Primaquine (Monograph)
Drug class: Antimalarials
VA class: AP101
CAS number: 63-45-6
Introduction
Antimalarial; 8-aminoquinoline derivative.
Uses for Primaquine
Malaria
Treatment of malaria caused by Plasmodium vivax or P. ovale† [off-label]. Provides a radical cure to prevent relapse of malaria caused by these Plasmodium. Has only low activity against asexual erythrocytic forms of Plasmodium; a regimen that includes a blood schizonticidal agent (e.g., chloroquine [or hydroxychloroquine]; quinine with doxycycline or tetracycline; mefloquine; fixed-combination of atovaquone and proguanil [atovaquone/proguanil]; fixed combination of artemether and lumefantrine [artemether/lumefantrine]) is always used in conjunction with primaquine for treatment of P. ovale or P. vivax malaria.
Presumptive antirelapse therapy (terminal prophylaxis) in travelers who received a suitable antimalarial for prevention of malaria but are returning from areas where P. vivax or P. ovale is endemic. If primaquine not used for terminal prophylaxis in individuals who may have been exposed to P. ovale or P. vivax malaria, delayed primary attacks or relapse caused by these Plasmodium can occur.
Prevention of malaria† [off-label] (primary prophylaxis). Primaquine may be an option when other recommended antimalarials (choroquine [or hydroxychloroquine], atovaquone/proguanil, doxycycline, mefloquine) cannot be used for primary prophylaxis and is a good choice when travelers will be in areas with high incidence of P. vivax malaria. If primaquine is used for primary prophylaxis, primaquine presumptive antirelapse therapy is not needed.
Assistance with diagnosis or treatment of malaria is available from CDC Malaria Hotline at 770-488-7788 or 855-856-4713 from 9:00 a.m. to 5:00 p.m. Eastern Standard Time or CDC Emergency Operation Center at 770-488-7100 after hours and on weekends and holidays.
Information on risk of malaria in specific countries and mosquito avoidance measures and recommendations regarding whether prevention of malaria is indicated and choice of antimalarials for prevention are available from CDC at [Web] and [Web].
Pneumocystis jirovecii Pneumonia
Treatment of Pneumocystis jirovecii (formerly Pneumocystis carinii) pneumonia† [off-label] (PCP); used in conjunction with clindamycin. Designated an orphan drug by FDA for use in conjunction with clindamycin for treatment of PCP associated with AIDS.
Co-trimoxazole is drug of choice for treatment of mild, moderate, or severe PCP, including PCP in HIV-infected adults, adolescents, and children. CDC, NIH, and IDSA state that a regimen of primaquine and clindamycin is an alternative for treatment of mild, moderate, or severe PCP in HIV-infected adults and adolescents who have had an inadequate response to co-trimoxazole or when co-trimoxazole is contraindicated or not tolerated. Although data not available regarding use in children, CDC, NIH, IDSA, and AAP state that a regimen of primaquine and clindamycin also can be considered an alternative to co-trimoxazole for treatment of PCP in HIV-infected children based on data in adults.
Not recommended for prevention of initial episodes (primary prophylaxis) of PCP in HIV-infected individuals because data insufficient to determine efficacy; not included in recommendations for long-term suppressive or chronic maintenance therapy (secondary prophylaxis) of PCP. Co-trimoxazole is drug of choice for primary and secondary prophylaxis of PCP in HIV-infected adults, adolescents, and children.
Primaquine Dosage and Administration
General
-
Prior to use, perform appropriate laboratory tests to rule out glucose-6-phosphate dehydrogenase (G6PD) deficiency. (See Hemolytic Anemia and G6PD Deficiency under Cautions.)
Administration
Oral Administration
Administer orally; usually as a single daily dose at the same time each day.
Take with food to decrease adverse GI effects (e.g., nausea, abdominal pain).
Dosage
Available as primaquine phosphate; dosage usually expressed in terms of primaquine.
Each 26.3-mg tablet of primaquine phosphate contains 15 mg of primaquine.
Pediatric Patients
Malaria
Radical Cure of P. ovale or P. vivax Malaria
Oral0.5 mg/kg (0.8 mg/kg of primaquine phosphate) once daily for 14 days.
Presumptive Antirelapse Therapy (Terminal Prophylaxis) of P. ovale or P. vivax Malaria
Oral0.5 mg/kg (0.8 mg/kg of primaquine phosphate) once daily for 14 days given after leaving malarious area.
Individuals who received primary prophylaxis with chloroquine, hydroxychloroquine, doxycycline, or mefloquine: Administer primaquine presumptive antirelapse therapy during final 2 weeks of primary prophylaxis or, if not feasible, administer for 14 days after primary prophylaxis discontinued.
Individuals who received primary prophylaxis with atovaquone/proguanil: Administer primaquine presumptive antirelapse therapy during final 7 days of primary prophylaxis and then for an additional 7 days or, if not feasible, administer for 14 days after primary prophylaxis discontinued.
Primary Prophylaxis of Malaria† [off-label]
Oral0.5 mg/kg (0.8 mg/kg of primaquine phosphate) once daily.
Initiate prophylaxis 1–2 days prior to entering a malarious area and continue during stay and for 7 days after leaving the area.
Pneumocystis jirovecii Pneumonia (PCP)† [off-label]
Treatment of PCP in HIV-infected Children†
Oral0.3 mg/kg (up to 30 mg) once daily for 21 days; used in conjunction with clindamycin (10 mg/kg [up to 600 mg] IV every 6 hours or 10 mg/kg [up to 300–450 mg] orally every 6 hours) given for 21 days.
Treatment of Mild to Moderate PCP in HIV-infected Adolescents†
Oral30 mg once daily for 21 days; used in conjunction with oral clindamycin (450 mg every 6 hours or 600 mg every 8 hours) given for 21 days.
Treatment of Moderate to Severe PCP in HIV-infected Adolescents†
Oral30 mg once daily for 21 days; used in conjunction with IV clindamycin (600 mg every 6 hours or 900 mg every 8 hours) or oral clindamycin (450 mg every 6 hours or 600 mg every 8 hours) given for 21 days.
Adults
Malaria
Radical Cure of P. ovale or P. vivax Malaria
Oral30 mg of primaquine (52.6 mg of primaquine phosphate) once daily for 14 days recommended by CDC and others. Although manufacturer recommends 15 mg of primaquine (26.3 mg of primaquine phosphate) once daily for 14 days, this dosage may be inadequate if malaria is acquired in Southeast Asia (particularly Indonesia and Oceania).
As an alternative to the daily regimen or if used in patients with borderline G6PD deficiency, CDC recommends 45 mg of primaquine (79 mg of primaquine phosphate) once weekly for 8 weeks. Consultation with an expert in infectious disease and/or tropical medicine recommended if this regimen considered for individuals with borderline G6PD deficiency. (See Hemolytic Anemia and G6PD Deficiency under Cautions.)
Presumptive Antirelapse Therapy (Terminal Prophylaxis) of P. ovale or P. vivax Malaria
Oral30 mg of primaquine (52.6 mg of primaquine phosphate) once daily for 14 days given after leaving malarious areas recommended by CDC and others. Although manufacturer recommends 15 mg of primaquine (26.3 mg of primaquine phosphate) once daily for 14 days, this dosage may be inadequate in areas with P. vivax that are relatively resistant to primaquine (e.g., Oceania).
Individuals who received primary prophylaxis with chloroquine, hydroxychloroquine, doxycycline, or mefloquine: Administer primaquine presumptive antirelapse therapy during final 2 weeks of primary prophylaxis or, if not feasible, administer for 14 days after primary prophylaxis discontinued.
Individuals who received primary prophylaxis with atovaquone/proguanil: Administer primaquine presumptive antirelapse therapy during final 7 days of primary prophylaxis and then for an additional 7 days or, if not feasible, administer for 14 days after primary prophylaxis discontinued.
Primary Prophylaxis of Malaria†
Oral30 mg of primaquine once daily.
Initiate prophylaxis 1–2 days prior to entering a malarious area and continue during stay and for 7 days after leaving the area.
Pneumocystis jirovecii Pneumonia (PCP)†
Treatment of Mild to Moderate PCP†
Oral30 mg once daily for 21 days; used in conjunction with oral clindamycin (450 mg every 6 hours or 600 mg every 8 hours) given for 21 days.
Treatment of Moderate to Severe PCP†
Oral30 mg once daily for 21 days; used in conjunction with IV clindamycin (600 mg every 6 hours or 900 mg every 8 hours) or oral clindamycin (450 mg every 6 hours or 600 mg every 8 hours) given for 21 days.
Prescribing Limits
Pediatric Patients
Malaria
Treatment or Prevention of Malaria
OralDo not exceed adult dosage.
Adults
Malaria
Treatment or Prevention of Malaria
OralManufacturer states do not exceed 15 mg of primaquine (26.3 mg of primaquine phosphate) once daily for 14 days; CDC and others recommend 30 mg of primaquine (52.6 mg of primaquine phosphate) once daily.
Special Populations
Hepatic Impairment
No specific dosage recommendations.
Renal Impairment
No specific dosage recommendations.
Geriatric Adults
Select dosage with caution because of age-related decreases in hepatic, renal, and/or cardiac function and concomitant disease and drug therapy.
Cautions for Primaquine
Contraindications
-
Severe G6PD deficiency. (See Hemolytic Anemia and G6PD Deficiency under Cautions.)
-
Pregnant women. (See Pregnancy under Cautions.)
-
Acutely ill patients who have systemic disease manifested by a tendency to develop granulocytopenia (e.g., rheumatoid arthritis, lupus erythematosus).
-
Patients receiving other potentially hemolytic drugs or agents capable of depressing the myeloid elements of bone marrow.
Warnings/Precautions
Warnings
Hemolytic Anemia and G6PD Deficiency
Hemolytic reactions (moderate to severe) may occur if used in individuals with G6PD deficiency or in individuals with family or personal history of favism. Hemolytic reactions can be fatal.
Perform appropriate laboratory testing to rule out G6PD deficiency before initiating primaquine.
Severe G6PD deficiency: Do not prescribe primaquine.
Mild to moderate G6PD deficiency: Base decision to prescribe primaquine on an assessment of risks and benefits. If use of the drug is considered, evaluate baseline hematocrit and hemoglobin concentration before treatment and closely monitor hematologic parameters during treatment (e.g., at days 3 and 8).
G6PD status unknown and G6PD testing unavailable: Base decision to prescribe primaquine on an assessment of risks and benefits. Assess risk factors for G6PD deficiency or favism. If use of the drug is considered, evaluate baseline hematocrit and hemoglobin concentration before treatment and closely monitor hematologic parameters during treatment (e.g., at days 3 and 8).
Consider that residual risk of hemolysis exists despite G6PD testing because of limitations of the tests. Routine hematologic monitoring (particularly CBCs and hemoglobin concentrations) is advisable during primaquine therapy, even in G6PD-normal individuals.
Do not exceed recommended dosage.
Monitor closely if used in individuals who have had a previous idiosyncratic reaction to primaquine (as manifested by hemolytic anemia, methemoglobinemia, or leukopenia) or in individuals with a personal or family history of hemolytic anemia or nicotinamide adenine dinucleotide (NADH) methemoglobin reductase deficiency.
Discontinue immediately if evidence of hemolytic anemia occurs (e.g., darkening of urine, marked fall in hemoglobin concentration or erythrocyte count) or if leukocyte count suddenly decreases.
Ensure that adequate medical support and follow-up to manage hemolytic risk are available for all patients receiving primaquine.
Cardiac Effects
Cardiac arrhythmia and prolonged QT interval reported.
Because of potential for QT interval prolongation, monitor ECG if used in patients with cardiac disease, long QT syndrome, history of ventricular arrhythmias, uncorrected hypokalemia and/or hypomagnesemia, or bradycardia (<50 bpm) and whenever used concomitantly with drugs that prolong the QT interval.
Females and Males of Reproductive Potential
Sexually active females of reproductive potential: Perform pregnancy test prior to initiation of primaquine; pregnancy must be avoided during and after treatment until an ongoing ovulatory cycle has been completed. (See Pregnancy under Cautions.)
Sexually active males whose partners may become pregnant: Use condom during primaquine treatment and for 3 months after the drug discontinued. (See Pregnancy under Cautions.)
General Precautions
GI Effects
Nausea, vomiting, epigastric distress, and abdominal cramps reported; incidence and severity appear to be dose related.
Adverse GI effects may be decreased by administration with food.
Specific Populations
Pregnancy
Contraindicated during pregnancy. Safe use during pregnancy not established. In addition, transplacental transfer of the drug to a G6PD-deficient fetus potentially could cause hemolytic anemia in utero.
In animals, has been associated with teratogenicity and injury to embryos and developing fetuses. Inform patients of potential for adverse genetic and reproductive effects.
Test all sexually active females of reproductive potential for pregnancy prior to initiation of primaquine. Advise such women to use effective contraception (i.e., methods with pregnancy rates <1%) during and after primaquine therapy until an ongoing ovulatory cycle has been completed (up to next menses). Advise sexually active males whose partners may become pregnant to use a condom during and for 3 months after primaquine therapy.
If a pregnant woman requires treatment of P. vivax or P. ovale malaria, CDC recommends use of oral chloroquine (300 mg once weekly) for prophylaxis for duration of the pregnancy and deferral of primaquine (to provide a radical cure) until after delivery and after the woman has been tested and determined not to have G6PD deficiency.
Lactation
Distributed into milk in low concentrations.
Manufacturer states discontinue nursing or the drug, taking into account importance of the drug to the mother.
CDC states do not use in nursing women unless the woman and breast-fed infant have been determined not to have G6PD deficiency.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults.
Select dosage with caution (starting at the low end of dosage range) because of age-related decreases in hepatic, renal, and/or cardiac function and potential for concomitant disease and drug therapy.
Common Adverse Effects
Hematologic effects (hemolytic anemia, leukocytosis, leukopenia); GI effects (nausea, vomiting, epigastric distress, abdominal cramps).
Drug Interactions
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Drugs that prolong QT interval |
Use concomitantly with caution and monitor ECG |
|
|
Quinacrine |
Quinacrine (not available in US) potentiates toxicity of antimalarials structurally related to primaquine |
Concomitant use contraindicated; do not use primaquine in individuals who recently received quinacrine |
Primaquine Pharmacokinetics
Absorption
Bioavailability
Rapidly and well absorbed from GI tract. Peak plasma concentrations generally attained within 2–4 hours.
Pharmacokinetics are altered during malaria infection; peak plasma concentrations may be higher in adults with malaria compared with healthy adults.
Food
In healthy adults, administration with food (approximately 28 g of fat) resulted in 1.23-fold increase in peak plasma concentration and 1.12-fold increase in AUC compared with administration in fasting state.
Distribution
Extent
Widely distributed following oral administration.
Low concentrations distributed into milk.
Elimination
Metabolism
Extensively and rapidly metabolized in the liver. The principal metabolite is carboxyprimaquine; plasma concentrations of the metabolite greatly exceed those of unchanged primaquine.
Elimination Route
Only small amounts excreted unchanged in urine.
Half-life
4–7 hours.
Stability
Storage
Oral
Tablets
25°C (may be exposed to 15–30°C); store in tight, light-resistant container.
Actions and Spectrum
-
Antimalarial.
-
Tissue schizonticidal agent active against the preerythrocytic and exoerythrocytic forms of Plasmodium falciparum, P. malariae, P. ovale, and P. vivax. Also gametocytocidal against P. falciparum and other Plasmodium.
-
Has only low activity against the erythrocytic forms of Plasmodium.
-
Primaquine-resistant and primaquine-tolerant P. vivax reported.
-
Exact mechanism of antimalarial activity unknown; appears to cause morphologic and physiologic changes in plasmodial mitochondria. In the treatment of malaria caused by P. vivax, primaquine eliminates tissue (exoerythrocytic) infection thereby preventing development of blood (erythrocytic) forms of the parasite that are responsible for relapse of P. vivax malaria.
-
Mechanism of action against P. jirovecii unknown.
-
Necessity of taking protective measures to reduce contact with mosquitoes (protective clothing, insect repellents, mosquito nets, remaining in air-conditioned or well-screened areas).
-
Possibility of contracting malaria during travel, regardless of prophylactic regimen used.
-
Importance of seeking medical attention as soon as possible if febrile illness develops during or after return from a malaria-endemic area and of informing clinician of possible malaria exposure.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, and any concomitant illnesses.
-
Importance of women informing clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise sexually active females and males of the importance of taking precautions to avoid pregnancy during and after primaquine therapy. (See Pregnancy under Cautions.)
-
Importance of advising patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
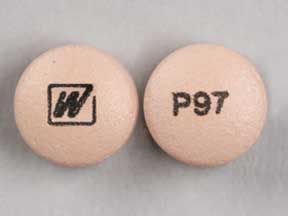
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
15 mg (of primaquine)* |
Primaquine Phosphate Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 18, 2018. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
More about primaquine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimalarial quinolines
- Breastfeeding
- En español