Dabigatran (Monograph)
Brand name: Pradaxa
Drug class: Direct Thrombin Inhibitors
Chemical name: N-[[2-[[[4-(Aminoiminomethyl)phenyl]amino]methyl]-1-methyl-1H-benzimidazol-5-yl]carbonyl]-N-2-pyridinyl-β-alanine
Molecular formula: C25H25N7O3C34H41N7O5C34H41N7O5•CH4O3S
CAS number: 211914-51-1
Warning
- Risk of Thrombosis Following Premature Discontinuance of Anticoagulation
-
Premature discontinuance of any oral anticoagulant, including dabigatran, increases risk of thrombotic events.
-
If discontinuance is required for reasons other than pathologic bleeding or completion of a course of therapy, consider coverage with an alternative anticoagulant.
- Spinal/Epidural Hematoma
-
Risk of epidural or spinal hematomas and neurologic injury, including long-term or permanent paralysis, in patients who are anticoagulated and also receiving neuraxial (spinal/epidural) anesthesia or spinal puncture.
-
Risk increased by use of indwelling epidural catheters or by concomitant use of drugs affecting hemostasis (e.g., NSAIAs, platelet-aggregation inhibitors, other anticoagulants).
-
Risk also increased by spinal deformity, spinal surgery, or history of traumatic or repeated epidural or spinal puncture.
-
Monitor frequently for signs and symptoms of neurologic impairment and treat urgently if neurologic compromise noted.
-
Consider potential benefits versus risks of spinal or epidural anesthesia or spinal puncture in patients receiving or being considered for anticoagulant therapy.
Introduction
Anticoagulant; a synthetic reversible direct thrombin inhibitor.
Uses for Dabigatran
Embolism Associated with Atrial Fibrillation
Reduction in risk of stroke and systemic embolism in adult patients with nonvalvular atrial fibrillation.
Direct oral anticoagulants (DOACs; apixaban, dabigatran, edoxaban, rivaroxaban) are noninferior or superior to warfarin in reducing thromboembolic risk in patients with nonvalvular atrial fibrillation and associated with reduced risk of serious bleeding.
The American College of Chest Physicians (ACCP), American Stroke Association (ASA), American College of Cardiology (ACC), American Heart Association (AHA), and other experts recommend antithrombotic therapy in all patients with nonvalvular atrial fibrillation who are considered to be at increased risk of stroke, unless contraindicated.
Current guidelines recommend use of the CHA2DS2-VASc risk stratification tool to assess a patient’s risk of stroke and need for anticoagulant therapy.
Experts state that antithrombotic therapy generally is not necessary in low-risk patients (CHA2DS2-VASc score of 0 in males or 1 in females), but should be considered in all higher-risk patients.
In patients with nonvalvular atrial fibrillation who are eligible for oral anticoagulant therapy, DOACs are recommended over warfarin based on improved safety and similar or improved efficacy.
Relative efficacy and safety of dabigatran and other DOACs (e.g., apixaban, rivaroxaban, edoxaban) remains to be fully elucidated.
When selecting an appropriate anticoagulant, consider factors such as the absolute and relative risks of stroke and bleeding; costs; patient compliance, preference, tolerance, and comorbidities; and other clinical factors such as renal function and degree of INR control (if the patient has been taking warfarin).
Experts state antithrombotic therapy in patients with atrial flutter generally should be managed in the same manner as in patients with atrial fibrillation.
DOACs including dabigatran have been used for pharmacologic cardioversion† [off-label] in patients with atrial fibrillation or atrial flutter of >48 hours’ duration or of unknown duration; DOACs are recommended as an alternative to warfarin in this setting.
Contraindicated in patients with prosthetic mechanical heart valves; increased risk of serious thromboembolic and bleeding events observed in such patients receiving dabigatran compared with warfarin therapy.
Not generally recommended in patients with other forms of valvular heart disease, including those with bioprosthetic heart valves.
Venous Thromboembolism – Treatment and Secondary Prevention
Treatment of acute DVT and/or PE in adults following initial treatment with a parenteral anticoagulant for 5–10 days. Also used to reduce the risk of recurrent DVT and PE in adults treated previously for an acute venous thromboembolic event (VTE).
Treatment of VTE in pediatric patients 3 months to <18 years of age after at least 5 days of initial parenteral anticoagulant treatment and to reduce the risk of recurrent VTE in such patients who have been previously treated.
FDA indication for pediatric patients is product-specific. Dabigatran capsules are indicated for children ≥8 years of age. Dabigatran pellets are indicated for children 3 months to <12 years of age.
DOACs are among several anticoagulants that can be used for treatment of VTE. DOACs have similar efficacy to warfarin, but reduced bleeding (particularly intracranial hemorrhage) and greater convenience for patients and healthcare providers.
DOACs generally should not be used in settings with increased risk of bleeding, morbid obesity (body weight >120 kg or BMI >40 mg/m2), drug-drug interactions, or GI complications affecting oral therapy (e.g., poor absorption, nausea and vomiting) because of lack of safety data.
In patients with cancer and established VTE, low molecular weight heparins (LMWHs) or oral factor Xa inhibitors (e.g., apixaban, rivaroxaban, edoxaban) are generally recommended over warfarin for long-term anticoagulation. ACCP and ASH recommend the use of an oral factor Xa inhibitor over LMWH for the initiation and treatment phases of therapy in patients with cancer-associated thrombosis.
Thromboprophylaxis in Major Orthopedic Surgery
Prevention of postoperative DVT and PE in adults undergoing hip-replacement surgery.
Shown to be as effective as enoxaparin in reducing risk of VTE in patients undergoing elective total hip-replacement surgery with similar rates of bleeding.
Also has been used for VTE prevention in patients undergoing total knee-replacement surgery† [off-label].
ACCP and other clinicians consider DOACs an acceptable option for pharmacologic thromboprophylaxis in patients undergoing total hip- or knee-replacement surgery.
Drug selection and duration of therapy should be individualized based on type of surgery, patient risk factors for embolism and bleeding, costs, patient compliance, preference, tolerance, and comorbidities, and other clinical factors such as renal function.
Dabigatran Dosage and Administration
General
Pretreatment Screening
-
Prior to initiating therapy with dabigatran, assess renal function in all patients. In children, estimate the glomerular filtration rate (eGFR) using the Schwarz formula as follows: eGFR = (0.413 × height in cm)/serum creatinine in mg/dL. Avoid use of dabigatran in pediatric patients with an eGFR <50 mL/minute per 1.73 m2.
-
When used in pediatric patients for treatment and secondary prevention of venous thromboembolism (VTE), obtain body weight for dosing.
Patient Monitoring
-
Periodically assess renal function as clinically indicated (i.e., more frequently in situations that may be associated with a decline in renal function) and adjust therapy accordingly.
-
When used in pediatric patients for treatment and secondary prevention of VTE, periodically assess body weight and adjust doses and dosage forms accordingly.
-
If dabigatran is administered in an epidural or spinal anesthesia/analgesia or lumbar puncture setting, frequently monitor for signs or symptoms of neurological impairment (e.g., numbness, tingling, weakness in lower limbs, bowel and/or bladder dysfunction).
-
Monitor patients for any signs or symptoms of bleeding (e.g., unusual bruising) during therapy.
-
Routine monitoring of coagulation status is not required in patients receiving dabigatran. When necessary, the manufacturer states that the ecarin clotting time (ECT) or the activated partial thromboplastin time (aPTT) may be used to assess the anticoagulant effects of dabigatran; however, results of such tests should be interpreted with caution. Use of the prothrombin time (PT)/international normalized ratio (INR) should be avoided since this test is relatively insensitive to the effects of dabigatran and results may be unreliable.
Dispensing and Administration Precautions
-
Dabigatran is available in different dosage forms and not all forms are approved for the same indications and age groups. Dabigatran dosage forms are not interchangeable due to bioavailability differences. Avoid substituting different dosage forms on a mg-to-mg basis and do not combine more than one dosage form to achieve the total dose.
-
Based on the Institute for Safe Medication Practices (ISMP), dabigatran is a high-alert medication that has a heightened risk of causing significant patient harm when used in error.
Administration
Oral Administration
Administer orally (as capsules or oral pellets).
Dosage forms are not interchangeable.
Capsules
Administer orally twice daily without regard to meals. Consider administration with food, if GI distress occurs.
Capsules may be used in pediatric patients ≥8 years of age who are able to swallow capsules whole. Administer one dose in the morning and one in the evening, 12 hours apart.
Do not remove capsules from bottle or blister package until time of use.
Swallow capsules whole with full glass of water; do not chew, break, or empty the contents of the capsule.
Take a missed dose as soon as it is remembered on the same day. If a missed dose cannot be taken at least 6 hours before next scheduled dose, skip the dose; do not double doses.
Pellets
May use oral pellets in children 3 months to <12 years of age as soon as they are able to swallow soft foods.
Administer one dose in the morning and one in the evening, 12 hours apart. Administer oral pellets twice daily before a meal to ensure that the child takes the full dose.
Swallow pellets without chewing after mixing with 2 teaspoons of a soft food at room temperature (e.g., baby rice cereal prepared with water, mashed carrots, apple sauce, or mashed banana); alternatively mix with 1–2 ounces of apple juice for drinking. Do not use milk, milk products, or soft foods containing milk to prepare the dose.
Administer immediately after mixing or within 30 minutes.
Do not administer via syringe or feeding tubes.
Discard any dose not administered within 30 minutes and prepare a new dose as necessary.
Do not administer a second dose if a partial dose has been taken. Administer the next dose as scheduled approximately 12 hours later.
Administer a missed dose as soon as it is remembered on same day; do not administer missed dose if it cannot be taken at least 6 hours before next scheduled dose. Do not give a double dose.
Do not remove packet from aluminum bag until time of use.
Dosage
Available as dabigatran etexilate mesylate; dosage expressed in terms of the prodrug, dabigatran etexilate.
Pediatric Patients
Venous Thromboembolism – Treatment and Secondary Prevention
Oral
Pediatric patients 3 months to <12 years of age with eGFR (Schwartz) >50 mL/minute per 1.73 m2: Table 1 provides dosing recommendations for the oral pellets in patients <2 years of age and Table 2 provides recommendations for the oral pellets in patients 2 to <12 years of age.
|
Actual body weight |
Age |
Dose given twice daily |
Number of packets needed |
|---|---|---|---|
|
3 kg to <4 kg |
3 to <6 months |
30 mg |
One 30 mg packet twice daily |
|
4 kg to <5 kg |
3 to <10 months |
40 mg |
One 40 mg packet twice daily |
|
5 kg to <7 kg |
3 to <5 months |
40 mg |
One 40 mg packet twice daily |
|
5 to <24 months |
50 mg |
One 50 mg packet twice daily |
|
|
7 kg to <9 kg |
3 to <4 months |
50 mg |
One 50 mg packet twice daily |
|
4 to <9 months |
60 mg |
Two 30 mg packets twice daily |
|
|
9 to <24 months |
70 mg |
One 30 mg plus one 40 mg packet twice daily |
|
|
9 kg to <11 kg |
5 to <6 months |
60 mg |
Two 30 mg packets twice daily |
|
6 to <11 months |
80 mg |
Two 40 mg packets twice daily |
|
|
11 to <24 months |
90 mg |
One 40 mg plus one 50 mg packet twice daily |
|
|
11 kg <13 kg |
8 to <18 months |
100 mg |
Two 50 mg packets twice daily |
|
18 to <24 months |
110 mg |
One 110 mg packet twice daily |
|
|
13 kg to <16 kg |
10 to <11 months |
100 mg |
Two 50 mg packets twice daily |
|
11 to <24 months |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
|
16 kg to <21 kg |
12 to <24 months |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
21 kg to <26 kg |
18 to <24 months |
180 mg |
One 30 mg plus one 150 mg packet twice daily |
|
Actual body weight |
Dose given twice daily |
Number of packets needed |
|---|---|---|
|
7 kg to <9 kg |
70 mg |
One 30 mg plus one 40 mg packet twice daily |
|
9 kg to <11 kg |
90 mg |
One 40 mg plus one 50 mg packet twice daily |
|
11 kg to <13 kg |
110 mg |
One 110 mg packet twice daily |
|
13 kg to <16 kg |
140 mg |
One 30 mg plus one 110 mg packet twice daily |
|
16 kg to <21 kg |
170 mg |
One 20 mg plus one 150 mg packet twice daily |
|
21 kg to <41 kg |
220 mg |
Two 110 mg packets twice daily |
|
≥41 kg |
260 mg |
One 110 mg plus one 150 mg packet twice daily |
Pediatric patients 8 to <18 years of age with eGFR (Schwartz) >50 mL/minute per 1.73 m2:Table 3 provides dosage recommendations for the capsules in patients 8 to <18 years of age.
|
Actual body weight |
Dose given twice daily |
Number of capsules needed |
|---|---|---|
|
11 kg to <16 kg |
75 mg twice daily |
One 75 mg capsule twice daily |
|
16 kg to <26 kg |
110 mg twice daily |
One 110 mg capsule twice daily |
|
26 kg to <41 kg |
150 mg twice daily |
One 150 mg capsule twice daily |
|
Or |
||
|
Two 75 mg capsules twice daily |
||
|
41 kg to <61 kg |
185 mg twice daily |
One 110 mg plus one 75 mg capsule twice daily |
|
61 kg to <81 kg |
220 mg twice daily |
Two 110 mg capsules twice daily |
|
≥81 kg |
260 mg twice daily |
One 150 mg plus one 110 mg capsule twice daily |
|
Or |
||
|
One 110 mg plus two 75 mg capsules twice daily |
Adults
Embolism Associated with Atrial Fibrillation
Oral
Patients with Clcr >30 mL/minute: 150 mg twice daily.
Venous Thromboembolism - Treatment and Secondary Prevention
Oral
Patients with Clcr >30 mL/minute: 150 mg twice daily following 5–10 days of therapy with a parenteral anticoagulant.
Determine optimum duration of anticoagulation based on individual clinical situation (e.g., location of thrombi, presence or absence of precipitating factors for thrombosis, presence of cancer, risk of bleeding). In general, ACCP states that anticoagulant therapy should be continued beyond the acute treatment period for ≥3 months, and possibly longer in certain patients with a high risk of recurrence and low or moderate risk of bleeding.
Thromboprophylaxis in Hip Replacement Surgery
Oral
Patients with Clcr >30 mL/minute: Single dose of 110 mg administered 1–4 hours after surgery, provided hemostasis has been achieved, followed by 220 mg once daily. If dabigatran therapy not initiated on day of surgery, initiate therapy with 220 mg once daily when hemostasis established.
Manufacturer recommends treatment duration of 28–35 days. ACCP recommends at least 10–14 days, possibly up to 35 days, for patients undergoing major orthopedic surgery.
Transitioning from Other Anticoagulant Therapy
Transitioning from warfarin to dabigatran: Discontinue warfarin and initiate dabigatran when INR is <2.
Transitioning from LMWH to dabigatran: Discontinue LMWH and initiate dabigatran within 2 hours prior to what would have been the time of the next scheduled LMWH dose.
Transitioning from heparin IV infusion to dabigatran: Discontinue heparin infusion and initiate dabigatran at the time of discontinuance.
Transitioning to Other Anticoagulant Therapy
Pediatric Patients
Transitioning from dabigatran to warfarin: in patients with eGFR (Schwartz) ≥50 mL/minute per 1.73 m2, begin warfarin 3 days before discontinuing dabigatran. Dabigatran may affect INR; INR for monitoring warfarin is more reliable ≥2 days after dabigatran discontinuance.
Transitioning from dabigatran to parenteral anticoagulant: discontinue dabigatran and begin parenteral anticoagulant 12 hours after the last dose of dabigatran.
Adults
Transitioning from dabigatran to warfarin:
Initiate warfarin before discontinuing dabigatran. Dabigatran may affect INR; INR for monitoring warfarin is more reliable ≥2 days after dabigatran discontinuance.
Clcr ≥50 mL/minute: begin warfarin 3 days before discontinuing dabigatran.
Clcr 30–50 mL/minute: begin warfarin 2 days before discontinuing dabigatran.
Clcr 15–30 mL/minute: begin warfarin 1 day before discontinuing dabigatran.
Clcr <15 mL/minute: recommendations not available.
Transitioning from dabigatran to parenteral anticoagulant:
Clcr ≥30 mL/minute: discontinue dabigatran and begin parenteral anticoagulant 12 hours after the last dose of dabigatran.
Clcr <30 mL/minute: discontinue dabigatran and begin parenteral anticoagulant 24 hours after the last dose of dabigatran.
Managing Anticoagulation in Patients Requiring Invasive Procedures
Withhold dabigatran prior to surgery or other invasive procedures if possible. If surgery cannot be delayed, weigh increased risk of bleeding against urgency of intervention.
Consider withholding drug for longer periods in patients who may require complete hemostasis (e.g., prior to major surgery, spinal puncture, placement of spinal or epidural catheter or port).
Consider resumption of anticoagulant therapy as soon as medically appropriate.
Pediatric Patients
Patients with eGFR (Schwartz) >80 mL/minute per 1.73 m2: withhold dabigatran beginning 24 hours prior to procedure.
Patients with eGFR (Schwartz) 50-80 mL/minute per 1.73 m2: withhold dabigatran beginning 48 hours prior to procedure.
Idarucizumab efficacy and safety in pediatric patients not established.
Adults
Clcr ≥50 mL/minute: withhold dabigatran beginning 1–2 days prior to procedure.
Clcr <50 mL/minute: withhold dabigatran beginning 3–5 days prior to procedure.
Idarucizumab can be used in case of emergency surgery or urgent procedures when reversal of the anticoagulant effect of dabigatran is needed. Dabigatran therapy can be reinitiated 24 hours after administration of idarucizumab; consider reinitiation of dabigatran as soon as medically appropriate.
Special Populations
Hepatic Impairment
Manufacturer makes no specific dosage recommendations.
Renal Impairment
Embolism Associated with Atrial Fibrillation
Reduce dosage to 75 mg orally twice daily in adults with severe renal impairment (Clcr 15–30 mL/minute). For patients with a creatinine clearance <15 mL/minute or who are receiving hemodialysis, dosage recommendations cannot be provided.
In adults with Clcr 30–50 mL/minute and receiving concomitant therapy with the P-gp inhibitors dronedarone or systemic ketoconazole, reduce dosage to 75 mg twice daily. Avoid such concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute). Avoid concomitant use of P-gp inhibitors in patients with Clcr <30 mL/minute.
Venous Thromboembolism - Treatment and Secondary Prevention
Pediatric Patients: Avoid use in children with eGFR (Schwartz) <50 mL/minute per 1.73 m2 due to risk of increased drug exposure. Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.
Adults: Manufacturer states that dosage recommendations cannot be provided for patients with Clcr ≤30 mL/minute or for those receiving dialysis. Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.
Avoid concomitant use of P-gp inhibitors in patients with Clcr <50 mL/minute.
Thromboprophylaxis in Hip-Replacement Surgery
Dosage recommendations cannot be provided for adult patients with Clcr ≤30 mL/minute or for those receiving dialysis. Discontinue in patients who develop acute renal failure while on therapy; consider an alternative anticoagulant.
Avoid concomitant use of P-gp inhibitors in patients with Clcr <50 mL/minute.
Geriatric Patients
Manufacturer makes no specific dosage recommendations.
Cautions for Dabigatran
Contraindications
-
Active pathologic bleeding.
-
History of serious hypersensitivity reaction.
-
Mechanical prosthetic heart valve.
Warnings/Precautions
Warnings
Risk of Thrombosis Following Premature Discontinuance of Anticoagulation
Premature discontinuance in the absence of adequate alternative anticoagulation may increase risk of thromboembolic events. (See Boxed Warning.)
When transitioning patients from one anticoagulant therapy to another, ensure continuous anticoagulation while minimizing risk of bleeding.
Particular caution advised when switching from a DOAC to warfarin therapy because of warfarin's slow onset of action.
If discontinuance of dabigatran required for reasons other than pathologic bleeding or completion of a course of therapy, consider coverage with an alternative anticoagulant.
Advise patients regarding importance of adhering to therapeutic regimen and on steps to take if doses are missed.
Spinal/Epidural Hematoma
Epidural or spinal hematoma reported with concurrent use of anticoagulants and neuraxial (spinal/epidural) anesthesia or spinal puncture procedures. Such hematomas have resulted in neurologic injury, including long-term or permanent paralysis. (See Boxed Warning.)
To reduce risk of bleeding with concurrent use of dabigatran and neuraxial anesthesia or spinal puncture, carefully consider pharmacokinetic (PK) profile of dabigatran in relation to timing of such procedures.
Frequently monitor for signs and symptoms of neurologic impairment (e.g., midline back pain, numbness/tingling or weakness in lower limbs, bowel or bladder dysfunction). If neurologic compromise noted, diagnose and treat immediately; consider spinal cord decompression.
Carefully consider potential benefits versus risks of neuraxial intervention in patients who are currently receiving or will receive anticoagulants.
Other Warnings and Precautions
Bleeding
Risk of serious, potentially fatal, bleeding. Promptly evaluate if any manifestations of blood loss occur during therapy.
Discontinue if active pathologic bleeding occurs. However, should not readily discontinue anticoagulation for commonly occurring minor or “nuisance” bleeding.
Risk of bleeding may be increased in patients with renal impairment or those receiving concomitant drugs that affect hemostasis (e.g., antiplatelet agents, heparin, thrombolytic therapy, chronic use of NSAIAs). Overdosage also may lead to hemorrhagic complications.
Temporarily interrupt therapy prior to any elective surgery or other invasive procedure to reduce risk of bleeding. If serious bleeding occurs, discontinue dabigatran and initiate appropriate treatment.
Idarucizumab is a specific reversal agent for dabigatran that is used in adults for life-threatening or uncontrolled bleeding or in patients who require emergency surgery/urgent procedures. Idarucizumab can be used in conjunction with supportive measures (e.g., maintenance of adequate diuresis, mechanical compression, surgical hemostasis, volume replacement, blood products), which should be considered as medically appropriate.
Idarucizumab efficacy and safety in pediatric patients not established.
Dabigatran can be dialyzed; however, results will likely vary depending on individual patient-specific characteristics.
Consider use of procoagulant reversal agents such as anti-inhibitor coagulant complex (also known as activated prothrombin complex concentrate) or recombinant factor VIIa for immediate reversal of anticoagulation if idarucizumab not available.
Protamine sulfate and vitamin K not expected to be effective. Consider use of platelet concentrates in case of thrombocytopenia or if long-acting antiplatelet drugs have been used.
If overdosage occurs, may consider early (e.g., within 1–2 hours) use of activated charcoal.
Patients with Prosthetic Heart Valves
Contraindicated in patients with mechanical prosthetic heart valves.
Increased risk of thromboembolic events (valve thrombosis, stroke, TIA, MI) and major bleeding (mainly postoperative pericardial effusions) with dabigatran compared with warfarin therapy.
Not generally recommended in patients with other forms of valvular heart disease, including those with bioprosthetic heart valves.
Drugs Affecting P-glycoprotein Transport
Avoid concurrent dabigatran with P-glycoprotein transport inducers (e.g., rifampin) due to reduced exposure to dabigatran.
P-glycoprotein transport inhibitors (e.g., dronedarone, systemic ketoconazole) may increase systemic exposure to dabigatran in patients with renal impairment; dosage reduction or avoidance of such concomitant therapy may be necessary.
Thrombosis Risk in Triple Positive Antiphospholipid Syndrome
Risk of recurrent thrombotic events in patients with triple-positive antiphospholipid syndrome (APS) (i.e., positive for lupus anticoagulant, anticardiolipin, and anti-beta 2-glycoprotein I antibodies); use not recommended in these patients.
Specific Populations
Pregnancy
No adequate data in pregnant women; increased maternal bleeding observed in animals.
Use during labor and delivery in women receiving neuraxial anesthesia may result in epidural or spinal hematomas. Consider use of a shorter-acting anticoagulant as delivery approaches. Monitor for increased bleeding in the neonate.
Lactation
Distributed into milk in rats; not known whether distributed into human milk.
Females and Males of Reproductive Potential
Assess for increased risk of bleeding potentially requiring surgical intervention in females of reproductive potential and those with abnormal uterine bleeding.
Pediatric Use
Safety and efficacy of dabigatran for VTE treatment and reduction in risk of recurrent VTE have been established in pediatric patients <12 years of age (oral pellets) and pediatric patients 8 to <18 years of age (oral capsules).
Safety and efficacy not established in pediatric patients for other indications.
Geriatric Use
Risk of stroke and bleeding increases with age, but risk-benefit profile is favorable in all age groups.
Hepatic Impairment
Large interpatient variability , but no consistent change in exposure or pharmacodynamic (PD) response observed in adults with moderate hepatic impairment (Child-Pugh class B). Pediatric patients with active liver disease were excluded from the DIVERSITY trial.
Renal Impairment
Primarily eliminated renally. Exposure (AUC), half-life, and anticoagulant effects are increased in patients with renal impairment. Evaluate renal function prior to initiating therapy and periodically thereafter when clinically indicated.
Dosage adjustments in adults may be necessary depending on degree of renal impairment and indication for use.
Not evaluated in pediatric patients with eGFR <50 mL/minute per 1.73 m2; avoid use in these patients.
Hemodialysis can remove dabigatran.
Common Adverse Effects
Adverse effects (>15%): GI adverse reactions, bleeding.
Drug Interactions
Does not inhibit or induce, and is not a substrate for, CYP isoenzymes.
Substrate for the P-glycoprotein (P-gp) transport system.
No clinical drug interaction studies have been conducted in pediatric subjects.
Drugs Affecting or Metabolized by Hepatic Microsomal Enzymes
Pharmacokinetic interactions with drugs metabolized by CYP isoenzymes unlikely.
Drugs Affecting P-glycoprotein Transport
P-gp inducers: Potential PK interaction (reduced dabigatran exposure); avoid concomitant use.
P-gp inhibitors: Potential PK interaction (increased dabigatran exposure). In patients with atrial fibrillation, the Anticoagulation Forum recommends avoiding use of dabigatran in patients with Clcr <30 mL/minute who are taking P-gp inhibitors. In the VTE setting, these experts recommend avoiding use of dabigatran in patients with a Clcr <50 mL/minute who are taking P-glycoprotein inhibitors.
Drugs Affecting Hemostasis
Potential increased risk of hemorrhage. Promptly evaluate any manifestations of bleeding.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Amiodarone |
Increased dabigatran concentrations and AUC; increased renal clearance of dabigatran No meaningful alteration of amiodarone pharmacokinetics |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute Increased renal clearance of dabigatran may persist after amiodarone discontinuance due to long amiodarone half-life |
|
Anticoagulants, other |
Increased risk of bleeding |
Monitor for bleeding manifestations |
|
Aspirin |
Increased risk of bleeding Potential increased risk of bleeding with chronic NSAIA use |
Monitor for bleeding manifestations Large clinical trial in patients with atrial fibrillation demonstrated a 2-fold increase in major bleeding events/year with concomitant aspirin and dabigatran; similar to observed increased risk with concurrent aspirin and warfarin |
|
Atorvastatin |
Pharmacokinetic interaction unlikely |
|
|
Clarithromycin |
Pharmacokinetic interaction unlikely |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute |
|
Clopidogrel |
Increased risk of bleeding Potentially increased dabigatran concentrations and AUC |
Monitor for bleeding manifestations Large clinical trial in patients with atrial fibrillation demonstrated a 2-fold increase in major bleeding events/year with concomitant clopidogrel and dabigatran; similar to observed increased risk with concurrent clopidogrel and warfarin |
|
Diclofenac |
Pharmacokinetic interaction unlikely Potentially increased risk of bleeding with chronic NSAIA use |
Monitor for bleeding manifestations |
|
Digoxin |
Pharmacokinetic interaction unlikely |
|
|
Dronedarone |
Increased systemic exposure to dabigatran; lesser degree of increase when dronedarone administered 2 hours after dabigatran |
Nonvalvular atrial fibrillation: Reduce dosage to 75 mg twice daily in patients with moderate renal impairment (Clcr 30–50 mL/minute); avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Separate administration of dabigatran and dronedarone by several hours in patients with Clcr ≥50 mL/minute; avoid concomitant use in patients with Clcr <50 mL/minute |
|
Enoxaparin |
Increased risk of bleeding No alteration in dabigatran systemic exposure or pharmacodynamic assessments (i.e., aPTT, ECT, diluted thrombin time [dTT]) when dabigatran started 24 hours after last dose of enoxaparin |
Monitor for bleeding manifestations |
|
Heparin |
Increased risk of bleeding |
Monitor for bleeding manifestations |
|
Ketoconazole |
Increased dabigatran concentrations and AUC |
Nonvalvular atrial fibrillation: Reduce dosage to 75 mg twice daily in patients with moderate renal impairment (Clcr 30–50 mL/minute); avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Separate administration of dabigatran and ketoconazole by several hours in patients with Clcr ≥50 mL/minute; avoid concomitant use in patients with Clcr <50 mL/minute |
|
NSAIAs |
Increased risk of bleeding with chronic NSAIA use |
Monitor for bleeding manifestations |
|
Pantoprazole |
Decreased dabigatran concentrations and AUC Pharmacokinetics of pantoprazole not affected |
Interaction not considered clinically important |
|
Quinidine |
Increased dabigatran concentrations and AUC |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute |
|
Rifampin |
Decreased dabigatran concentrations and AUC |
Avoid concurrent use |
|
Thrombolytic agents |
Increased risk of bleeding |
Monitor for bleeding manifestations |
|
Ticagrelor |
Increased steady-state peak plasma concentration and AUC of dabigatran; magnitude of increase dependent on dose and timing of dabigatran administration |
Increased bleeding risk with concurrent use. Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute |
|
Verapamil |
Potentially increased dabigatran concentrations and AUC Interaction dependent on verapamil formulation and timing of administration; verapamil immediate release given 1 hour prior to dabigatran increased dabigatran AUC 2.4-fold, while verapamil given 2 hours after dabigatran had negligible effects |
Nonvalvular atrial fibrillation: Avoid concomitant use in patients with severe renal impairment (Clcr 15–30 mL/minute) Treatment or secondary prevention of venous thromboembolism: Avoid concomitant use in patients with Clcr <50 mL/minute Thromboprophylaxis following hip-replacement surgery: Avoid concomitant use in patients with Clcr <50 mL/minute |
|
Warfarin |
Increased risk of bleeding |
INR for monitoring warfarin more accurate ≥2 days after discontinuing dabigatran; monitor for bleeding manifestations |
Dabigatran Pharmacokinetics
Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester and hydrolyzed to the active moiety, dabigatran, by esterases in plasma and the liver.
Dabigatran undergoes conjugation to acyl glucuronides that have similar pharmacologic activity to dabigatran and account for approximately 20% of the total plasma dabigatran concentration. The PK of dabigatran are generally described in terms of total plasma dabigatran concentrations, which includes the major acyl glucuronide metabolites. Dabigatran exhibits linear, dose-dependent PK.
Absorption
Bioavailability
Absolute bioavailability of dabigatran following oral administration of dabigatran etexilate approximately 3–7%.
Oral absorption is formulation-dependent. The oral pellet formulation is 37% more bioavailable in healthy adults compared to the capsule.
Available in capsules and oral pellets and relative bioavailability between dosage forms is age-dependent.
Onset
Peak plasma concentration attained approximately 1–2 hours following oral administration. Maximal effects on coagulation assays expected within 2 hours of administration; such effects correlate with peak plasma concentrations. Similar PK/PD effects on coagulation assays observed in pediatric patients.
Duration
Effects on anticoagulation assays decline by approximately 50% at 12 hours after administration.
Food
High-fat meal delays time to peak plasma concentration by 2 hours but does not affect bioavailability.
Special Populations
Similar PK/PD effects on coagulation assays observed in pediatric patients.
When dabigatran was administered 1–3 hours after completing hip arthroplasty, time to peak plasma concentrations was delayed to 6 hours but returned to normal day after surgery. There was no effect on AUC.
In adult patients with mild, moderate, or severe renal impairment, AUC estimated to be increased 1.5-, 3.2-, or 6.3-fold respectively; peak plasma concentrations increased 1.1-, 1.7-, or 2.1-fold, respectively.
Distribution
Extent
Not known whether dabigatran distributes into human milk; distributed into milk in rats.
Plasma Protein Binding
Approximately 35%.
Elimination
Metabolism
Dabigatran etexilate is a prodrug of dabigatran; rapidly absorbed following oral administration and hydrolyzed in the plasma and liver to dabigatran, the active moiety.
Elimination Route
Bioavailable dabigatran excreted principally (80%) in urine as unchanged drug. Approximately 86% of total oral dose is eliminated in the feces.
Removed by dialysis; redistribution may occur.
Half-life
Oral capsules: 12–17 hours in healthy adults and 12–14 hours in pediatric patients.
Oral pellets: 9–11 hours in pediatric patients.
Special Populations
In adult patients with mild, moderate, or severe renal impairment, plasma half-life averages 15, 18, or 27 hours, respectively.
In patients with moderate hepatic impairment (Child-Pugh class B), large interpatient variability apparent, but no consistent change in exposure or PD response.
Stability
Storage
Oral
Capsules
20–25°C (excursions permitted to 15–30°C). Store in original package (i.e., bottles or blister pack) to protect from moisture.
Once bottle is opened, manufacturer recommends that drug be used within 4 months. Keep bottle tightly closed.
Oral Pellets
20–25°C (excursions permitted to 15–30°C). Store in original aluminum package to protect from moisture.
Do not open the packets until ready for use.
Use the packets within 6 months of opening the aluminum bag.
Actions
-
Selective, competitive, reversible direct thrombin inhibitor.
Prevents thrombus formation by binding free and clot-bound thrombin, thereby inhibiting the conversion of fibrinogen to fibrin. Also inhibits thrombin-mediated platelet aggregation. Dabigatran etexilate mesylate is absorbed as the dabigatran etexilate ester and hydrolyzed to the active moiety, dabigatran, by esterases in plasma and the liver.
-
Metabolized to several acyl glucuronides with similar activity as dabigatran.
-
Prolongs dTT and ECT linearly over the range of therapeutic plasma concentrations.
-
Prolongs aPTT in a curvilinear manner. INR may be elevated, but is not a reliable assessment of dabigatran activity.
Advice to Patients
-
Instruct patients to take dabigatran exactly as prescribed and to not discontinue therapy without first consulting a clinician.
-
Inform patients that the oral capsule and pellets are not interchangeable; do not substitute different dosage forms on a mg-to-mg basis. Consult with a health care provider to make sure the proper dosage form and dosage are used.
-
Advise patients of the importance of having an adult caregiver administer dabigatran to pediatric patients.
-
Instruct patients to take a missed dose (capsules or oral pellets) as soon as it is remembered on the same day, but only if it can be taken at least 6 hours prior to the next scheduled dose. Do not take 2 doses at the same time to make up for a missed dose.
-
Inform patients that they may bruise and/or bleed more easily and that a longer than normal time may be required to stop bleeding when taking dabigatran; advise patients on how to recognize signs and symptoms of bleeding.
-
Advise patients to inform their clinicians immediately if any unusual bleeding or bruising, including menstrual or vaginal bleeding that is heavier than normal, occurs during therapy.
-
Dabigatran is not for patients with artificial heart valves; advise patients to inform their health care provider if they had or will have heart valve surgery.
-
Dabigatran is not recommended for use in patients with antiphospholipid syndrome (APS), especially with positive triple antibody testing; advise patients to inform their health care provider if they have APS.
-
Inform patients about the risk of adverse GI reactions. Advise patients to consult their healthcare provider if they experience dyspepsia, burning, nausea, abdominal pain/discomfort, epigastric discomfort, or indigestion.
-
Advise patients who have had neuraxial anesthesia or spinal puncture to monitor for manifestations of spinal or epidural hematoma (e.g., numbness or weakness of legs, bowel or bladder dysfunction), particularly if they are receiving concomitant nonsteroidal anti-inflammatory agents (NSAIAs), platelet inhibitors, or other anticoagulants; inform patients to seek emergency medical attention if any of these symptoms occur.
-
Advise patients to inform their clinicians (e.g., physicians, dentists) that they are receiving dabigatran therapy before scheduling any surgery or invasive procedures, including dental procedures.
-
Advise patients to swallow dabigatran capsules whole with a full glass of water, without opening, chewing, or otherwise emptying the contents of the capsule. Advise patients to inform their health care provider if they are unable to swallow the capsule whole. Do not sprinkle contents of capsules on food or into a beverage.
-
Inform patients of special storage and handling requirements for dabigatran capsules. Store the drug capsules only in the original container (bottle or blister package) and protect from moisture; do not store capsules in pill boxes or organizers. Remove only one capsule from the bottle at a time, right before use, and close the bottle tightly immediately after use. When more than one bottle is dispensed, advise the patient to open only one bottle at a time. For blister packages of capsules, do not open or puncture the blister until time of use. The manufacturer states that dabigatran capsules should be used within 4 months after the bottle is first opened.
-
Advise the adult caregiver on the proper administration of dabigatran oral pellets. The oral pellets should be sprinkled on baby rice cereal (prepared with water), mashed carrots, apple sauce, or mashed bananas, or taken with apple juice. Do not mix with any other food or liquid. Do not mix the oral pellets with milk, milk products, or foods that contain milk. The oral pellets should be administered before meals to help ensure that the full dose is taken.
-
Advise the caregiver to administer the oral pellets right away or within 30 minutes after mixing; discard oral pellets that have been in contact with soft food or apple juice for more than 30 minutes. If the child only takes part of their oral pellet dose, do not give another dose at that time; administer the next dose at the regularly scheduled time, about 12 hours later.
-
Advise caregivers to not use an oral syringe or feeding tube to administer the oral pellets.
-
Inform caregivers of special storage and handling requirements for dabigatran oral pellets. Oral pellet packets are dispensed in an aluminum bag with a desiccant. Keep the oral pellet packets in the original aluminum bag to keep them dry. Remove only one packet at a time. Do not open the oral pellet packet until ready to administer the dose. After opening the aluminum bag, oral pellets must be used within 6 months.
-
Advise females to inform their clinician if they are or plan to become pregnant or plan to breast-feed.
-
Advise patients to inform their clinician of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary and herbal supplements, as well as any concomitant illnesses.
-
Advise patients of other important precautionary information. (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
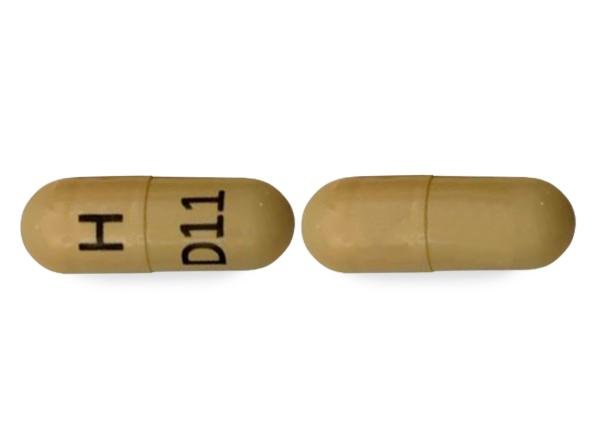
Oral |
Capsules |
75 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
|
110 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
150 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
Pellets |
20 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
|
|
30 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
40 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
50 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
110 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
||
|
150 mg (of dabigatran etexilate) |
Pradaxa |
Boehringer Ingelheim |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions March 22, 2023. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about dabigatran
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (102)
- Drug images
- Latest FDA alerts (5)
- Side effects
- Dosage information
- During pregnancy
- Drug class: thrombin inhibitors
- Breastfeeding
- En español