Dilation and Curettage
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
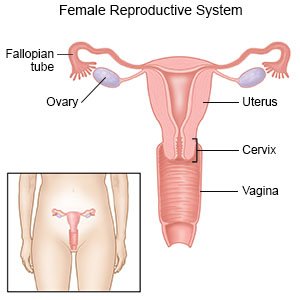
Dilation and curettage (D&C)
is a procedure to remove tissue from the lining of your uterus.
 |
How to prepare for a D&C:
- Your healthcare provider will talk to you about how to prepare for your D&C. He or she may tell you not to eat or drink anything after midnight on the day of your procedure. He or she will tell you which medicines to take or not take on the day of your procedure. You may need blood tests before and after your D&C. You may need immune globulin medicine if your blood is Rh-negative, and you had a miscarriage. This medicine helps prevent problems with a future pregnancy.
- You may need a vaginal swab test before your D&C to check for infection. Healthcare providers may place medicine in your cervix to help it dilate. This medicine may be inserted 1 to 2 days before your procedure or the day of your procedure. You may be given an antibiotic through your IV to help prevent a bacterial infection.
What will happen during a D&C:
- You may be given local or epidural anesthesia to numb your procedure area and decrease discomfort. With local or epidural anesthesia, you will be awake during your procedure. Medicine may be given in your IV to help you relax or make you drowsy. You may instead be given general anesthesia to keep you asleep during the procedure. You will lie on your back with your feet in stirrups. A tool called a speculum will be inserted into your vagina to keep it open. Your healthcare provider will check your cervix to see if it is dilated. If needed, he or she may use tools to dilate your cervix.
- Your healthcare provider may use a tool or suction to remove tissue from your uterus. To use suction, your healthcare provider will insert a thin tube into your uterus. The tube is connected to a suction machine or a syringe. The tissue will be removed through the tube. Forceps may be needed to remove larger amounts of tissue. Tissue may be sent to a lab for tests. Medicines may be given to help your uterus tighten, and prevent heavy bleeding.
What to expect after a D&C:
You will be taken to a recovery room so healthcare providers can watch for heavy bleeding or other problems. You may be able to go home a few hours after your D&C. Have someone drive you home. You may have cramps and spotting or light bleeding for a few days. If you had general anesthesia, have someone stay with you for 24 hours. This is to make sure you do not have a reaction to the anesthesia. It may take a few months for your monthly period to start or become regular.
Risks of a D&C:
- If you are awake during your D&C, you may have pain while the tissue is removed. Your uterus, cervix, intestines, or nearby tissue may be torn or damaged. You may have life-threatening blood loss, and need a blood transfusion or another surgery. You may need to have your uterus removed. You may get an infection in your uterus that could spread to your blood and become life-threatening. You may have an allergic reaction to the anesthesia or antibiotics.
- After your D&C, you may have nausea, vomiting, dizziness, or a headache. Scar tissue may form in your uterus. You may need another D&C to remove more tissue from your uterus. If cancer caused your abnormal vaginal bleeding, lab tests may not find the cancer in your uterus. If your D&C was done to end a pregnancy, you have an increased risk for a future miscarriage. You are also at risk for preterm delivery during a future pregnancy.
Related medications
Call your local emergency number (911 in the US) if:
- You have signs of an allergic reaction, such as hives, trouble breathing, or severe swelling.
Seek care immediately if:
- You have heavy vaginal bleeding that soaks 1 pad in 1 hour for 2 hours in a row.
- You have a fever higher than 100.4°F (38°C).
- You have abdominal cramps for more than 2 days.
- Your pain does not get better, even after treatment.
Call your doctor or gynecologist if:
- You have foul-smelling vaginal discharge.
- You do not get your monthly period.
- You feel depressed or anxious.
- You feel very tired and weak.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics help fight or prevent a bacterial infection.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care:
- Use sanitary pads if needed. You may have light bleeding for up to 2 weeks. Do not use tampons. Use sanitary pads instead. This will help prevent a vaginal infection.
- Rest as needed. Slowly start to do more each day. Return to your daily activities as directed.
- Do not have sex for at least 2 weeks after the procedure. This will help prevent an infection.
- Use birth control right after your procedure. Your monthly period should start again in 4 to 8 weeks. During this time, you could still ovulate (release an egg). Use birth control as directed to prevent pregnancy during this time.
Follow up with your doctor or gynecologist as directed:
Your uterus will be checked to make sure it is healing. You may also be given results of any tests done on removed tissue. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
