Acute Bronchitis in Children
Medically reviewed by Drugs.com. Last updated on Sep 23, 2025.
AMBULATORY CARE:
Acute bronchitis
is swelling and irritation in your child's lungs. It is usually caused by a virus and most often happens in the winter. Bronchitis may also be caused by bacteria or by a chemical irritant, such as smoke.
 |
Common signs and symptoms include the following:
- Cough that lasts up to 3 weeks, stuffy nose
- Hoarseness, sore throat
- Fever, body aches, and chills
- Feeling more tired than usual
- Wheezing or pain when your child breathes or coughs
- Headache
Call your local emergency number (911 in the US) if:
- Your child is struggling to breathe. The signs may include:
- Skin between your child's ribs or around the neck being sucked in with each breath (retractions)
- Flaring (widening) of your child's nose when he or she breathes
- Trouble talking or eating
- Your child's lips or nails turn gray or blue.
- Your child is dizzy, confused, faints, or is much harder to wake than usual.
- Your child's breathing problems get worse, or he or she wheezes with every breath.
Seek care immediately if:
- Your child has a fever, headache, and stiff neck.
- Your child has signs of dehydration, such as crying without tears, a dry mouth, or cracked lips.
- Your child is urinating less, or his or her urine is darker than usual.
Related medications
Treatment options
The following list of medications are related to or used in the treatment of this condition.
Call your child's doctor if:
- Your child's fever goes away and then returns.
- Your child's cough lasts longer than 3 weeks or gets worse.
- Your child's symptoms do not go away or get worse, even after treatment.
- You have any questions or concerns about your child's condition or care.
Medicines:
Your child may need any of the following:
- Cough medicine helps loosen mucus in your child's lungs and makes it easier to cough up. Do not give cold or cough medicines to children under 4 years of age. Ask your healthcare provider if you can give cough medicine to your child.
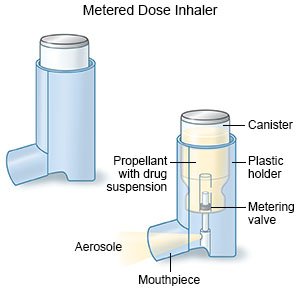
- An inhaler gives medicine in a mist form so that your child can breathe it into his or her lungs. Ask your child's healthcare provider to show you or your child how to use the inhaler correctly.
- Antibiotics may be given if your child's bronchitis is caused by bacteria.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to give your child and how often to give it. Follow directions. Read the labels of all other medicines your child uses to see if they also contain acetaminophen, or ask your child's doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- NSAIDs , such as ibuprofen, help decrease swelling, pain, and fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If your child takes blood thinner medicine, always ask if NSAIDs are safe for him or her. Always read the medicine label and follow directions. Do not give these medicines to children younger than 6 months without direction from a healthcare provider.
- Do not give aspirin to children younger than 18 years. Your child could develop Reye syndrome if he or she has the flu or a fever and takes aspirin. Reye syndrome can cause life-threatening brain and liver damage. Check your child's medicine labels for aspirin or salicylates.
- Give your child's medicine as directed. Contact your child's healthcare provider if you think the medicine is not working as expected. Tell the provider if your child is allergic to any medicine. Keep a current list of the medicines, vitamins, and herbs your child takes. Include the amounts, and when, how, and why they are taken. Bring the list or the medicines in their containers to follow-up visits. Carry your child's medicine list with you in case of an emergency.
Manage your child's symptoms:
- Have your child drink liquids as directed. Your child may need to drink more liquids than usual to stay hydrated. Ask how much your child should drink each day and which liquids are best for him or her. If you are breastfeeding or feeding your child formula, continue to do so. Your baby may not feel like drinking his or her regular amounts with each feeding. You may need to feed your baby smaller amounts of breast milk or formula more often.
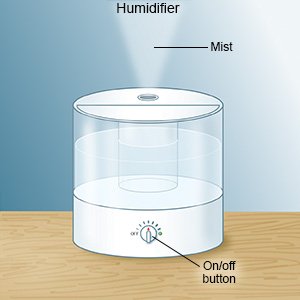
- Use a cool mist humidifier. This increases air moisture in your home. This may make it easier for your child to breathe and help decrease his or her cough.
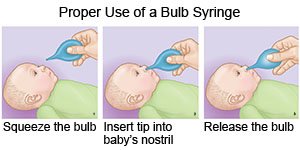
- Clear mucus from your baby's nose. Use a bulb syringe to remove mucus from your baby's nose. Squeeze the bulb and put the tip into one of your baby's nostrils. Gently close the other nostril with your finger. Slowly release the bulb to suck up the mucus. Empty the bulb syringe onto a tissue. Repeat the steps if needed. Do the same thing in the other nostril. Make sure your baby's nose is clear before he or she feeds or sleeps. The healthcare provider may recommend you put saline drops into your baby's nose if the mucus is very thick.
Prevent acute bronchitis:
 |
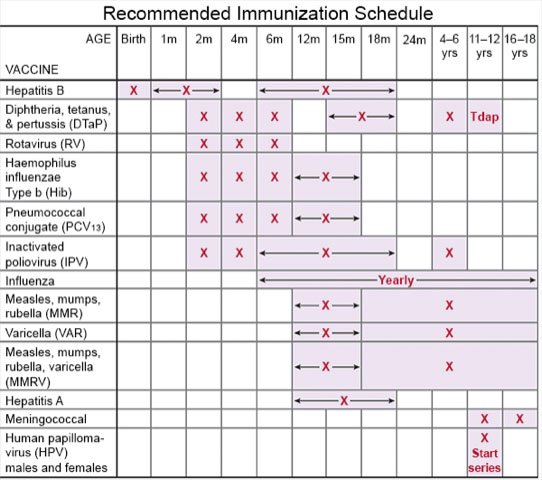
- Ask about vaccines your child may need. Have your child get a flu vaccine each year as soon as recommended, usually in September or October. Ask your child's healthcare provider if your child should also get a pneumonia or COVID-19 vaccine. Your child's provider can tell you other vaccines your child needs, and when he or she should get them.
- Prevent the spread of germs:
- Have your child wash his or her hands often with soap and water. Carry germ-killing hand lotion or gel with you. Have your child use the lotion or gel to clean his or her hands when soap and water are not available.

- Remind your child not to touch his or her eyes, nose, or mouth unless he or she has washed hands first.
- Remind your child to cover his or her mouth while coughing or sneezing to prevent the spread of germs. Have your child cough or sneeze into his or her shirt sleeve or a tissue. Ask those around your child to cover their mouths when they cough or sneeze.
- Try to have your child avoid people who have a cold or the flu. Your child should stay away from others as much as possible.
- Have your child wash his or her hands often with soap and water. Carry germ-killing hand lotion or gel with you. Have your child use the lotion or gel to clean his or her hands when soap and water are not available.
- Do not smoke or allow others to smoke around your child. Nicotine and other chemicals in cigarettes and cigars can cause lung damage. Ask your healthcare provider for information if you currently smoke and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your provider before you use these products.
Follow up with your child's doctor as directed:
Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Learn more about Acute Bronchitis
Treatment options
Care guides
- Acute Bronchitis
- Acute Bronchitis in Children
- Bronchiolitis
- Chronic Bronchitis
- Reactive Airways Disease
Symptoms and treatments
Medicine.com guides (external)
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
