Zolmitriptan (Monograph)
Brand name: Zomig
Drug class: Selective Serotonin Agonists
- Antimigraine Agents
- Selective Vascular Serotonin Type 1-Like Receptor Agonists
- 5-HT1 Agonists
VA class: CN105
Chemical name: (S)-4-[[3-[2-(dimethylamino)ethyl]indol-5-yl]methyl]-2-oxazolidinone
Molecular formula: C16H21N3O2
CAS number: 139264-17-8
Introduction
Selective serotonin (5-hydroxytryptamine; 5-HT) type 1B and 1D receptor agonist (“triptan”).
Uses for Zolmitriptan
Vascular Headaches
Acute treatment of migraine attacks with or without aura.
Not recommended for management of hemiplegic or basilar migraine or for prophylaxis of migraine.
Safety and efficacy not established for management of cluster headaches.
Zolmitriptan Dosage and Administration
Administration
Administer orally or intranasally.
Oral Administration
Administer orally as conventional or orally disintegrating tablets without regard to meals.
To achieve a dose of 1.25 mg, manually break the scored 2.5-mg conventional tablet in half. Do not break orally disintegrating tablets.
Just prior to administration of orally disintegrating tablet, remove tablet from blister package; peel open blister package, place tablet on tongue to dissolve, and swallow with saliva.
Administration of orally disintegrating tablet with liquid is not necessary.
Intranasal Administration
Administer intranasally as a single spray into 1 nostril.
Do not spray contents into eyes.
To administer, blow nose gently and remove protective cap just before use. Hold nasal spray device gently and do not press plunger until tip is placed into nostril. Block one nostril by pressing firmly on side of nose and put tip into other nostril as far as feels comfortable. Tilt head slightly back and breathe gently through nose while pressing plunger firmly with thumb; a click may be heard. Keep head tilted slightly back and remove tip of device from nose; breathe gently through mouth for 5–10 seconds. Liquid may be felt in nose or back of throat. Consult manufacturer’s patient information for complete directions.
Single-use spray pump; discard after use.
Dosage
Due to similarity in systemic exposure, dosage adjustments with oral and intranasal formulations should be similar; doses <5 mg can be achieved only through use of oral formulations. Dose of 1.25 mg can be achieved only with conventional oral tablets.
Adults
Vascular Headaches
Migraine
OralInitially, 1.25 or 2.5 mg. In clinical studies, single oral doses of 1 (not commercially available in US), 2.5, or 5 mg were effective, but the 2.5- and 5-mg doses were effective in a greater proportion of patients. The 5-mg dose appears to offer little additional benefit and is associated with increased risk of adverse effects.
If headache has not resolved by 2 hours after initial dose or if it recurs after transient improvement, dose may be repeated after ≥2 hours.
Following failure to respond to first dose, reconsider diagnosis of migraine prior to administration of a second dose.
Intranasal5 mg (1 spray) as a single dose; individualize selection of dosage and administration route.
If headache recurs, dose may be repeated after 2 hours.
Following failure to respond to first dose, reconsider diagnosis of migraine prior to administration of a second dose.
Prescribing Limits
Adults
Vascular Headaches
Migraine
OralMaximum 5 mg per single dose and 10 mg in any 24-hour period.
Safety of treating an average of >3 headaches per 30-day period has not been established.
IntranasalMaximum 10 mg in any 24-hour period.
Safety of treating an average of >4 headaches per 30-day period has not been established.
Special Populations
Hepatic Impairment
Vascular Headaches
Migraine
OralModerate to severe hepatic impairment: Initially, 1.25 mg. In patients with severe hepatic impairment, maximum 5 mg in any 24-hour period.
IntranasalUse of intranasal formulation not recommended; recommended doses can be achieved only with conventional oral formulations.
Geriatric Patients
Select dosage with caution, usually starting at the low end of the dosage range, because of increased frequency of decreased hepatic, renal, or cardiac function and of concomitant disease or drug therapy.
Cautions for Zolmitriptan
Contraindications
-
Ischemic heart disease (e.g., angina pectoris, history of MI, documented silent ischemia).
-
Coronary artery vasospasm (e.g., Prinzmetal variant angina).
-
Wolff-Parkinson-White syndrome or cardiac arrhythmias associated with other accessory pathway conduction disorders.
-
Uncontrolled hypertension.
-
Other serious underlying cardiovascular disease.
-
Cerebrovascular syndromes (e.g., stroke syndromes, TIAs).
-
Peripheral vascular disease or ischemic bowel disease.
-
Hemiplegic or basilar migraine.
-
Treatment within previous 24 hours with another 5-HT1 receptor agonist or an ergot alkaloid. (See Specific Drugs under Interactions.)
-
Concurrent or recent (within 2 weeks) treatment with an MAO-A inhibitor. (See Specific Drugs under Interactions.)
-
Known sensitivity to zolmitriptan or any ingredient in the formulation.
Warnings/Precautions
Careful Diagnosis of Migraine
Use only in patients in whom a clear diagnosis of migraine has been established.
If first migraine attack treated with zolmitriptan fails to respond to the drug, reconsider diagnosis before administering zolmitriptan to treat subsequent attacks.
Exclude other potentially serious neurologic disorders before administering zolmitriptan to patients not previously diagnosed with migraine or to those with atypical symptoms.
Cardiac Effects
Possible myocardial ischemia and/or infarction and coronary vasospasm, even in patients without a history of CAD. Contraindicated in patients with ischemic or vasospastic heart disease.
Possible fatal or life-threatening cardiac rhythm disturbances (e.g., ventricular tachycardia or fibrillation). Discontinue if such disturbances occur.
Contraindicated in patients with symptomatic Wolff-Parkinson-White syndrome or cardiac arrhythmias associated with other accessory pathway conduction disorders.
Tightness, pain, pressure, and heaviness in the precordium, throat, neck, and jaw occur frequently but usually are noncardiac in origin. Manufacturer states that cardiovascular evaluation should be performed if patient is at high cardiac risk.
Patients at Risk for CAD
Perform cardiovascular evaluation prior to initiating therapy in patients with multiple cardiovascular risk factors (e.g., postmenopausal women; men >40 years of age; patients with risk factors such as hypertension, hypercholesterolemia, smoking, obesity, diabetes, family history of CAD) who have not previously received 5-HT1 receptor agonist therapy.
If evaluation provides evidence of CAD or coronary vasospasm, do not administer the drug.
If results of evaluation are satisfactory, consider administering the initial dose in a medically supervised setting followed immediately by an ECG.
Periodic cardiovascular evaluation recommended in patients with risk factors for CAD if receiving intermittent long-term therapy.
Cerebrovascular Events
Possible cerebral or subarachnoid hemorrhage and stroke, sometimes fatal. (See Careful Diagnosis of Migraine under Cautions.) Discontinue therapy if a cerebrovascular event occurs.
Risk of certain cerebrovascular events (e.g., stroke, hemorrhage, TIA) may be increased in patients with migraine.
Other Vasospastic Effects
Possible noncoronary vasospastic reactions (e.g., peripheral vascular ischemia, GI ischemia and infarction with abdominal pain and bloody diarrhea, splenic infarction, Raynaud’s syndrome); transient or permanent blindness and partial vision loss reported very rarely in patients receiving 5-HT1 receptor agonists.
If signs or symptoms suggestive of vasospasm occur following administration, evaluate patient to rule out vasospastic reaction before administering additional doses.
Hypertensive Effects
Substantial increases in BP, including hypertensive crisis with acute impairment of organ systems, reported rarely with 5-HT1 receptor agonists in patients with or without history of hypertension. May be pronounced in patients with moderate to severe hepatic impairment. (See Hepatic Impairment under Cautions.) Monitor BP in all patients receiving zolmitriptan.
Increases in mean pulmonary arterial pressure observed following administration of a 5-HT1 receptor agonist to patients with suspected CAD who were undergoing cardiac catheterization.
Serotonin Syndrome
Potentially life-threatening serotonin syndrome reported in patients receiving 5-HT1 receptor agonists, particularly in those receiving SSRIs or SNRIs concomitantly. (See Specific Drugs under Interactions.) Also may occur in patients receiving MAO inhibitors or tricyclic antidepressants concomitantly.
Symptoms may include mental status changes (e.g., agitation, hallucinations, coma), autonomic instability (e.g., tachycardia, labile BP, hyperthermia), neuromuscular aberrations (e.g., hyperreflexia, incoordination), and/or GI symptoms (e.g., nausea, vomiting, diarrhea).
If manifestations of serotonin syndrome occur, discontinue zolmitriptan and any concurrently administered serotonergic agents and initiate supportive and symptomatic treatment.
Medication Overuse Headache
Overuse of drugs indicated for management of acute migraine attacks (e.g., use of 5-HT1 receptor agonists, ergotamine, opiates, or certain analgesic combinations on a regular basis for ≥10 days per month) may result in migraine-like daily headaches or a marked increase in frequency of migraine attacks.
Detoxification, including withdrawal of overused drugs; treatment of withdrawal symptoms (e.g., transient worsening of headaches); and consideration of prophylactic migraine therapy may be necessary.
Local Effects
Possible local irritation or soreness after intranasal administration. Adverse effects perceived in nasopharynx, occasionally severe, usually resolve within 1 hour.
No clinically important nasopharyngeal changes observed by examination following repeated use for up to 1 year’s duration.
Sensitivity Reactions
Hypersensitivity reactions (e.g., angioedema, anaphylaxis) reported.
Ocular Effects
Possible accumulation of zolmitriptan and/or its metabolites in melanin-rich tissues (e.g., eye) over time, resulting in potential toxicity in these tissues with extended use.
Phenylketonuria
Each 2.5- or 5-mg Zomig-ZMT orally disintegrating tablet contains aspartame, which is metabolized in GI tract to provide 2.81 or 5.62 mg of phenylalanine, respectively. Conventional tablets do not contain aspartame.
Specific Populations
Pregnancy
Category C.
Lactation
Distributed into milk in rats; not known whether distributed into human milk. Discontinue nursing or the drug.
Pediatric Use
Safety and efficacy not established in children <18 years of age; use not recommended.
Studies in adolescents 12–17 years of age with migraines failed to demonstrate efficacy. Adverse effects similar to those reported in adults. Serious adverse events reported in limited number of pediatric patients receiving 5-HT1 receptor agonists.
Not studied in children <12 years of age.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether they respond differently than younger adults; select dosage with caution.
Pharmacokinetic profile similar to that in younger adults.
Hepatic Impairment
Substantial elevation of BP observed in some patients with moderate to severe hepatic impairment following 10-mg oral dose. Use with caution and adjust dosage in these patients. (See Hepatic Impairment under Dosage and Administration.)
Common Adverse Effects
With oral therapy: Dizziness, paresthesia, neck/throat/jaw/chest symptoms (e.g., pain, tightness, pressure, heaviness), other sensations of heaviness/pressure/tightness, nausea, somnolence, warm or cold sensation, asthenia, dry mouth, dyspepsia, dysphagia, vertigo, sweating.
With intranasal therapy: Paresthesia, hyperesthesia, unusual taste, throat pain, pain of specified location, nausea, somnolence, disorder or discomfort of the nasal cavity, asthenia, tightness of the throat, dry mouth.
Drug Interactions
Appears to be metabolized by CYP1A2; active N-desmethyl metabolite appears to be further metabolized by MAO-A.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
Increased time to peak plasma acetaminophen concentrations |
|
|
Antidepressants, SSRIs (e.g., citalopram, escitalopram, fluoxetine, fluvoxamine, paroxetine, sertraline) and SNRIs (e.g., duloxetine, venlafaxine) |
Potentially life-threatening serotonin syndrome Zolmitriptan pharmacokinetics or effect on BP not altered by fluoxetine pretreatment |
Observe carefully if used concomitantly, particularly during treatment initiation, dosage increases, or when another serotonergic agent is initiated |
|
Cimetidine |
Increased half-life and systemic exposure to zolmitriptan and its active metabolite |
Limit zolmitriptan dosage: Maximum 2.5 mg as single dose; maximum 5 mg in any 24-hour period |
|
Ergot alkaloids (e.g., ergotamine, dihydroergotamine, methysergide [no longer commercially available in the US]) |
Additive vasospastic effects |
Use within 24 hours contraindicated |
|
5-HT1 receptor agonists |
Additive vasospastic effects |
Use within 24 hours contraindicated |
|
MAO inhibitors |
Increased plasma concentrations of zolmitriptan and its active metabolite with concurrent use of MAO-A inhibitors; selegiline (selective MAO-B inhibitor) did not affect pharmacokinetics of zolmitriptan or its active metabolite |
Use of oral or intranasal zolmitriptan within 2 weeks of MAO-A inhibitor contraindicated |
|
Metoclopramide |
Metoclopramide (single 10-mg dose) did not affect pharmacokinetics of zolmitriptan or its metabolites |
|
|
Oral contraceptives |
Increased plasma zolmitriptan concentrations |
|
|
Propranolol |
Increased plasma zolmitriptan concentrations; peak zolmitriptan concentration may be delayed |
|
|
Xylometazoline |
Topical application of xylometazoline to nasal mucosa 30 minutes prior to intranasal zolmitriptan did not affect zolmitriptan pharmacokinetics |
Zolmitriptan Pharmacokinetics
Absorption
Bioavailability
Well absorbed after oral administration, with peak plasma concentrations attained within 1.5 hours (conventional tablets) or 3 hours (orally disintegrating tablets). Rapidly absorbed via the nasopharynx after intranasal administration, with peak plasma concentrations attained within 3 hours.
Mean absolute bioavailability after oral administration is approximately 40%; mean bioavailability of nasal solution is 102% compared with oral tablet.
Mean plasma concentrations after oral administration are increased by up to 1.5-fold in females compared with males.
Food
Food does not substantially affect bioavailability.
Distribution
Plasma Protein Binding
25%.
Elimination
Metabolism
Undergoes hepatic metabolism to form 3 principal metabolites, including N-desmethyl zolmitriptan (5-HT1B/1D potency is 2–6 times that of zolmitriptan). Formation of N-desmethyl zolmitriptan may depend on CYP1A2; MAO-A appears to mediate metabolism of N-desmethyl zolmitriptan.
Elimination Route
Excreted in urine (65%) and feces (30%) as unchanged drug and metabolites; dose recovered in urine as unchanged drug (8%) and indole acetic acid (31%), N-oxide (7%), and N-desmethyl (4%) metabolites.
Half-life
Approximately 3 hours for zolmitriptan and active N-desmethyl metabolite after oral or intranasal administration.
Special Populations
In patients with severe hepatic impairment, peak plasma concentrations, time to achieve peak plasma concentrations, and AUC are 1.5-, 2-, and 3-fold higher, respectively, than in healthy individuals after oral administration. Pharmacokinetics of nasal spray not evaluated in patients with hepatic impairment.
In patients with severe renal impairment (Clcr 5–25 mL/minute), clearance is reduced by 25% after oral administration; no substantial change in clearance in patients with moderate renal impairment (Clcr 26–50 mL/minute). Pharmacokinetics of nasal spray not evaluated in patients with renal impairment.
Stability
Storage
Oral
Conventional and Orally Disintegrating Tablets
20–25°C; protect from light and moisture.
Intranasal
Solution
20–25°C.
Actions
-
Binds with high affinity to 5-HT1B and 5-HT1D receptors.
-
Structurally and pharmacologically related to other selective 5-HT1B/1D receptor agonists (e.g., almotriptan, eletriptan, frovatriptan, naratriptan, rizatriptan, sumatriptan).
-
Precise mechanism of action not established; may ameliorate migraine through selective constriction of certain intracranial blood vessels, inhibition of neuropeptide release, and reduced transmission in trigeminal pain pathway.
Advice to Patients
-
Risk of serious cardiovascular or cerebrovascular events (e.g., MI, stroke) or other vasospastic reactions. Importance of seeking medical care if symptoms of such reactions (e.g., shortness of breath, weakness, slurring of speech, sudden or severe abdominal pain, difficulty in seeing, or tightness, pain, pressure, or heaviness in the chest, throat, neck, or jaw) occur and of not taking zolmitriptan again until evaluated by clinician.
-
Importance of adhering to prescribed directions for use. Importance of patient reading manufacturer's patient information before initial use and each time prescription is refilled.
-
Importance of informing patients of risk of serotonin syndrome, particularly with concurrent use of zolmitriptan and an SSRI or SNRI. Importance of seeking immediate medical attention if symptoms of serotonin syndrome develop.
-
Overuse of drugs indicated for the management of acute migraine attacks may exacerbate headaches; importance of recording headache frequency and drug use to monitor effectiveness of treatment.
-
For patients taking zolmitriptan orally disintegrating tablets, importance of not removing tablet from blister package until just before administering dose; importance of peeling blister open and placing tablet on tongue to dissolve and be swallowed with saliva. Orally disintegrating tablets should not be broken.
-
Importance of informing patients with phenylketonuria that orally disintegrating tablets contain aspartame.
-
For patients using zolmitriptan nasal spray, importance of not spraying nasal solution into the eyes.
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, dietary supplements, and herbal supplements, as well as any concomitant illnesses (e.g., cardiovascular disease).
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Nasal |
Solution |
5 mg/0.1 mL |
Zomig Nasal Spray |
AstraZeneca |
|
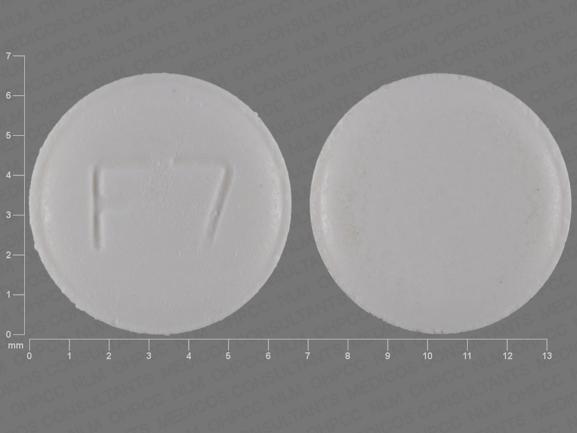
Oral |
Tablets, film-coated |
2.5 mg |
Zomig (scored) |
AstraZeneca |
|
5 mg |
Zomig |
AstraZeneca |
||
|
Tablets, orally disintegrating |
2.5 mg |
Zomig-ZMT |
AstraZeneca |
|
|
5 mg |
Zomig-ZMT |
AstraZeneca |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions July 31, 2013. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about zolmitriptan
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (164)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: antimigraine agents
- Breastfeeding