Left Hemispheric Stroke
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
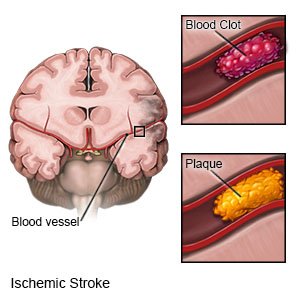
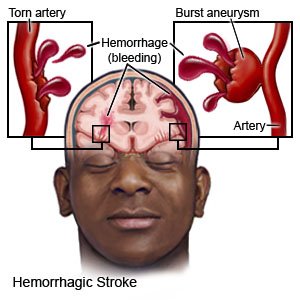
A left hemispheric stroke
happens when blood cannot flow to the left hemisphere (side) of your brain. A stroke caused by a blood clot is called an ischemic stroke. A stroke caused by a burst or torn blood vessel is called a hemorrhagic stroke. A stroke is a medical emergency that needs immediate treatment.
 |
 |
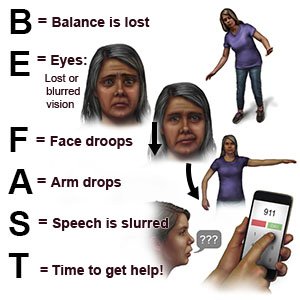
Warning signs of a stroke:
The words BE FAST can help you remember and recognize warning signs of a stroke:
- B = Balance: Sudden loss of balance
- E = Eyes: Loss of vision in one or both eyes
- F = Face: Face droops on one side
- A = Arms: Arm drops when both arms are raised
- S = Speech: Speech is slurred or sounds different
- T = Time: Time to get help immediately
 |
Signs and symptoms:
The left hemisphere of your brain controls the right side of your body. It also controls your speech and language abilities. You may have any of the following:
- Trouble swallowing, walking, or remembering
- Paralysis or weakness on the right side of your body
- Loss of vision in one or both eyes
- Falling toward your right side
- Lack of awareness of the right side of your body
- Trouble speaking, reading, writing, or understanding language
- Changes in mood or the ability to pay attention or learn new information
Call your local emergency number (911 in the US) or have someone else call if:
- You have any of the following signs of a stroke:
- Numbness or drooping on one side of your face
- Weakness in an arm or leg
- Confusion or difficulty speaking
- Dizziness, a severe headache, or vision loss
-
- You have a seizure.
- You feel lightheaded, short of breath, and have chest pain.
- You cough up blood.
Seek care immediately if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have loss of balance or coordination.
- You have double vision or vision loss.
- You have unusual or heavy bleeding.
- You have trouble swallowing.
Call your doctor or neurologist if:
- Your blood pressure or blood sugar level is higher or lower than you were told it should be.
- You have trouble having a bowel movement or urinating.
- You have questions or concerns about your condition or care.
Related medications
Treatment
depends on the type of stroke you had. You may need any of the following:
- Medicines may help improve your blood's ability to clot and stop the bleeding. You may instead need medicine to break up blood clots, or to prevent them from forming. You may also need medicine to treat pain, high blood pressure, high cholesterol, or diabetes.
- Thrombolysis is a procedure used to break apart clots in an artery. A catheter is guided into the artery until it is near the clot. Medicine is put through the catheter that will help break apart the clot. The clot may be pulled out of the artery during the procedure.
- Surgery may be used to remove a blood clot or to relieve pressure within your brain. You may also need surgery to remove plaque buildup from your carotid arteries. Surgery may instead be needed to stop the bleeding or remove blood that has leaked out of the blood vessels.
Recovery testing:
Your healthcare provider will test your recovery 90 days (3 months) after your stroke. This may be done over the phone or in person. Your provider will ask how well you can do the activities you did before the stroke. He or she will also ask how well you can do your daily activities without help. Your provider may make recommendations for you based on your test. For example, you may need someone to help you walk safely. You may also need help with daily activities, such as getting dressed. Based on your answers, your provider may do this test again over time.
Self-care:
- Go to stroke rehabilitation (rehab) as directed. Rehab is a program run by specialists who will help you recover abilities you may have lost. Specialists include physical, occupational, and speech therapists. Physical therapists help you gain strength or keep your balance. Occupational therapists teach you new ways to do daily activities. Your therapy may include movements for everyday activities. An example is being able to raise yourself from a chair. A speech therapist helps you improve your ability to talk and swallow.
- Make your home safe. Remove anything you might trip over. Tape electrical cords down. Keep paths clear throughout your home. Make sure your home is well lit. Put nonslip materials on surfaces that might be slippery. An example is your bathtub or shower floor. A cane or walker may help you keep your balance as you walk.

What you need to know about depression:
Talk to your healthcare provider if you have depression that continues or is getting worse. Your provider may be able to help treat your depression. Your provider can also recommend support groups for you to join. A support group is a place to talk with others who have had a stroke. It may also help to talk to friends and family members about how you are feeling. Tell your family and friends to let your healthcare provider know if they see any signs of depression:
- Extreme sadness
- Avoiding social interaction with family or friends
- A lack of interest in things you used to enjoy
- Irritability
- Trouble sleeping
- Low energy levels
- A change in eating habits or sudden weight gain or loss
Lower your risk for another stroke:
- Manage health conditions. A condition such as diabetes can increase your risk for a stroke. Control your blood sugar level if you have hyperglycemia or diabetes. Take your prescribed medicines and check your blood sugar level as directed.

- Check your blood pressure if directed. High blood pressure can increase your risk for a stroke. Follow your healthcare provider's directions for controlling your blood pressure.

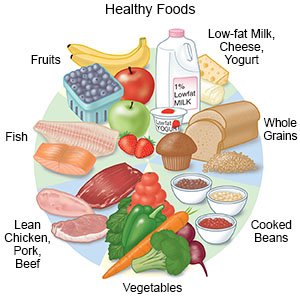
- Eat a variety of healthy foods. Healthy foods include whole-grain breads, low-fat dairy products, beans, lean meats, and fish. Eat at least 5 servings of fruits and vegetables each day. Choose foods that are low in fat, cholesterol, salt, and sugar. Eat foods that are high in potassium, such as potatoes and bananas. A dietitian can help you create healthy meal plans.
- Maintain a healthy weight. Ask your healthcare provider what a healthy weight is for you. Ask him or her to help you create a weight loss plan, if needed. He or she can help you create small goals if you have a lot of weight to lose.
- Exercise as directed. Exercise can lower your blood pressure, cholesterol, weight, and blood sugar levels. Healthcare providers will help you create exercise goals. They can also help you make a plan to reach your goals. For example, you can break exercise into 10 minute periods, 3 times in the day. Find an exercise that you enjoy. This will make it easier for you to reach your exercise goals.
- Do not drink alcohol. Alcohol can increase your risk for a stroke. Alcohol may also increase your blood pressure or thin your blood. Blood thinning can increase your risk for hemorrhagic stroke.
- Do not use nicotine products or illegal drugs. Nicotine and other chemicals in cigarettes and cigars can cause blood vessel damage. Nicotine and illegal drugs both increase your risk for a stroke. Ask your healthcare provider for information if you currently smoke or use drugs and need help to quit. E- cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
Follow up with your doctor or neurologist as directed:
You may need to come in for regular tests of your brain function. You may also need regular blood tests. Write down your questions so you remember to ask them during your visits.
For support and more information:
- American Stroke Association
Phone: 1- 888 - 478-7653
Web Address: http://www.stroke.org
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
