Exemestane (Monograph)
Brand name: Aromasin
Drug class: Antiestrogens
- Aromatase Inhibitors
Introduction
Antineoplastic agent; irreversible, selective steroidal aromatase inhibitor (type I), structurally related to the natural substrate androstenedione.
Uses for Exemestane
Initial, Sequential, or Extended Adjuvant Therapy for Postmenopausal Women with Early-Stage Hormone Receptor-Positive Breast Cancer
Sequential adjuvant therapy in postmenopausal women with early-stage estrogen receptor-positive breast cancer who have received 2–3 years of adjuvant tamoxifen and are switched to exemestane to complete a total of 5 consecutive years of adjuvant hormonal therapy.
Guidelines from ASCO state that postmenopausal women with node-positive hormone-receptor positive breast cancer should be offered extended adjuvant endocrine therapy with one of the following: aromatase inhibitor therapy for up to a total of 10 years; tamoxifen for 10 years; tamoxifen for 5 years, then an aromatase inhibitor for 5 years; or tamoxifen for 2–3 years, then an aromatase inhibitor for 7–8 years. Women with node-negative breast cancer may also be offered extended adjuvant endocrine therapy for up to a total of 10 years, although benefits are likely narrower due to the lower risk for recurrence.
Consider adverse effects, patient preference, and preexisting conditions when selecting an adjuvant regimen; during the course of adjuvant therapy, patients who are intolerant of one treatment may be switched to a different treatment.
Advanced Breast Cancer in Postmenopausal Women
Treatment of advanced breast cancer in postmenopausal women with progressive disease after tamoxifen therapy.
Adjuvant Therapy for Early-Stage Breast Cancer in Premenopausal Women
Use of endocrine therapy (i.e., anastrozole, exemestane, letrozole, tamoxifen) in combination with ovarian suppression† [off-label] as adjuvant therapy in premenopausal women† [off-label] with early-stage hormone receptor-positive breast cancer may be considered a reasonable choice (accepted).
Reduction in the Incidence of Breast Cancer in Women at High Risk
Exemestane has been used for the reduction in the incidence of breast cancer among women who are at high risk of developing the disease† [off-label].
Exemestane Dosage and Administration
General
Pretreatment Screening
-
Assess baseline 25-hydroxyvitamin D levels prior to treatment.
-
Assess bone mineral density at baseline in patients with osteoporosis or at risk for osteoporosis.
-
Pregnancy testing for females of reproductive potential is recommended within 7 days prior to starting exemestane.
Patient Monitoring
-
Monitor patients for bone mineral density loss, particularly those with osteoporosis or at risk for osteoporosis.
Administration
Oral Administration
Exemestane is administered orally once daily after a meal.
Dosage
Adults
Breast Cancer
Sequential Adjuvant Therapy for Postmenopausal Women with Early-stage Hormone Receptor-Positive Breast Cancer
Oral25 mg once daily. Initiate following completion of 2–3 years of adjuvant tamoxifen therapy to complete a total of 5 consecutive years of adjuvant hormonal therapy.
Advanced Breast Cancer in Postmenopausal Women
Oral25 mg once daily.
Initial Adjuvant Therapy for Postmenopausal Women with Early-Stage Hormone Receptor-Positive Breast Cancer† [off-label]
Oral25 mg once daily for up to 10 years† [off-label].
Extended Adjuvant Therapy for Postmenopausal Women with Early-Stage Hormone Receptor-Positive Breast Cancer†
Oral25 mg once daily for up to 10 years†.
Adjuvant Therapy for Early-Stage Breast Cancer in Premenopausal Women in Combination with Ovarian Suppression†
Oral25 mg once daily for 5 years has been used in combination with ovarian suppression†.
Reduction in the Incidence of Breast Cancer in Women at High Risk
Oral25 mg once daily has been used†.
Dosage Modification for Concomitant Use with Drugs that Induce CYP3A4
Strong CYP3A4 inducers may decrease exemestane exposure. The recommended dosage of exemestane when given concurrently with strong CYP3A4 inducers (e.g., rifampin [rifampicin] or phenytoin) is 50 mg once daily after a meal.
Special Populations
Renal Impairment
Dosage adjustment does not appear to be necessary.
Hepatic Impairment
Dosage adjustment does not appear to be necessary.
Geriatric Patients
The manufacturer makes no recommendations for dosage adjustments based on age.
Cautions for Exemestane
Contraindications
-
Known hypersensitivity to exemestane or any ingredient in the formulation.
Warnings/Precautions
Reductions in Bone Mineral Density
Postmenopausal women receiving an aromatase inhibitor as adjuvant therapy are at high risk for osteoporosis.
Greater reductions in bone mineral density (BMD) at lumbar spine and hip observed over 2 years in patients receiving exemestane (3.1 and 4.2%, respectively) versus tamoxifen (0.2 and 0.3%, respectively). Another study showed greater reductions in lumbar spine and hip BMD over 2 years in patients receiving exemestane (3.5 and 4.6%, respectively) versus placebo (2.4 and 2.6%, respectively).
Incidence of fractures higher in patients switched to exemestane after receiving 2–3 years of adjuvant tamoxifen than in those continuing tamoxifen to complete 5 years of adjuvant therapy.
Assess bone density by bone densitometry at the commencement of exemestane treatment in women with osteoporosis or at risk of osteoporosis. Monitor patients for BMD loss and treat as appropriate.
Vitamin D Assessment
Assess vitamin D (25-hydroxyvitamin D) levels prior to beginning therapy with an aromatase inhibitor due to the high prevalence of vitamin D deficiency among women with breast cancer. Supplementation with vitamin D may be necessary.
Administration with Estrogen-containing Agents.
Do not administer estrogen-containing agents concomitantly with exemestane. (See Specific Drugs under Interactions.)
Laboratory Abnormalities
Grade 3 or 4 lymphocytopenia reported in 20% of exemestane-treated patients with advanced breast cancer. Most patients (89%) had preexisting lower-grade lymphocytopenia; 40% recovered or improved during exemestane therapy. No substantial increase in viral infections and no opportunistic infections observed in clinical studies.
In early-stage breast cancer, hematologic abnormalities reported less frequently with exemestane than with tamoxifen treatment; grade 3 or 4 abnormalities reported rarely.
In advanced breast cancer, serum AST, ALT, alkaline phosphatase, and γ-glutamyltransferase (γ-glutamyltranspeptidase, GGT, GGTP) concentrations >5 times the ULN (i.e., grade 3 or worse) reported rarely in patients receiving exemestane; generally attributable to bone or liver metastasis. In patients without evidence of liver metastasis, grade 3–4 GGT elevations reported at similar rates in exemestane- or megestrol-treated patients.
In early-stage breast cancer, elevated bilirubin and alkaline phosphatase concentrations reported more frequently with exemestane than with tamoxifen or placebo treatment. Grade 3–4 bilirubin elevations reported rarely.
Elevated Scr reported.
Use in Premenopausal Women
Manufacturer states exemestane is not indicated for treatment of breast cancer in premenopausal women. Possible incomplete estrogen suppression and reflex increases in gonadotropin levels (ovarian hyperstimulation syndrome).
Has been used in combination with ovarian suppression as adjuvant therapy in premenopausal women† with early-stage hormone receptor-positive breast cancer.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm; embryotoxic, fetotoxic, and abortifacient in animals. Test for pregnancy status within 7 days prior to initiation of the drug. Advise females of reproductive potential to use effective contraceptive methods during therapy and for 1 month after discontinuance of the drug. If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard and potential risk for pregnancy loss.
Specific Populations
Pregnancy
May cause fetal harm. No adequate and well-controlled studies in pregnant women. If exemestane is used during pregnancy or if the patient becomes pregnant while receiving the drug, inform the patient of the potential hazard to the fetus and the potential risk for pregnancy loss.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Effects on nursing infant and milk production also unknown. Discontinue nursing during therapy and for ≥1 month after drug discontinuance.
Females and Males of Reproductive Potential.
Manufacturer recommends testing for pregnancy status within 7 days prior to initiation of exemestane. Advise females of reproductive potential to use an effective method of contraception while taking exemestane and for 1 month after the last dose of treatment.
May impair female and male fertility.
Pediatric Use
Not indicated; safety and efficacy not established.
Geriatric Use
No special precautions.
Hepatic Impairment
Systemic exposure increased in patients with moderate or severe hepatic impairment; however, dosage adjustment does not appear to be necessary.
Renal Impairment
Systemic exposure increased in patients with moderate or severe renal impairment; however, dosage adjustment does not appear to be necessary.
Common Adverse Effects
Adverse events reported in ≥10% of patients with early-stage breast cancer receiving exemestane include hot flushes (flashes), fatigue, arthralgia, headache, insomnia, and increased sweating.
Adverse events reported in ≥5% of patients with advanced breast cancer receiving exemestane include fatigue, nausea, and hot flushes. Most adverse events were mild to moderate in severity.
Drug Interactions
Metabolized by CYP3A4. Does not inhibit CYP1A2, 2C9, 2D6, 2E1, or 3A4.
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 inhibitors: Clinically important pharmacokinetic interactions are unlikely.
CYP3A4 inducers: Possible decreased exposure to exemestane. If a potent CYP3A4 inducer is used concomitantly, increase exemestane dosage to 50 mg once daily.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Anticonvulsants (carbamazepine, phenobarbital, phenytoin) |
Possible decreased exposure to exemestane |
Increase exemestane dosage to 50 mg once daily after a meal |
|
Estrogen-containing agents |
May diminish pharmacologic action of exemestane |
Do not use concomitantly |
|
Ketoconazole |
No substantial effect on pharmacokinetics of exemestane |
|
|
Rifampin |
Decreased AUC and peak plasma concentrations of exemestane |
Increase exemestane dosage to 50 mg once daily after a meal |
|
St. John's wort (Hypericum perforatum) |
Possible decreased exposure to exemestane |
Increase exemestane dosage to 50 mg once daily after a meal |
Exemestane Pharmacokinetics
Absorption
Bioavailability
Rapidly absorbed following oral administration; peak concentrations in women with breast cancer or healthy women attained within about 1.2 or 2.9 hours, respectively. Approximately 42% of an oral dose is absorbed from the GI tract.
Following repeated doses, mean AUC in women with breast cancer is approximately twice that in healthy women.
Food
High-fat meal increases AUC and peak plasma exemestane concentrations by 59 and 39%, respectively.
Special Populations
Age (43–68 years) and sex do not affect pharmacokinetics.
Distribution
Extent
Extensively distributed into tissues.
Crosses placenta.
Distributed into milk in animals; not studied in pregnant or nursing women.
Plasma Protein Binding
90% (mainly α1-acid glycoprotein and albumin).
Elimination
Metabolism
Extensively metabolized via CYP3A4 and aldoketoreductases; metabolites are inactive or inhibit aromatase with decreased potency compared with parent drug. One metabolite, 17-hydroexemestane, may have androgenic activity.
Elimination Route
Excreted similarly (42%) in both urine and feces; <1% excreted as unchanged drug in urine.
Half-life
Approximately 24 hours.
Special Populations
In patients with moderate or severe hepatic (Child-Pugh class B or C) or renal (Clcr <35 mL/minute per 1.73 m2) impairment, AUC is approximately 3 times higher than in healthy individuals.
Stability
Storage
Oral
Tablets
Store at 25°C (excursions permitted between 15–30°C).
Actions
-
Acts as a false substrate and is converted by aromatase to reactive alkylating intermediates that bind covalently to the substrate binding site of the enzyme; this irreversible binding to the active site of aromatase results in its inactivation (i.e., “suicide” inhibition).
-
Selectively inhibits conversion of androgens to estrogens; resulting reduction in serum and tumor concentrations of estrogen inhibits tumor growth and delays disease progression.
-
Selectively inhibits synthesis of estrogens; does not affect synthesis of adrenal corticosteroid, aldosterone, or thyroid hormone.
-
Dose-dependent decrease in sex hormone binding globulin (SHBG) observed with dosages ≥2.5 mg daily.
-
Slight, dose-independent increases in serum LH and FSH concentrations observed even at low dosages as result of negative feedback on the pituitary gland.
-
At dosages ≤25 mg daily, no clinically important effect on circulating concentrations of androstenedione, dehydroepiandrostenedione sulfate, or 17-hydroxyprogesterone and only small decreases in circulating concentrations of testosterone observed.
-
At dosages ≥200 mg daily, testosterone and androstenedione concentrations are increased. 17-Hydroexemestane, a metabolite, exhibits substantial intrinsic androgenic activity, which may become clinically important at high (e.g., 200 mg daily) dosages.
Advice to Patients
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and herbal supplements, as well as any concomitant illnesses.
-
Importance of not taking estrogen-containing agents concomitantly with exemestane.
-
Risk of osteoporosis. Monitor bone mineral density (BMD).
-
Risk of fetal harm and pregnancy loss. Advise females of reproductive potential to use effective contraception during exemestane therapy and for 1 month after the last dose of the drug.
-
Patients also should be advised that exemestane is FDA-labeled for use only in postmenopausal women.
-
Advise women to avoid breast-feeding while receiving exemestane and for 1 month following discontinuance of therapy.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
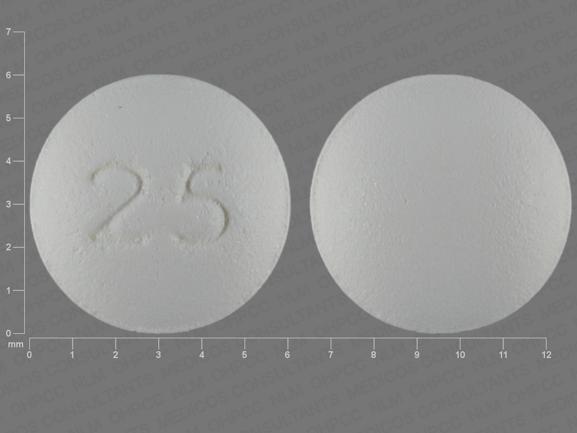
Oral |
Tablets |
25 mg* |
Aromasin |
Pfizer |
|
Exemestane Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 22, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
- Which is better - Aromasin or Femara?
- Aromasin vs Femara - how do they compare?
- How long do you need to take Aromasin?
- Should you take Aromasin with food?
More about exemestane
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (120)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: aromatase inhibitors
- Breastfeeding
- En español