Amiodarone Disease Interactions
There are 10 disease interactions with amiodarone.
- Dialysis
- Pulmonary dysfunction
- Sinus node dysfunction
- Visual impairment
- Cardiovascular dysfunction
- QT prolongation
- Hepatic impairment
- Neurologic dysfunction
- Thyroid dysfunction
- Electrolyte imbalance
Amiodarone (applies to amiodarone) dialysis
Major Potential Hazard, High plausibility. Applicable conditions: hemodialysis
Amiodarone and its active metabolite are not removed by hemodialysis.
Amiodarone (applies to amiodarone) pulmonary dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Pulmonary Impairment
Pulmonary toxicities such as hypersensitivity pneumonitis or interstitial/alveolar pneumonitis are potentially fatal (approximately 10% of the time) and have occurred in as many as 10% to 17% of patients administered daily dosages of approximately 400 mg of amiodarone. More frequently, asymptomatic abnormal diffusion capacity has been observed. Patients with preexisting pulmonary dysfunction does not appear to have an increased risk of pulmonary toxicity; however, they have a poorer prognosis if toxicity does develop. Thus, the risks and benefits of amiodarone therapy should be weighed carefully. Clinical monitoring of pulmonary function, including chest X-ray (baseline and every 3 to 6 months) and pulmonary function tests (with diffusion capacity), is recommended in all patients receiving amiodarone therapy. Any new respiratory symptom during treatment should be evaluated promptly and thoroughly, since toxicity is more likely to be reversible if diagnosed and managed early. Patients who develop hypersensitivity pneumonitis should be withdrawn permanently from amiodarone therapy and treated with steroids. In the case of interstitial/alveolar pneumonitis, steroid therapy and dosage reduction or discontinuation of amiodarone, if possible, usually result in clinical improvement. Subsequent rechallenge with amiodarone at reduced dosages does not always lead to return of toxicity and may be considered in some patients. The use of a lower loading dose and maintenance doses may also decrease the incidence of amiodarone- induced pulmonary toxicity.
Amiodarone (applies to amiodarone) sinus node dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block, Cardiogenic Shock
The use of amiodarone is contraindicated for use in patients with cardiogenic shock, severe sinus node dysfunction causing marked sinus bradycardia, second- or third-degree AV block, or symptomatic bradycardia in the absence of a functioning pacemaker.
Amiodarone (applies to amiodarone) visual impairment
Major Potential Hazard, Low plausibility. Applicable conditions: Visual Defect/Disturbance
Optic neuropathy and/or neuritis has occurred during administration of amiodarone and has resulted in visual impairment such as changes in visual acuity, decrease in peripheral vision, and blindness. Optic toxicity can occur at any time following initiation of amiodarone. Therapy with amiodarone should be administered cautiously in patients with visual defects. Regular ophthalmologic examinations including fundoscopy and slit- lamp examinations are recommended.
Antiarrhythmics (applies to amiodarone) cardiovascular dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Congestive Heart Failure, Hypotension
Antiarrhythmic agents can induce severe hypotension (particularly with IV administration) or induce or worsen congestive heart failure (CHF). Patients with primary cardiomyopathy or inadequately compensated CHF are at increased risk. Antiarrhythmic agents should be administered cautiously and dosage and/or frequency of administration modified in patients with hypotension or adequately compensated CHF. Alternative therapy should be considered unless these conditions are secondary to cardiac arrhythmia.
Antimalarial agents (applies to amiodarone) QT prolongation
Major Potential Hazard, Moderate plausibility. Applicable conditions: Psoriasis
The use of certain antimalarial agents is contraindicated in patients with known prolongation of QT interval as these patients can develop fatal arrhythmias. These drugs should also be avoided in patients with clinical conditions known to prolong the QT interval, such as uncorrected hypokalemia or hypomagnesemia, bradycardia, and certain other cardiac conditions. Caution is advised in patients taking other medications that can prolong the QT interval.
Amiodarone (applies to amiodarone) hepatic impairment
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
There have been rare reports of fatal hepatocellular necrosis after treatment with amiodarone. In patients with life-threatening arrhythmias, the potential risk of hepatic injury should be weighed against the potential benefit of amiodarone therapy. Patients with hepatic impairment should be monitored for evidence of progressive hepatic injury. Consideration should be given to reducing the rate of administration or withdrawing treatment if needed.
Amiodarone (applies to amiodarone) neurologic dysfunction
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Neurologic Disorder, Parkinsonism
Reversible and dose-related nervous system toxicity such as dizziness, paresthesia, tremor and involuntary movements, lack of coordination, abnormal gait and ataxia is commonly noted in patients receiving amiodarone. Therapy with amiodarone should be administered cautiously and dosage modifications considered in patients with or predisposed to neurologic dysfunction.
Amiodarone (applies to amiodarone) thyroid dysfunction
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Hyperthyroidism, Hypothyroidism
Amiodarone inhibits peripheral conversion of thyroxine (T4) to triiodothyronine (T3) and also contributes inorganic iodine that can result in altered thyroid function tests, hypothyroidism, or hyperthyroidism. Therapy with amiodarone should be administered cautiously in patients with thyroid dysfunction. Clinical monitoring, including baseline and periodic evaluation of thyroid function is recommended. Modification of thyroid therapy may be necessary.
Antiarrhythmics (applies to amiodarone) electrolyte imbalance
Moderate Potential Hazard, High plausibility. Applicable conditions: Hypokalemia, Hyperkalemia, Magnesium Imbalance
Electrolyte imbalance can alter the therapeutic effectiveness of antiarrhythmic agents. Hypokalemia and hypomagnesemia can reduce the effectiveness of antiarrhythmic agents. In some cases, these disorders can exaggerate the degree of QTc prolongation and increase the potential for torsade de pointes. Hyperkalemia can potentiate the toxic effects of antiarrhythmic agents. Electrolyte imbalance should be corrected prior to initiating antiarrhythmic therapy. Clinical monitoring of cardiac function and electrolyte concentrations is recommended.
Switch to professional interaction data
Amiodarone drug interactions
There are 755 drug interactions with amiodarone.
Amiodarone alcohol/food interactions
There is 1 alcohol/food interaction with amiodarone.
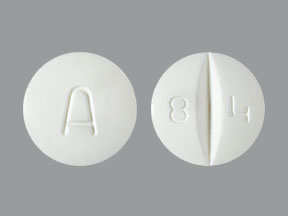
More about amiodarone
- amiodarone consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (96)
- Drug images
- Side effects
- Dosage information
- Patient tips
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.