Hazard, High plausibility. Applicable conditions: Glaucoma/Intraocular Hypertension, Urinary Retention, Gastrointestinal Obstruction
Tricyclic and tetracyclic antidepressants (TCAs) have anticholinergic activity, to which elderly patients are particularly sensitive. Tertiary amines such as amitriptyline and trimipramine tend to exhibit greater anticholinergic effects than other agents in the class. Therapy with TCAs should be administered cautiously in patients with preexisting conditions that are likely to be exacerbated by anticholinergic activity, such as urinary retention or obstruction; angle-closure glaucoma, untreated intraocular hypertension, or uncontrolled primary open-angle glaucoma; and gastrointestinal obstructive disorders. In patients with angle-closure glaucoma, even average doses can precipitate an attack. Glaucoma should be treated and under control prior to initiation of therapy with TCAs, and intraocular pressure monitored during therapy.
TCAs (applies to Etrafon Forte) cardiovascular disease
Major Potential Hazard, High plausibility. Applicable conditions: Hyperthyroidism, Cerebrovascular Insufficiency, History - Cerebrovascular Disease, History - Myocardial Infarction, Hypotension, Dehydration, Arrhythmias
Tricyclic and tetracyclic antidepressants (TCAs) may cause orthostatic hypotension, reflex tachycardia, syncope, and dizziness, particularly during initiation of therapy or rapid escalation of dosage. Imipramine appears to have the greatest propensity to induce these effects, while secondary amines such as nortriptyline may do so less frequently. Tolerance to the hypotensive effects often develops after a few doses to a few weeks. Rarely, collapse and sudden death have occurred secondary to severe hypotension. Other reported adverse cardiovascular effects include tachycardia, arrhythmias, heart block, hypertension, thrombosis, thrombophlebitis, myocardial infarction, strokes, congestive heart failure, and ECG abnormalities such as PR and QT interval prolongation. Therapy with TCAs should be avoided during the acute recovery phase following myocardial infarction, and should be administered only with extreme caution in patients with hyperthyroidism, a history of cardiovascular or cerebrovascular disease, or a predisposition to hypotension. Close monitoring of cardiovascular status, including ECG changes, is recommended at all dosages. Many of the newer antidepressants, including bupropion and the selective serotonin reuptake inhibitors (SSRIs), are considerably less or minimally cardiotoxic and may be appropriate alternatives.
TCAs (applies to Etrafon Forte) pheochromocytoma
Major Potential Hazard, Moderate plausibility.
Tricyclic and tetracyclic antidepressants (TCAs) may potentiate the effects of circulating catecholamines. Enhanced sympathetic activity can provoke hypertensive crises in patients with pheochromocytoma or other tumors of the adrenal medulla, such as some neuroblastomas. Therapy with TCAs should be administered cautiously in patients with these tumors.
Tricyclic antidepressants (applies to Etrafon Forte) acute myocardial infarction recovery
Major Potential Hazard, Moderate plausibility.
The use of most tricyclic antidepressants is contraindicated in patients that are going through the acute recovery period after a myocardial infarction.
Tricyclic antidepressants (applies to Etrafon Forte) cardiovascular disease
Major Potential Hazard, Moderate plausibility.
Tricyclic antidepressants should be used with extreme caution in patients with evidence of cardiovascular disease because of the possibility of fluctuations in the blood pressure, arrhythmias, conduction defects, tachycardia, myocardial infarction and stroke. This also applies to patients who have family history of sudden death, cardiac dysrhythmias, or conduction disturbances. In some cases a gradual dose titration is recommended.
Tricyclic antidepressants (applies to Etrafon Forte) seizure disorders
Major Potential Hazard, Moderate plausibility. Applicable conditions: Alcoholism, CNS Disorder
Tricyclic antidepressants (TCAs), can lower the seizure threshold and trigger seizures. These drugs should be used with extreme caution in patients with a history of seizures, or other predisposing factors, such as head trauma, CNS abnormalities, and alcoholism. Daily dose restrictions might apply for specific antidepressants. Physicians are encouraged to get additional dosing recommendations on the manufacturer's prescribing information.
Phenothiazines (applies to Etrafon Forte) breast cancer
Moderate Potential Hazard, Moderate plausibility.
The chronic use of phenothiazines is associated with persistent elevations in prolactin levels. The clinical significance in patients with a history of breast cancer is unknown and should be considered prior to therapy; approximately one-third of human breast cancers are thought to be prolactin-dependent. Chronic administration of neuroleptic drugs has been associated with mammary tumorigenesis in animal studies; however, evidence is inconclusive in humans.
Phenothiazines (applies to Etrafon Forte) NMS
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Neuroleptic Malignant Syndrome
Therapy with phenothiazines may precipitate or aggravate a potentially fatal symptom complex known as neuroleptic malignant syndrome (NMS). Treatment should not be initiated in patients with active NMS, and should be immediately discontinued if currently administered in such patients. In patients with a history of NMS, introduction or reintroduction of phenothiazines should be carefully considered, since NMS may recur.
Phenothiazines (applies to Etrafon Forte) renal dysfunction
Moderate Potential Hazard, Moderate plausibility.
Phenothiazines should be used with caution in patients with renal dysfunction. Patients with renal insufficiency may be more prone to hypotension. Periodic renal function tests are recommended for all patients during prolonged therapy.
Phenothiazines (applies to Etrafon Forte) seizure disorders
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: CNS Disorder, Seizures
Phenothiazines can lower the seizure threshold. Caution is recommended during administration in patients with a history of convulsive disorders or EEG abnormalities. Anticonvulsant therapy should be maintained or adequately adjusted during phenothiazine treatment.
TCAs (applies to Etrafon Forte) bone marrow suppression
Moderate Potential Hazard, Low plausibility. Applicable conditions: Bone Marrow Depression/Low Blood Counts
The use of tricyclic and tetracyclic antidepressants (TCAs) has rarely been associated with bone marrow suppression. Leukopenia, agranulocytosis, thrombocytopenia, anemia, eosinophilia, purpura, and pancytopenia have been reported with some TCAs. Patients with preexisting bone marrow suppression or blood dyscrasias receiving TCAs should be monitored closely during therapy for further decreases in blood counts.
TCAs (applies to Etrafon Forte) diabetes
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
Both elevation and lowering of blood sugar levels have been reported with the use of some tricyclic antidepressants (TCAs). Rarely, these effects have also occurred with maprotiline, a tetracyclic antidepressant. Patients with diabetes should be monitored for worsening control of blood glucose when treated with these agents, particularly during dosage escalation or whenever dosage has been altered.
TCAs (applies to Etrafon Forte) renal/liver disease
Moderate Potential Hazard, High plausibility. Applicable conditions: Renal Dysfunction
Tricyclic and tetracyclic antidepressants (TCAs) are known to undergo metabolism in the liver. Some of the metabolites, such as those of imipramine, clomipramine and desipramine, may be pharmacologically active. Many of the metabolites are also excreted by the kidney. There are very limited data concerning the use of TCAs in patients with renal and/or liver disease. Therapy with TCAs should be administered cautiously in patients with significantly impaired renal or hepatic function. Dosage adjustments may be necessary.
TCAs (applies to Etrafon Forte) schizophrenia/bipolar disorder
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Mania
Tricyclic antidepressants (TCAs) may aggravate symptoms of psychosis in schizophrenic patients, particularly those with paranoid symptomatology. Depressed patients, usually those with bipolar disorder, may experience a switch from depression to mania or hypomania. These occurrences have also been reported rarely with the tetracyclic antidepressant, maprotiline. Therapy with these agents should be administered cautiously in patients with schizophrenia, bipolar disorder, or a history of mania.
TCAs (applies to Etrafon Forte) tardive dyskinesia
Moderate Potential Hazard, Moderate plausibility.
Tricyclic and tetracyclic antidepressants (TCAs) have anticholinergic activity, to which elderly patients are particularly sensitive. Tertiary amines such as amitriptyline and trimipramine tend to exhibit greater anticholinergic effects than other agents in the class. As with other drugs that possess anticholinergic activity, TCAs may aggravate tardive dyskinesia or induce previously suppressed symptoms. Patients with tardive dyskinesia requiring therapy with TCAs should be monitored for exacerbation of the condition.
Tricyclic antidepressants (applies to Etrafon Forte) acute alcohol intoxication
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Alcoholism
Tricyclic antidepressants can enhance the response to alcohol. In patients who may use alcohol excessively, it should be borne in mind that the potentiation may increase the danger inherent in any suicide attempt or overdosage.
Tricyclic antidepressants (applies to Etrafon Forte) bipolar disorder screening
Moderate Potential Hazard, Moderate plausibility.
A major depressive episode can be the initial presentation of bipolar disorder. Patients with depressive symptoms should be adequately screened to determine if they are at risk for bipolar disorder prior to initiating treatment with a tricyclic antidepressant. This screening should include a detailed psychiatric history, including a family history of suicide, bipolar disorder, and depression. It should be noted that tricyclic antidepressants are not approved for use in treating bipolar depression.
Tricyclic antidepressants (applies to Etrafon Forte) glaucoma
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Glaucoma (Narrow Angle)
Tricyclic antidepressants as other type of antidepressants have an effect on pupil size causing dilation. This effect can potentially narrow the eye angle resulting in increased intraocular pressure and angle closure glaucoma, especially in predisposed patients. These drugs should be used with caution in patients with anatomically narrow angle or history of glaucoma. Doxepin hydrochloride capsules are contraindicated in patients with glaucoma.
Tricyclic antidepressants (applies to Etrafon Forte) hyper/hypoglycemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
There have been reports of both elevation and lowering of blood sugar levels in patients receiving tricyclic antidepressants. These drugs should be used with caution in patients with hypoglycemia, hyperglycemia or diabetes. Monitoring sugar levels is recommended.
Tricyclic antidepressants (applies to Etrafon Forte) liver/renal disease
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction, Liver Disease
In general, tricyclic antidepressants should be used with caution in patients with liver or renal disease, as these drugs are metabolized and excreted through the liver and kidneys. Dose selection, especially in the elderly patients that might have liver or renal dysfunction, should usually be limited to the smallest effective total daily dose. Some tricyclic antidepressants such as clomipramine and nortriptyline have occasionally been associated with elevations in SGOT (AST) and SGPT (ALT), and other hepatic adverse events such as jaundice. Although serious liver injury has only been reported rarely, therapy with these drugs should be administered cautiously in patients with preexisting liver disease and periodic monitoring of liver enzyme levels is recommended.
Tricyclic antidepressants (applies to Etrafon Forte) neutropenia
Moderate Potential Hazard, Moderate plausibility.
The use of some tricyclic antidepressants has been associated with neutropenia (ANC < 500/mm3) and agranulocytosis (ANC < 500/mm3). Leukocyte and differential blood counts should be performed in patients that develop fever and sore throat during treatment. Therapy should be discontinued if there is evidence of pathologic neutrophil depression.
Tricyclic antidepressants (applies to Etrafon Forte) schizophrenia
Moderate Potential Hazard, Moderate plausibility.
Some tricyclic antidepressants have shown to cause activation or exacerbation of psychosis in schizophrenic patients. A dosage reduction might be required.
Tricyclic antidepressants (applies to Etrafon Forte) thyroid disorders
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperthyroidism
Most tricyclic antidepressants should be administered with caution in hyperthyroid patients or those receiving thyroid medication as they may develop arrhythmias when these drugs are given.
Tricyclic antidepressants (applies to Etrafon Forte) urinary retention
Moderate Potential Hazard, Moderate plausibility.
Due to their anticholinergic properties, tricyclic antidepressants should be administered with caution in patients with history of urinary retention. Particularly doxepin hydrochloride capsules are contraindicated in patients with tendency to urinary retention.
Switch to professional interaction data
Etrafon Forte drug interactions
There are 817 drug interactions with Etrafon Forte (amitriptyline / perphenazine).
Etrafon Forte alcohol/food interactions
There are 3 alcohol/food interactions with Etrafon Forte (amitriptyline / perphenazine).
More about Etrafon Forte (amitriptyline / perphenazine)
- Check interactions
- Compare alternatives
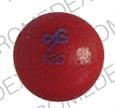
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: psychotherapeutic combinations
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.