Blood Thinners
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
What do I need to know about blood thinners?
Blood thinners are medicines that prevent blood clots from forming in an artery, vein, or the heart. These medicines may also prevent a blood clot from getting bigger. Blood clots prevent the flow of blood to organs and tissues such as the heart or a leg. The 2 main types of blood thinners are antiplatelet medicine and anticoagulant medicine. Antiplatelet medicine prevents platelets from sticking together and forming a clot. Anticoagulant medicine prevents the blood from clotting too much.
Why do I need to take a blood thinner?
- Antiplatelets may be given to prevent blood clots from happening anywhere in the body. You may need to take antiplatelet medicine if you have coronary artery disease, peripheral vascular disease, or have had a stroke or heart attack. You may also need to take antiplatelet medicine after you have an intravascular coronary stent placed.
- Anticoagulants may be given if you are at high risk for a stroke or have a condition called atrial fibrillation. Atrial fibrillation is an irregular heartbeat that makes the heart quiver instead of beat. This condition may cause blood to stay in the heart and cause blood clots to form there. Anticoagulants may also be given if you have blockages in blood vessels in your brain. You may need anticoagulants after a deep vein thrombosis (DVT), cardiac bypass graft, angioplasty, or vascular surgery.
What are the most common side effects of blood thinners?
The most common side effects of blood thinners are bleeding and bruising. Anticoagulants may cause bleeding in your brain, stomach, or other parts of your body. This bleeding may happen without an injury or trauma. This may become life-threatening and you may need other treatments to control the bleeding. Ask your healthcare provider about other side effects of your blood thinner.
Related medications
What are new oral anticoagulants (NOACs)?
NOACs are a type of anticoagulant medicine that has a lower risk for bleeding. Examples include dabigatran, rivaroxaban, apixaban, and edoxaban. You do not need routine blood tests if you take a NOAC. NOACs may be given to a person with a pulmonary embolism, DVT, atrial fibrillation, acute coronary syndrome, or to prevent a stroke or DVT.
Which foods and medicines should I avoid while I am taking anticoagulants?
Do not start any new medicines, vitamins, or herbal supplements before you talk to your healthcare provider. Do not make changes to your diet without talking to your provider. Many medicines, vitamins, and herbal supplements may prevent blood thinners from working correctly. Ask your provider for a full list of foods and medicines to avoid. The following may cause severe bleeding, or prevent anticoagulants from working correctly:
- Alcohol may increase your risk for bleeding when taken with anticoagulants. Do not drink alcohol unless your provider says it is okay.
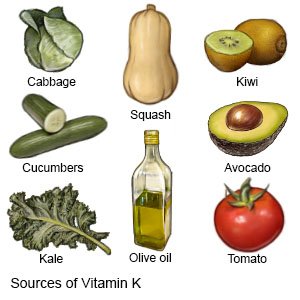
- Changes in your regular vitamin K intake can prevent warfarin from working correctly. Warfarin works best if you eat the same amount of vitamin K every day. Some foods that contain vitamin K include spinach, kale, broccoli, romaine lettuce, collard greens, and kiwi. Ask your provider for more information about foods that contain vitamin K.
- NSAIDs may increase your risk for bleeding. Examples include ibuprofen, aspirin, and naproxen. Do not take these medicines unless your provider says it is okay.
- Some antibiotics may increase your risk for bleeding. Talk to your provider before you take antibiotics.
- Alternative medicines such as ginkgo biloba, garlic, chamomile, and St. John's wort, should not be taken with anticoagulants. Some may prevent anticoagulants from working, and others may increase your risk for bleeding.
How can I care for myself while I take anticoagulants?
- Do not play contact sports. This may increase your risk for bleeding if you get injured or hit. Walk, swim, or do yoga to get exercise. Ask your healthcare provider about other exercises that are safe.
- Use an electric razor to shave. This may prevent cuts that could bleed.
- Use a soft bristled tooth brush and wax floss. This may prevent bleeding from your gums.
- Prevent falls in and out of your home. Wear non-slip shoes or slippers when you are out of bed. Keep walkways clear. Remove throw rugs and other objects that can cause you to trip and fall. Use assistive devices as directed.

- Be careful with sharp objects. Wear gloves when you work outside with sharp tools or in the garden.
- Use contraception to prevent a pregnancy. Anticoagulants can cause problems with your baby, and dangerous bleeding during pregnancy.
- Carry your medicine with you when you travel. This will prevent you from missing a dose of medicine if your bag gets lost. Talk to your provider before you travel.
- Wear or carry a medical alert bracelet or necklace at all times. This will alert healthcare providers that you take an anticoagulant if you are unconscious or need emergency medical treatment.

What else do I need to know about blood thinners?
- Tell all of your healthcare providers and dentist that you take a blood thinner. This will help them plan for procedures and surgeries. It will also prevent them from giving you medicine that may interact with your blood thinner.
- You should not take antiplatelet medicine if you have liver or kidney disease, a peptic ulcer, or gastrointestinal disease. You should also not take this medicine if you have a bleeding disorder, uncontrolled asthma, or uncontrolled high blood pressure. These conditions may increase your risk for bleeding.
- Take anticoagulants exactly as prescribed. Do not double up on a dose if you have missed a dose. Some anticoagulants should be taken at the same time every day.
- Keep appointments for blood tests if you are taking warfarin. Blood tests will help your provider make changes to your dose of anticoagulants so that they work correctly. The blood test will measure the amount of time it takes for your blood to clot. This is called the international normalized ratio (INR). If your INR is too high, you may be at an increased risk for bleeding. If your INR is too low, you may be at an increased risk for blood clots. Your provider may change the dose of your anticoagulant medicine depending on the results of your blood test.
Care Agreement
You have the right to help plan your care. Learn about your health condition and how it may be treated. Discuss treatment options with your healthcare providers to decide what care you want to receive. You always have the right to refuse treatment. The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
