Rigid Sigmoidoscopy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
WHAT YOU NEED TO KNOW:
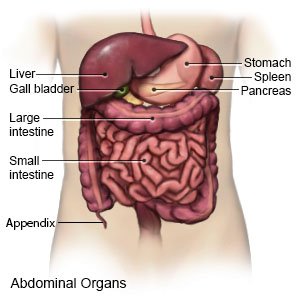
A rigid sigmoidoscopy is a procedure to look inside your rectum and sigmoid colon. The sigmoid colon is the lower part of your intestines, closest to your rectum. A sigmoidoscope will be inserted into your rectum. This is a firm tube with a light and tiny camera on the end. Pictures of your colon appear on a monitor during the procedure. A rigid sigmoidoscopy may help diagnose colon diseases, inflammation, polyps (growths), or infections.
 |
HOW TO PREPARE:
Before your procedure:
- Your healthcare provider will tell you how to prepare. Arrange to have someone drive you home after the procedure.
- Tell your provider if you have had a sigmoidoscopy, barium enema, or colonoscopy before and when it was done.
- Tell your provider about all medicines you currently take. You will be told if you need to stop any medicine for this procedure, and when to stop. Your provider will tell you which medicines to take or not take on the day of the procedure.
- You may need blood, urine, or bowel movement tests.
- Tell your provider if you are pregnant or have other medical conditions, such as severe bowel inflammation or kidney problems. Certain medicines used to empty your colon may not be good for you.
The night before your procedure:
You may be told not to eat or drink anything after midnight.
The day of your procedure:
- You or a close family member will be asked to sign a legal document called a consent form. It gives healthcare providers permission to do the procedure or surgery. It also explains the problems that may happen, and your choices. Make sure all your questions are answered before you sign this form.
- Your bowel needs to be empty before your procedure. This is so healthcare providers can see the inside of your colon more clearly. You may need a laxative. This is a pill that will help empty your bowel. You may also need an enema. This is a liquid inserted into your rectum to flush out your bowel.
- Take only the medicines your healthcare provider told you to take. If you need to take medicines, take them with few small sips of water.
- Healthcare providers may insert an IV into your vein. You may be given liquids or medicine through the IV.
- You may get medicine to help you relax for this procedure.
WHAT WILL HAPPEN:
What will happen:
- You will be asked to lie on your left side and raise one or both knees toward your chest. Your healthcare provider will examine your anus and use a finger to check your rectum. Your provider may feel for your prostate if you are a man. If your bowel is not empty, your healthcare provider may give you another enema.
- The sigmoidoscope will be lubricated and gently inserted into your rectum and sigmoid colon. Your provider will put water or air into the tube to help clean or expand your colon. The passage of the tube and air may cause a feeling of pressure and a little discomfort. Your healthcare provider may take tissue samples from the walls of the bowel and send them to the lab for tests. Your provider will also remove bowel movement that may be blocking your bowel.
After your procedure:
You may have gas or bloating because of air that is still in your colon. Medicines may be given to relieve pain or to make it easier to have a bowel movement. You may be allowed to go home when your healthcare provider sees you are okay.
CONTACT YOUR HEALTHCARE PROVIDER IF:
- You have a fever.
- You have questions or concerns about your procedure.
Seek Care Immediately if
- You have blood in your bowel movement.
- You are not able to have a bowel movement.
- Your abdomen becomes tender and hard.
- Your vomit has blood or bile (yellow or green fluid) in it.
Risks
You may bleed or have pain as the scope is inserted. Your heartbeat may slow and your blood pressure may go so low that you sweat and faint. The scope may puncture (make a hole) or perforate (tear) your colon. This may cause bowel movement to leak out of the colon and into your abdomen.
Related medications
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
