Uterine Prolapse
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
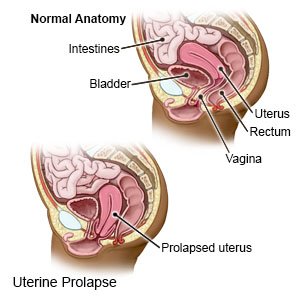
A uterine prolapse
is a condition that causes your uterus to slip down into your vagina. Prolapse can happen if the tissues and muscles supporting your uterus become weak or damaged.
 |
Common signs and symptoms:
- Pelvic pressure or heaviness
- A soft bulge or lump in your vagina that may bulge through your vaginal opening
- Trouble urinating or having a bowel movement
- Pain in your lower back, pelvis, or vagina
- Pain during sex
Seek care immediately if:
- You have bleeding from your vagina that does not stop.
- You have a mass coming out of your vagina that you cannot push back in.
- You are unable to urinate or have a bowel movement.
- You have severe abdominal pain.
Related medications
Call your doctor or gynecologist if:
- You are leaking urine or bowel movement.
- You have a fever.
- You have foul-smelling fluid coming from your vagina.
- You see blood coming from your vagina that is not from your monthly period.
- You have questions or concerns about your condition or care.
Treatment:
The goal of treatment is to correct the prolapse and relieve your signs and symptoms. Treatment may include any of the following:
- Estrogen may help strengthen the pelvic muscles and keep the prolapse from getting worse. This may be taken as a pill, applied as a cream, or inserted into your vagina.
- A vaginal device, such as a pessary or sphere, may be used to hold your uterus in place and support your muscles. These devices may help decrease pressure on other pelvic organs, or help you do Kegel exercises. If your gynecologist fits you for a pessary, you will need to remove and clean it regularly. You will be taught when and how to clean the pessary.
- Surgery may be needed to fix the prolapse. You may have surgery to tighten the muscles and tissues that hold your uterus in place. Your healthcare provider may use a mesh patch or a tissue graft to support or hold your uterus in place. Hysterectomy is surgery used to remove your uterus. Surgery to close your vagina may be used to hold your uterus in place.
Manage your symptoms:
- Sit with your legs elevated. This can help relieve pain or discomfort. Put pillows or blankets under your ankles to elevate your entire legs.
- Do Kegel exercises. These exercises strengthen the muscles that hold your uterus in place. They also tighten the muscles you use when you urinate or have a bowel movement. Tighten muscles in your pelvis (muscles you use to stop urinating). Hold the muscles tight for 5 seconds, then relax for 5 seconds. Gradually work up to holding the muscles contracted for 10 seconds. Do at least 3 sets of 10 repetitions a day.
- Do not strain. Do not lift heavy objects, stand for long periods of time, or strain to have a bowel movement. Prevent constipation by drinking plenty of liquids and eating foods high in fiber. Ask how much liquid to drink every day. High-fiber foods include fresh fruits, vegetables, and whole grains.
- Maintain a healthy weight. Ask your healthcare provider for a healthy weight for you. Ask him or her to help you create a weight loss plan if you are overweight. He or she can also help you create an exercise program. Exercise helps your bowels work better and decreases pressure inside your colon.
Follow up with your doctor or gynecologist as directed:
You may need to return regularly to have your pessary checked. You may also need to see your gynecologist for possible surgery. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
