Methamphetamine (Monograph)
Drug class: Amphetamines
Warning
- Abuse, Misuse, and Addiction
-
High potential for abuse and misuse, which can lead to substance use disorder, including addiction. Misuse and abuse of CNS stimulants such as methamphetamine can lead to overdose and death.
-
Assess risk of abuse, misuse, and addiction prior to prescribing. Throughout treatment, reassess each patient’s risk and frequently monitor for signs of abuse, misuse, and addiction.
Introduction
CNS stimulant.
Uses for Methamphetamine
Attention Deficit Hyperactivity Disorder (ADHD)
Used for the treatment of ADHD in pediatric patients ≥6 years of age.
Use is rare due to the overall risks versus benefits of this agent. There is high potential for abuse that can lead to development of a substance use disorder. Long-term abuse of methamphetamine leads to neurodegenerative changes in the brain.
American Academy of Pediatrics (AAP) states that, for pediatric patients 6–12 years of age with ADHD, provider should prescribe FDA-approved medications, in addition to parent training in behavior management (PTBM) and/or behavioral classroom interventions. Evidence is stated as particularly strong for stimulant medications (e.g., amphetamines, methylphenidate). For adolescents 12–18 years of age with ADHD, provider should prescribe FDA-approved medications with assent of the adolescent. Provider is also encouraged to prescribe behavioral and other evidence-based training interventions if available. Titrate doses of medications to achieve maximum benefit with tolerable side effects. Methamphetamine not included in these guidelines.
Methamphetamine Dosage and Administration
General
Pretreatment Screening
-
Evaluate patients for risk of abuse, misuse, and addiction prior to initiation of CNS stimulant therapy.
-
Children, adolescents, and adults being considered for stimulant therapy should undergo a thorough medical history review (including evaluation for a family history of sudden death or ventricular arrhythmia) and physical examination to detect the presence of cardiac disease.
-
Prior to initiating stimulant therapy, screen patients with attention deficit hyperactivity disorder (ADHD) carefully to determine if they are at risk for developing a manic episode; such screening should include a detailed psychiatric history (e.g., current or prior depressive symptoms; family history of suicide, bipolar disorder, or depression).
-
Prior to initiation of therapy, screen patients for motor or verbal tics or Tourette’s syndrome.
Patient Monitoring
-
Routinely monitor for the emergence or worsening of tics or Tourette’s syndrome.
-
Monitor growth (weight and height) closely in pediatric patients receiving stimulant therapy.
-
Throughout treatment, reassess each patient’s risk of abuse, misuse, and addiction. Frequently monitor for signs of abuse, misuse, and addiction during treatment.
-
Monitor for hypertension and tachycardia during stimulant therapy.
Dispensing and Administration Precautions
- Handling and Disposal
-
Methamphetamine should be disposed of by a medicine take-back program at a U.S. Drug Enforcement Administration (DEA) authorized collection site when it is no longer needed. If there is no take-back program or authorized DEA collection site available, the drug can be mixed with an undesirable, nontoxic substance such as dirt, cat litter, or used coffee grounds and disposed of in a sealed plastic bag in the household trash.
Administration
Oral Administration
Because of potential for insomnia, avoid administering doses in the late evening.
Dosage
Available as methamphetamine hydrochloride; dosage expressed in terms of the salt.
Adjust dosage according to individual response and tolerance; the smallest dose required to produce the desired response should always be used.
When possible, therapy should be interrupted occasionally to determine if there is a recurrence of behavioral symptoms sufficient to require continued treatment.
Pediatric Patients
Attention Deficit Hyperactivity Disorder
Oral
Children ≥6 years of age: Initially, 5 mg once or twice daily; daily dosage is increased in 5-mg increments at weekly intervals until the optimum response is attained.
Usual dosage is 20–25 mg daily, given once daily or in 2 divided doses.
Special Populations
Hepatic Impairment
No specific dosage recommendations.
Renal Impairment
No specific dosage recommendations.
Geriatric Patients
Select dosage with caution, usually starting at the low end of the dosage range, because of age-related decreases in hepatic, renal, or cardiac function, and of concomitant disease or other drug therapy.
Cautions for Methamphetamine
Contraindications
-
Concomitant or recent (within 14 days) administration of monoamine oxidase inhibitors (MAOIs), since hypertensive crisis could result.
-
Known hypersensitivity to amphetamine, or any ingredient in methamphetamine hydrochloride tablets. Hypersensitivity reactions, including anaphylaxis and angioedema, have been reported in patients taking other amphetamine products.
Warnings/Precautions
Warnings
Abuse, Misuse, and Addiction
Amphetamines expose patients to the risks of abuse and misuse, which can lead to the development of substance use disorder (including addiction; see Boxed Warning). Misuse and abuse of CNS stimulants may result in overdose or death. Risk further increased with higher dosages or unapproved routes of administration (i.e., snorting, injection). Monitor patients for signs of abuse, misuse, and addiction during treatment. Tolerance can also occur. Advise patients and/or caregivers to not share amphetamines with others and to store the drug in a safe (preferably locked) location to prevent misuse and abuse.
Other Warnings/Precautions
Risks to Patients with Serious Cardiac Disease
Sudden unexplained death reported in patients with structural cardiac abnormalities or other serious cardiac conditions receiving usual dosages of stimulants for ADHD.
Thoroughly review medical history (including evaluation for family history of sudden death or ventricular arrhythmia) and perform physical examination in all children, adolescents, and adults being considered for stimulant therapy.
In general, avoid use of CNS stimulants in adults or children with known serious structural cardiac abnormalities, cardiomyopathy, serious heart rhythm abnormalities, CAD, or other serious cardiac disease.
Increased Blood Pressure and Heart Rate
Possible modest increases in average BP (i.e., by about 2–4 mm Hg) and heart rate (i.e., by about 3–6 bpm); larger increases may occur. Monitor all patients for hypertension and tachycardia.
Psychiatric Adverse Reactions
May exacerbate symptoms of behavior disturbance and thought disorder in patients with preexisting psychotic disorder.
Psychotic (e.g., hallucinations, delusional thinking) or manic symptoms may occur with usual dosages in children and adolescents without prior history of psychotic illness. If psychotic or manic symptoms occur, consider causal relationship to stimulants, and discontinue therapy as appropriate.
May precipitate mixed or manic episodes in ADHD patients with comorbid bipolar disorder; use with caution in these patients. Prior to initiating therapy, carefully screen patients with ADHD and comorbid depressive symptoms to identify risk for bipolar disorder; screening should include a detailed psychiatric history (e.g., family history of suicide, bipolar disorder, or depression).
Long-term Suppression of Growth in Pediatric Patients
Long-term administration expected to cause suppression of normal weight and/or height patterns in some children and adolescents.
Manufacturer recommends closely monitoring growth during treatment; patients not growing or gaining weight as expected may require temporary discontinuance of treatment.
Seizures
Possible lowering of seizure threshold in patients with history of seizures, in those with prior EEG abnormalities but no history of seizures, and, very rarely, in those without history of seizures and with no prior EEG abnormalities. If seizures occur, discontinue therapy.
Peripheral Vasculopathy Including Raynaud's Phenomenon
Stimulants used to treat ADHD are associated with peripheral vascular disorders, including Raynaud’s phenomenon. Careful observation for digital changes warranted during stimulant therapy; further clinical evaluation (e.g., referral to rheumatologist) may be appropriate for certain patients who develop signs and symptoms of peripheral vasculopathy.
Serotonin Syndrome
Potentially fatal serotonin syndrome possible when amphetamines are used with other medications that affect serotonergic neurotransmitters, such as MAOIs, SSRIs, SNRIs, triptans, tricyclic antidepressants, fentanyl, lithium, tramadol, tryptophan, buspirone, and St. John’s Wort (Hypericum perforatum).
Amphetamines and amphetamine derivatives metabolized to some extent by CYP2D6 and to a minor extent, inhibit CYP2D6. In patients receiving concomitant CYP2D6 inhibitors, consider an alternate nonserotonergic drug or drug that does not inhibit CYP2D6.
Only use amphetamines with other serotonergic drugs or CYP2D6 inhibitors if potential benefits justify the potential risks. If clinically feasible, consider initiating amphetamine therapy at a lower dose and monitor patients for emergence of serotonin syndrome during therapy initiation or titration. If symptoms of serotonin syndrome occur, immediately discontinue amphetamines and any concomitant serotonergic agents, and initiate supportive care.
Motor and Verbal Tics and Worsening of Tourette's Syndrome
Amphetamines reported to exacerbate motor and phonic tics and Tourette’s syndrome. Screen for family history and clinically evaluate for presence of motor or verbal tics or Tourette’s syndrome prior to initiating stimulant therapy. Routinely monitor patients for emergence or worsening of tics or Tourette’s syndrome, and discontinue amphetamines if clinically needed.
Specific Populations
Pregnancy
National Pregnancy Registry for Psychostimulants available at 1-866-966-2388 and [Web].
Teratogenic and embryocidal effects observed in mammals receiving doses exceeding the usual therapeutic human dosage.
Risk of prematurity, low birth weight, and withdrawal symptoms (e.g., dysphoria, lassitude, significant agitation) in infants born to dependent women.
Do not use during pregnancy unless the potential benefits justify the possible risks to the fetus.
Lactation
Amphetamines are distributed into human milk. Avoid breastfeeding during therapy with amphetamines.
Pediatric Use
Not recommended for treatment of ADHD in pediatric patients <6 years of age.
Long-term administration expected to cause suppression of normal weight and/or height patterns in some children and adolescents.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Other clinical experience has not identified differences in responses between geriatric and younger patients.
Select dosage with caution in geriatric patients, starting at the low end of the dosage range.
Hepatic Impairment
Not studied in hepatic impairment.
Renal Impairment
Not studied in renal impairment.
Common Adverse Effects
Elevation of BP, tachycardia, palpitations, fatal cardiopulmonary in the context of drug abuse/misuse, psychotic episodes, dizziness, dysphoria, overstimulation, euphoria, insomnia, tremor, restlessness, headache, exacerbation of motor and verbal tics and Tourette’s syndrome, diarrhea, constipation, dry mouth, unpleasant taste, intestinal ischemia, other GI disturbances, urticaria, impotence, changes in libido, frequent or prolonged erections, rhabdomyolysis, suppression of growth in children with long-term use, and alopecia.
Drug Interactions
Amphetamines and amphetamine derivatives are metabolized to some extent by CYP2D6, and to a minor extent, inhibit CYP2D6 metabolism.
CYP2D6 Inhibitors
Concomitant use of methamphetamine with CYP2D6 inhibitors (e.g., fluoxetine, paroxetine, quinidine, ritonavir) may increase amphetamine exposure and risk of serotonin syndrome.
If used with CYP2D6 inhibitors, initiate methamphetamine at lower dosages and monitor for signs and symptoms of serotonin syndrome, especially during initiation and dosage increases. If serotonin syndrome occurs, discontinue methamphetamine therapy and the CYP2D6 inhibitor.
Specific Drugs
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
5-hydroxytryptamine type 1 (5-HT1) agonists (“triptans”) |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
Acidifying agents, GI (e.g., guanethidine, reserpine, glutamic acid, ascorbic acid) |
Decreases serum concentrations and efficacy of amphetamines |
Dosage increase of methamphetamine may be warranted based on clinical response |
|
Acidifying agents, urinary (e.g., ammonium chloride, sodium acid phosphate, methenamine) |
Decreases serum concentrations and efficacy of amphetamines |
Dosage increase of methamphetamine may be warranted based on clinical response |
|
Alkalinizing agents, GI (e.g., sodium bicarbonate) |
Increases serum concentrations and potentiates the effects of amphetamines |
Avoid concomitant use of GI alkalinizing agents |
|
Alkalinizing agents, urinary (e.g., acetazolamide, some thiazides) |
Increases serum concentrations and potentiates the effects of amphetamines |
|
|
Antidepressants, tricyclic (e.g., desipramine, protriptyline) |
Significant increases in the concentration of d-amphetamine in the brain; cardiovascular effects can be potentiated Increased risk of serotonin syndrome |
Use concomitantly under close supervision; adjust dosage or use alternate drug therapy based on clinical response |
|
Buspirone |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
Fentanyl |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
Lithium |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
MAO inhibitors (MAOIs, e.g., selegiline, tranylcypromine, isocarboxazid, phenelzine, linezolid, methylene blue) |
Concomitant or recent use can cause hypertensive crisis, death, stroke, myocardial infarction, aortic dissection, ophthalmological complications, eclampsia, pulmonary edema, and renal failure |
Methamphetamine contraindicated in patients currently or recently (within 14 days) receiving MAOIs |
|
Phenothiazines |
Possible antagonism of CNS stimulant action of amphetamines |
|
|
Proton pump inhibitors (e.g., omeprazole) |
Rate of amphetamine absorption increased |
Monitor patients for clinical changes and adjust therapy based on clinical response |
|
SSRIs and SNRIs |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
St. John's Wort (Hypericum perforatum) |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
Tramadol |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
|
Tryptophan |
Increased risk of serotonin syndrome |
Initiate methamphetamine therapy at a reduced dosage and monitor for emergence of serotonin syndrome during therapy initiation or titration; if serotonin syndrome occurs, discontinue both drugs |
Methamphetamine Pharmacokinetics
Absorption
Bioavailability
Readily and rapidly absorbed from the GI tract.
Distribution
Extent
Amphetamines are distributed into human milk.
Elimination
Metabolism
Metabolized in the liver by aromatic hydroxylation, N-dealkylation, and deamination.
Elimination Route
Excreted principally in urine. With normal urinary pH, approximately 62% of the dose is excreted in urine within the first 24 hours as unchanged drug (about 1/3) and metabolites (about 2/3).
Excretion is enhanced in acidic urine.
Half-life
4–5 hours. Alkaline urine substantially increases half-life.
Stability
Storage
Oral
Tablets
Tight, light-resistant, child-resistant containers at 20–25°C.
Actions
-
Sympathomimetic amine with CNS stimulant activity.
-
Also causes elevations in systolic and diastolic blood pressure, weak bronchodilation, and respiratory stimulation.
Advice to Patients
-
Provide the patient or caregiver with a copy of the manufacturer’s patient information (medication guide).
-
Risk of abuse, misuse, and addiction, which can lead to overdose and death. Advise patients not to share methamphetamine with others and store the drug in a safe (preferably locked) location to prevent abuse. Advise patient or caregiver on proper disposal of any remaining unused or expired drug.
-
Potential risks to patients with serious cardiac disease, including sudden death. Advise patients to inform their clinicians immediately of any adverse cardiovascular effects (e.g., chest pain, shortness of breath, or fainting).
-
Inform patients that methamphetamine may impair the ability to operate machinery or drive a motor vehicle.
-
Advise patients or caregivers that methamphetamine can elevate blood pressure and pulse rate.
-
Advise patients that recommended dosages of methamphetamine may cause psychotic or manic symptoms, even in patients without a history of psychotic symptoms or mania.
-
Inform patients or caregivers about the risk of peripheral vascular disorders, including Raynaud's phenomenon, and the associated signs and symptoms (e.g., feelings of numbness, coolness, or pain in fingers or toes; changes in color from pale to blue to red). Advise patients to report any new numbness, pain, skin color change, or sensitivity to temperature in fingers or toes to their clinician and to immediately contact their clinician if any signs of unexplained wounds appear on fingers or toes; further clinical evaluation may be appropriate.
-
Advise patients that methamphetamine may slow growth and cause weight loss in children.
-
Inform patients that motor and verbal tics and worsening of Tourette’s syndrome can occur during stimulant therapy. Advise patients to notify their clinician if they experience new or worsening tics or Tourette’s syndrome.
-
Advise patients to inform their clinician if they are or plan to become pregnant or plan to breast-feed. Inform patients about the existence of a pregnancy registry for ADHD medications.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses/conditions (e.g., cardiac/cardiovascular disease, mental/psychiatric disorder, suicidal ideation or behaviors, history of substance abuse).
-
Advise patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
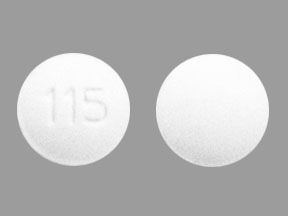
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
5 mg* |
Methamphetamine Hydrochloride Tablets (C-II) |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions August 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about methamphetamine
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (78)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: anorexiants
- Breastfeeding
- En español