Heart Attack
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
A heart attack happens when the blood vessels that supply blood to your heart are blocked. This can damage your heart or lead to an abnormal heart rhythm or heart failure. A heart attack is also called a myocardial infarction.
 |
DISCHARGE INSTRUCTIONS:
Call your local emergency number (911 in the US) for any of the following:
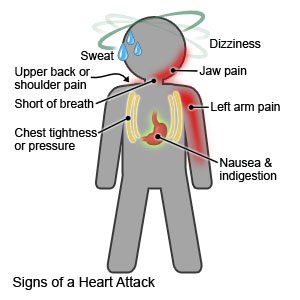
- You have any of the following signs of a heart attack:
- Squeezing, pressure, or pain in your chest
- You may also have any of the following:
- Discomfort or pain in your back, neck, jaw, stomach, or arm
- Shortness of breath
- Nausea or vomiting
- Lightheadedness or a sudden cold sweat
Seek care immediately if:
- You are tired and cannot think clearly.
- Your heart is beating faster than usual.
- You are bleeding from your gums or nose.
- You see blood in your urine or bowel movements.
- You urinate less than usual or not at all.
- You have new or increased swelling in your feet or ankles.
Call your doctor or cardiologist if:
- You have trouble taking your heart medicine.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Heart medicines help decrease blood pressure, control your heart rate, and help your heart function better.
- Nitroglycerin opens the arteries to your heart, increases oxygen levels, and can decrease chest pain. You may get your nitroglycerin as a pill, a patch, or a paste. Ask your healthcare provider or cardiologist how to safely take this medicine.
- Aspirin helps prevent clots from forming and causing blood flow problems. If healthcare providers want you to take aspirin daily, do not take acetaminophen or ibuprofen instead. Do not take more or less aspirin than healthcare providers say to take. If you are on another blood thinner medicine, ask your healthcare provider or cardiologist before you take aspirin for any reason.
- Antiplatelets , such as aspirin, help prevent blood clots. Take your antiplatelet medicine exactly as directed. These medicines make it more likely for you to bleed or bruise. If you are told to take aspirin, do not take acetaminophen or ibuprofen instead.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Cholesterol medicine decreases cholesterol and the amount of plaque in your blood.
- Do not take certain medicines without asking your healthcare provider first. These include NSAIDs, herbal or vitamin supplements, or hormones (estrogen or progestin).
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Cardiac rehabilitation (rehab)
is a program run by specialists who will help you safely strengthen your heart and prevent more heart disease. The plan includes exercise, relaxation, stress management, and heart-healthy nutrition. Healthcare providers will also check to make sure any medicines you take are working. The plan may also include instructions for when you can drive, return to work, and do other normal daily activities.
Manage other health conditions:
Diabetes and high cholesterol increases your risk for another heart attack and stroke. Talk to your healthcare provider about your management plan. He or she will make a plan that helps you manage your conditions.
Check your blood pressure at home:
High blood pressure can increase your risk for another heart attack. Sit and rest for 5 minutes before you take your blood pressure. Extend your arm and support it on a flat surface. Your arm should be at the same level as your heart. Follow the directions that came with your monitor. If possible, take at least 2 readings each time. Take your blood pressure at least 2 times each day at the same times, such as mornings and evenings. Keep a record of your readings and bring it to your follow-up visits. Ask your healthcare provider what your blood pressure should be.
 |
Get a flu vaccine every year as soon as it is available:
The vaccine will help prevent the flu. A heart attack will make it harder for you to fight off the flu virus on your own. The flu may also be worse for you than for a person who has not had a heart attack. Ask about other vaccinations you may need.
Lifestyle changes you may need to make after a heart attack:
- Follow a heart-healthy diet. A heart-healthy diet is an eating plan low in total fat, unhealthy fats, and sodium (salt). A heart-healthy diet helps decrease your risk for heart disease and stroke. Limit the amount of fat you eat to 25% to 35% of your total daily calories. Your healthcare provider may recommend the DASH (Dietary Approaches to Stop Hypertension) Eating Plan to help lower high blood pressure and LDL (bad) cholesterol. The plan is low in sodium, sugar, unhealthy fats, and total fat. It is high in potassium, calcium, magnesium, and fiber. Ask for more information about this plan.

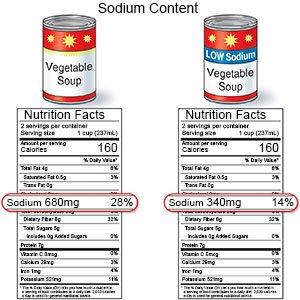
- Limit sodium (salt) as directed. Too much sodium can affect your fluid balance. Check labels to find low-sodium or no-salt-added foods. Some low-sodium foods use potassium salts for flavor. Too much potassium can also cause health problems. Your healthcare provider will tell you how much sodium and potassium are safe for you to have in a day. He or she may recommend that you limit sodium to 2,300 mg a day.
- Do not smoke. Nicotine and other chemicals in cigarettes and cigars can cause lung and heart damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Exercise as directed. Ask your healthcare provider about the best exercise plan for you. Exercise makes your heart stronger, lowers blood pressure, and helps prevent a heart attack. The goal is 30 to 60 minutes a day, 5 to 7 days a week. You may have to work up to this goal. Healthcare providers can help you reach this goal, starting in cardiac rehab sessions.
- Maintain a healthy weight. Ask your healthcare provider how much you should weigh. He or she can help you create a safe weight loss plan if you are overweight.
- Manage stress. Stress may increase your risk for another heart attack. Learn ways to control stress, such as relaxation, deep breathing, and music. Talk to someone about things that upset you.
Follow up with your healthcare provider or cardiologist within 14 days or as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Heart Attack
Treatment options
Care guides
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
