Vaginal Hysterectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about a vaginal hysterectomy:
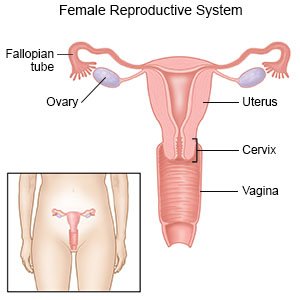
A vaginal hysterectomy is surgery to remove your uterus through your vagina. Other organs, such as your ovaries and fallopian tubes, may also be removed.
 |
How to prepare for a vaginal hysterectomy:
Your healthcare provider will talk to you about how to prepare for surgery. He or she may tell you not to eat or drink anything after midnight on the day of your surgery. You will need to stop taking aspirin 7 to 10 days before your procedure. You will need to stop taking NSAIDs 3 days before your procedure. You will also need to stop taking certain herbal supplements 7 days before your procedure. These include garlic, gingko biloba, and ginseng. Your provider may tell you to shower the night before your surgery. He or she may tell you to use a certain soap to help prevent a surgical site infection. Your provider will tell you what medicines to take or not take on the day of your surgery. You will be given an antibiotic through your IV to help prevent a bacterial infection. Arrange for someone to drive you home and stay with you after surgery.
What will happen during a vaginal hysterectomy:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given regional anesthesia to numb the lower part of your body. Your surgeon will make an incision in the area where your vagina and cervix (the opening to your uterus) meet. He or she will tie the blood vessels that go to your uterus to help decrease bleeding. He or she will then cut and tie the ligaments that hold your uterus in place.
- Your surgeon will remove your uterus through your vagina. He or she may also remove your cervix, ovaries, and fallopian tubes. Your surgeon may also remove tissue surrounding your uterus. Any incisions that were made will be closed with absorbable stitches. A vaginal pack or sanitary pad may be used to absorb bleeding. A vaginal pack is a special gauze that is inserted into the vagina.
What will happen after a vaginal hysterectomy:
You may have a catheter to help drain your bladder for up to 24 hours. You will have pain for the first few days after surgery. You will need to wear sanitary pads for vaginal bleeding that occurs after surgery. You will be asked to walk as soon as possible after surgery. This will help to prevent blood clots in your legs. You may need to stay in the hospital after surgery.
Risks of a vaginal hysterectomy:
- The surgeon may need to change the type of surgery he or she was planning to do. For example, he or she may need to change to an open abdominal surgery. You will not be able to become pregnant after you have a hysterectomy. You will go through menopause if your ovaries are removed.
- You may bleed more than expected or get an infection. Your bladder, ureters, or bowels may be damaged during surgery. If your ureters were injured, you may need a catheter to drain your bladder for several days to weeks. You may get scar tissue in your abdomen that blocks your intestine or causes pelvic pain. If you have a hysterectomy to treat cancer, this surgery may not take it away completely. There is also a chance that the cancer may return. You may get a blood clot in your leg or arm. This may become life-threatening.
Call your local emergency number (911 in the US) for any of the following:
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Related medications
Contact your healthcare provider or gynecologist if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have increasing abdominal or pelvic pain.
- You have heavy vaginal bleeding that fills 1 or more sanitary pads in 1 hour.
- You have a fever.
- You have nausea or are vomiting.
- You feel pain or burning when you urinate, or you have trouble urinating.
- You have pus or a foul-smelling odor coming from your vagina.
- You feel pressure in your rectum.
- You have questions or concerns about your condition or care.
Medicines:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Stool softeners help treat or prevent constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Activity:
- Wear an abdominal binder as directed. An abdominal binder will decrease pain when you move or cough.
- Rest as needed. Get up and move around as directed to help prevent blood clots. Start with short walks and slowly increase the distance every day. Limit the number of times you climb stairs to 2 times each day. Plan most of your daily activities on one level of your home.
- Do not lift objects heavier than 10 pounds for 6 weeks. Avoid strenuous activity for 2 weeks.
- Do not strain during bowel movements. High-fiber foods and extra liquids can help you prevent constipation. Examples of high-fiber foods are fruit and bran. Prune juice and water are good liquids to drink.
- Do not have sex, use tampons, or douche for up to 8 weeks. Ask your healthcare provider if it is okay to take a tub bath.
- Do not go in pools or hot tubs for 6 weeks or as directed.
- Ask when it is safe for you to drive, return to work, and return to other regular activities.
Deep breathing:
Take deep breaths and cough 10 times each hour. This will decrease your risk for a lung infection. Take a deep breath and hold it for as long as you can. Let the air out and then cough strongly. Deep breaths help open your airway. You may be given an incentive spirometer to help you take deep breaths. Put the plastic piece in your mouth and take a slow, deep breath, then let the air out and cough. Repeat these steps 10 times every hour.
Get support:
This surgery may be life-changing for you and your family. You will no longer be able to get pregnant. Sudden changes in the levels of your hormones may occur and cause mood swings and depression. You may feel angry, sad, or frightened, or cry frequently and unexpectedly. These feelings are normal. Talk to your healthcare provider about where you can get support. You can also ask if hormone replacement medicine is right for you.
Follow up with your healthcare provider or gynecologist as directed:
You may need to return for other tests. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
