Support for your Loved One after a Stroke
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about support for your loved one after a stroke:
A stroke can make physical tasks more challenging for your loved one. He or she may need help with personal care and daily activities. He or she may also have depression or other emotional changes. You can offer support to help your loved one with physical, mental, and emotional activities.
Call your local emergency number (911 in the US) if your loved one has any of the following:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
- Trouble waking, or you cannot wake him or her
- A fall that includes hitting his or her head
- A seizure
- Chest pain with or without shortness of breath
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have loss of balance or coordination.
- You have double vision or vision loss.
- You have unusual or heavy bleeding.
Call your loved one's doctor or neurologist if he or she has any of the following:
- Weak, dizzy, or fainting spells
- A fall without hitting his or her head
- Blood sugar or blood pressure levels that are higher or lower than healthcare providers recommend
- Feelings of extreme sadness or anxiety
- Trouble sleeping
- Choking or coughing fits when eating or drinking
- New or worsening symptoms
- You have questions or concerns about your loved one's condition or care.
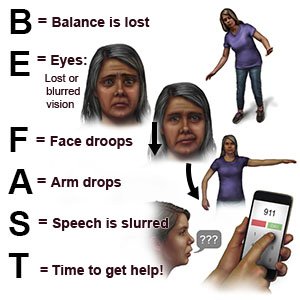
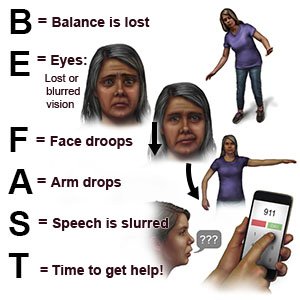
Know the warning signs of a stroke:
The words BE FAST can help you remember and recognize warning signs of a stroke:
- B = Balance: Sudden loss of balance
- E = Eyes: Loss of vision in one or both eyes
- F = Face: Face droops on one side
- A = Arms: Arm drops when both arms are raised
- S = Speech: Speech is slurred or sounds different
- T = Time: Time to get help immediately
 |
Be part of therapy:
- Go with your loved one to therapy. Learn exercises and ways to help him or her manage the physical effects of the stroke.
- Help practice the skills learned in therapy. More practice may improve recovery from a stroke.
- Help with range of motion (ROM) exercises. ROM exercises are gentle, slow movements of joints. Physical therapists will show you and your loved one how to do ROM exercises. ROM exercises can help increase flexibility and decrease pain.
Understand your loved one's strengths and weaknesses:
A stroke can affect a person in many ways. Understand what he or she can do and what help may be needed. You can show support by doing the following:
- Encourage self-care tasks. Encourage him or her to do as many self-care tasks as possible. Help build on strengths. Do not point out what he or she used to be able to do. Some effects of a stroke may be permanent.
- Help your loved one exercise his or her mind. Board games, crossword puzzles, and mind exercises may help improve problem solving skills and memory.
- Give simple step-by-step directions. He or she may have difficulty paying attention or completing tasks.
- Be patient. Your loved one may think and act more slowly after a stroke. Let him or her know that you are there to give support.
Related medications
Understand the treatment plan:
Your loved one may need several therapies or medicines after a stroke. It is important for you to know the following:
- The goals of therapy
- Reasons for new medicines, when and how to give each medicine, and side effects to report
- Lifestyle changes such as healthy eating, getting more exercise, or quitting smoking
- Assistive devices needed and how they are used
- Care equipment that may be needed at home, such as handrails, a wheelchair, or a raised toilet seat
Understand your loved one's insurance plan:
Find out the services covered by his or her insurance plan. Understand the out-of-pocket costs. Talk to a social worker or case manager about services that are not covered.
Help lower your loved one's risk for another stroke:
- Prepare healthy foods. Healthy foods can decrease the risk for heart disease and other conditions that could cause another stroke. You may want to work with a dietitian to help plan healthy meals. A stroke can cause problems with swallowing. A dietitian can help you create meal plans with foods that are easier to swallow.

- Encourage your loved one to quit smoking, if needed. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Ask healthcare providers for information on quitting. E- cigarettes or smokeless tobacco still contain nicotine. Talk to providers before your loved one uses these products.
- Encourage your loved one to limit or stop drinking alcohol, if needed. Alcohol can raise your loved one's blood pressure. Alcohol can also raise his or her blood sugar level, or make diabetes more difficult to manage. A healthcare provider can tell your loved one how many drinks are okay to have within 24 hours and within 1 week. A drink is 12 ounces of beer, 5 ounces of wine, or 1½ ounces of alcohol.
- Exercise together. Exercise may lower blood pressure and prevent heart disease. Talk to healthcare providers about the best exercise program for your loved one. He or she may have balance or movement problems that can make some exercises less safe. It may help to find exercises you both enjoy and can do together safely.
- Help him or her take medicines as directed. Blood thinners and medicines to manage blood pressure or heart conditions can decrease the risk for another stroke. You may need to set an alarm or use other reminders if medicines need to be given at certain times each day.
Lower the risk for falls at home:
- Tape electrical cords down or remove them from hallways and walkways.
- Keep paths clear throughout the home.
- Make sure the home has good lighting.
- Put nonslip materials on surfaces that might be slippery. An example is the bathtub or shower floor. Remind your loved one to ask for help getting in and out of the shower.
- Encourage the use of assistive devices such as a cane or walker.
 |
Know the signs of depression after a stroke:
Depression can lower your loved one's quality of life. He or she may stop doing things that can help build strength. Depression can cause him or her to become more dependent. Tell your loved one's healthcare providers if you see any signs of depression:
- Extreme sadness
- Avoiding social interaction with family or friends
- A lack of interest in things he or she once enjoyed
- Irritability
- Trouble sleeping
- Low energy levels
- A change in eating habits or sudden weight gain or loss
Take care of yourself:
- Ask for help. Healthcare providers can help you find respite care if needed. This means medical care providers take care of your loved one so you can rest. You may be able to get help from home health aids or nurses. You may also be able to get help with transportation to appointments. Ask family or friends to stay with your loved one so you can have a break. Take time for yourself to relax and enjoy activities. Eat healthy foods, exercise, and get plenty of rest.
- Join a support group. It may be helpful to discuss your fears or concerns with others who care for someone who had a stroke. Other caregivers may understand how you feel. You may get ideas about how to give support and cope with stress. Healthcare providers can help you find a support group.
Follow up with your loved one's doctor or neurologist as directed:
Write down your questions so you remember to ask them during your visits.
For support and more information:
- American Stroke Association
Phone: 1- 888 - 478-7653
Web Address: http://www.stroke.org
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
