Venetoclax (Monograph)
Brand name: Venclexta
Drug class: Antineoplastic Agents
- B-cell lymphoma 2 inhibitor
- BCL-2 inhibitor
Chemical name: 4-Dimethyl-1-cyclohexen-1-yl]methyl]-1-piperazinyl]-N-[[3-nitro-4-[[(tetrahydro-2H-pyran-4-yl)methyl]amino]phenyl]sulfonyl]-2-(1H-pyrrolo[2,3-b]pyridin-5-yloxy)-benzamide, 4-[4-[[2-(4-chlorophenyl)-4
Molecular formula: C45H50ClN7O7S
CAS number: 1257044-40-8
Introduction
Antineoplastic agent; inhibitor of B-cell lymphoma 2 (BCL-2).1
Uses for Venetoclax
Chronic Lymphocytic Leukemia (CLL) and Small Lymphocytic Lymphoma (SLL)
Treatment of CLL or SLL.1 2 16 17 18 19 20 21 22 23
Designated an orphan drug by FDA for treatment of CLL/SLL.3
Generally recommended among first-line treatment options for symptomatic CLL.2000 2001
Acute Myeloid Leukemia (AML)
Treatment of newly diagnosed AML in combination with azacitidine, decitabine, or low-dose cytarabine for patients ≥75 years of age or with comorbidities that preclude use of intensive induction chemotherapy.1 24 25 26 27 28 29 30
Designated an orphan drug by FDA for treatment of AML.3
Generally recommended in combination with other agents for treatment of AML in older adults or adults with significant comorbidities.3015 3016
Venetoclax Dosage and Administration
General
Pretreatment Screening
-
Prior to initiating first dose, assess patients for risk of tumor lysis syndrome and give appropriate prophylaxis (e.g., adequate hydration and antihyperuricemic agents) based on tumor burden at baseline and other risk factors (e.g., renal impairment, malignancy).1
-
In patients with CLL or SLL, assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine); correct any preexisting abnormalities prior to initiation of therapy.1
-
In patients with AML, patients should have a leukocyte count less than 25,000/mm3 prior to initiation of venetoclax therapy; pretreatment cytoreduction may be necessary.1 Assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine) and correct any preexisting abnormalities prior to initiation of therapy.1
-
Perform pregnancy testing prior to initiating treatment in females of reproductive potential.1
Patient Monitoring
-
Institute appropriate prophylaxis and monitoring for tumor lysis syndrome according to tumor burden at baseline.1
-
In patients with CML or SLL: Assess risk for tumor lysis syndrome and provide prophylaxis and monitoring when starting therapy and prior to resuming therapy following dosage interruption lasting >1 week during initial dose-escalation period or >2 weeks following completion of the dose-escalation period.1
-
In patients with AML: Assess blood chemistries for tumor lysis syndrome (i.e., potassium, phosphorus, calcium, uric acid, creatinine) prior to each dose, at 6–8 hours following each new dose during dosage escalation, and 24 hours after reaching the final dosage.1 Consider increased laboratory monitoring and reduction of initial dosage for patients with risk factors for tumor lysis syndrome.1
-
Monitor CBC periodically during therapy.1
-
Monitor for manifestations of infection during therapy.1
Premedication and Prophylaxis
- Tumor Lysis Syndrome
-
In patients with AML, initiate prophylaxis (i.e., hydration and an antihyperuricemic agent) and monitor for tumor lysis syndrome prior to first dose and during dose escalation.1 Prior to initiation of therapy, leukocyte count should be <25,000/mm3; pretreatment cytoreduction may be necessary.1 Assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine) prior to each dose, at 6–8 hours following each new dose during the dose-escalation period, and 24 hours following completion of the dose-escalation period.1 Consider increased laboratory monitoring and reduction of starting dosage for patients with risk factors for tumor lysis syndrome.1
-
In patients with CLL or SLL, institute appropriate prophylaxis and monitoring as described in Table 1.1 Assess risk and provide prophylaxis and monitoring when starting therapy and prior to resuming therapy following dosage interruption lasting >1 week during initial dose-escalation period or >2 weeks following completion of the dose-escalation period.1 Administer initial 20- and 50-mg doses of venetoclax in the hospital in patients with high tumor burden at baseline; may administer subsequent doses in the outpatient setting.1 Dosage modifications may be necessary if laboratory evidence or clinical manifestations of tumor lysis syndrome occur during therapy.1
Administer IV hydration if oral hydration is not tolerated
Begin oral hydration 2 days prior to initiating venetoclax, on the day of the first dose, and every time the dose is increased
Initiate antihyperuricemic agent (e.g., allopurinol) 2–3 days prior to initiating venetoclax
|
Tumor Burden |
Prophylaxis |
Monitoring |
|---|---|---|
|
Low tumor burden: All lymph nodes with diameter <5 cm AND absolute lymphocyte count <25,000/mm3 |
Oral hydration (1.5–2 L), and allopurinol |
Assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine) prior to, at 6–8 and 24 hours following the first 20- and 50-mg doses of venetoclax, and prior to each subsequent escalating dose (100, 200, and 400 mg) |
|
Medium tumor burden: Any lymph node diameter 5 cm to <10 cm OR absolute lymphocyte count ≥25,000/mm3 |
Oral hydration (1.5–2 L), and allopurinol |
Assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine) prior to, at 6–8 and 24 hours following the first 20- and 50-mg doses of venetoclax, and prior to each subsequent escalating dose (100, 200, and 400 mg) |
|
Consider additional IV hydration |
In patients with Clcr <80 mL/minute prior to the first 20- and 50-mg doses, consider hospitalization for drug administration and more intensive hydration and monitoring (see the following recommendations for monitoring in hospital) |
|
|
High tumor burden: Any lymph node diameter ≥10 cm OR any lymph node diameter ≥5 cm and absolute lymphocyte count ≥25,000/mm3 |
Oral (1.5–2 L), and IV (150–200 mL/hour as tolerated) hydration and allopurinol |
Hospitalize patients for administration of the first 20- and 50-mg doses of venetoclax; assess blood chemistries (i.e., potassium, phosphorus, calcium, uric acid, creatinine) prior to and at 4, 8, 12, and 24 hours following each dose |
|
Consider rasburicase if baseline uric acid concentrations are elevated |
Administer subsequent escalating doses (100, 200, and 400 mg) in the outpatient setting; assess blood chemistries prior to and at 6–8 and 24 hours following each dose |
Other General Considerations
-
Consider the usual cautions, precautions, and contraindications associated with drugs used in combination with venetoclax.1
Administration
Oral Administration
Administer orally once daily with a meal and full glass of water at approximately the same time each day.1 12 Swallow tablets intact; do not chew, crush, or break.1 Dosage may be delivered using any combination of the approved tablet strengths.1
Dosage
Adults
CLL/SLL
Oral
Recommended dosage is 400 mg once daily; to reduce tumor burden (i.e., debulk) and minimize risk of tumor lysis syndrome, initiate at a low dosage and increase gradually over 5 weeks according to the following schedule: 20 mg daily in first week, 50 mg daily in second week, 100 mg daily in third week, 200 mg daily in fourth week, then 400 mg daily starting the fifth week and thereafter.1
Venetoclax in Combination with Obinutuzumab
OralDuring cycle 1, administer obinutuzumab 100 mg IV on day 1, 900 mg on day 2, and then 1 g on day 8 and day 15.1 During cycles 2–6, administer obinutuzumab 1 g IV on day 1 of each 28-day cycle.1 Do not continue obinutuzumab beyond 6 cycles.1
On cycle 1 day 22, initiate venetoclax at a low dosage and titrate over 5 weeks according to the following schedule: 20 mg daily in first week, 50 mg daily in second week, 100 mg daily in third week, 200 mg daily in fourth week, then 400 mg daily in the fifth week and thereafter.1 After completing the dosage escalation phase on cycle 2 day 28, continue venetoclax at a dosage of 400 mg once daily from cycle 3 day 1 until the last day of cycle 12.1
Venetoclax in Combination with Rituximab
OralInitiate venetoclax at a low dosage and titrate over 5 weeks according to the following schedule: 20 mg daily in first week, 50 mg daily in second week, 100 mg daily in third week, 200 mg daily in fourth week, then 400 mg daily in the fifth week and thereafter.1 Continue venetoclax 400 mg once daily for 24 months starting from day 1 of cycle 1 of rituximab.1
Initiate rituximab after patient has completed the 5-week dose-escalation for venetoclax and has received venetoclax at the recommended dosage of 400 mg once daily for 7 days.1 Administer rituximab 375 mg/m2 IV on day 1 of cycle 1.1 For cycles 2–6, administer rituximab 500 mg/m2 IV on day 1 of each 28-day cycle.1 Do not continue rituximab beyond 6 cycles.1
Venetoclax Monotherapy
Oral400 mg once daily; initiate at a low dosage and titrate over 5 weeks according to the following schedule: 20 mg daily in first week, 50 mg daily in second week, 100 mg daily in third week, 200 mg daily in fourth week, then 400 mg daily thereafter.1
Continue therapy until disease progression or unacceptable toxicity.1
Dosage Modification for Toxicity in Patients with CLL/SLL
OralIf a dosage modification is needed in patients with CLL/SLL, adjust dosage by one dose level (see Table 2).1
If dosage reduction occurs during the initial 5-week titration period, continue reduced dosage for 1 week before escalating back to previous dosage.1
If interruption of therapy is necessary for >1 week during the initial 5-week titration period or for >2 weeks while receiving venetoclax 400 mg once daily, reassess risk for tumor lysis syndrome to determine if a reduced dosage is necessary when resuming therapy.1
Larger dose reductions may be required at the discretion of the clinician1
|
Current Venetoclax Dosage |
Dosage Reduction after Recovery from Toxicity |
|---|---|
|
400 mg |
Restart at 300 mg once daily |
|
300 mg |
Restart at 200 mg once daily |
|
200 mg |
Restart at 100 mg once daily |
|
100 mg |
Restart at 50 mg once daily |
|
50 mg |
Restart at 20 mg once daily |
|
20 mg |
Restart at 10 mg once daily |
If adverse effects occur in patients with CLL or SLL, see Table 3 for recommended dosage modifications (i.e., temporary interruption of therapy, dosage reduction, discontinuance of therapy).1
|
Adverse Reaction and Severity |
Modification |
|---|---|
|
Tumor Lysis Syndrome |
|
|
Blood chemistry abnormalities or symptoms consistent with tumor lysis syndrome |
Withhold therapy |
|
If resolution occurs within 24–48 hours of the last dose, resume therapy at the same dosage; however, if laboratory abnormalities require >48 hours to resolve or if clinical tumor lysis syndrome (clinical sequelae may include acute renal failure, cardiac arrhythmias, sudden death, and/or seizures) occurs, resume therapy at a reduced dosage when resolution occurs (see Table 2) |
|
|
Hematologic Toxicity |
|
|
Grade 3 neutropenia associated with fever or infection |
First occurrence: Withhold therapy; when toxicity improves to grade 1 or less, resume at same dosage |
|
Subsequent occurrences: Withhold therapy, resume therapy at a reduced dosage when the toxicity resolves (see Table 2) |
|
|
Grade 4 hematologic toxicity (except for lymphopenia) |
First occurrence: Withhold therapy; when toxicity improves to grade 1 or less, resume at same dosage |
|
Subsequent occurrences: Withhold therapy, resume therapy at a reduced dosage when the toxicity resolves (see Table 2) |
|
|
Nonhematologic Toxicity |
|
|
Grade 3 or 4 |
First occurrence: Withhold therapy; when toxicity improves to grade 1 or less, resume at same dosage |
|
Subsequent occurrences: Withhold therapy, resume therapy at a reduced dosage when the toxicity resolves (see Table 2) |
Dosage Modification for Concomitant Use with CYP3A or P-gp Inhibitors in Patients with CLL/SLL
OralConcomitant use with a potent or moderate CYP3A inhibitor or a P-gp inhibitor may be contraindicated or reduction of the venetoclax dosage may be necessary as described in Table 4.1 When concomitant use of the potent or moderate CYP3A inhibitor or P-gp inhibitor is discontinued, return venetoclax dosage (after 2–3 days) to dosage used prior to initiation of the CYP3A inhibitor or P-gp inhibitor.1
|
Coadministered Drug |
Concomitant Use During Initial Venetoclax Dosage Escalation |
Concomitant Use with Steady Daily Dosage of Venetoclax (After Dosage Escalation) |
|---|---|---|
|
Posaconazole |
Contraindicated |
Consider using an alternative drug with no or less CYP3A inhibition potential |
|
If concomitant use cannot be avoided, reduce venetoclax dosage to 70 mg daily; monitor frequently for toxicities |
||
|
Other potent CYP3A inhibitor |
Contraindicated |
Consider using an alternative drug with no or less CYP3A inhibition potential |
|
If concomitant use cannot be avoided, reduce venetoclax dosage to 100 mg daily; monitor frequently for toxicities |
||
|
Moderate CYP3A inhibitor |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
|
P-gp inhibitor |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Acute Myeloid Leukemia
Venetoclax in Combination with Azacitidine
OralVenetoclax 400 mg once daily; initiate at a low dosage and titrate over 3 days according to following schedule: 100 mg on day 1, 200 mg on day 2, and 400 mg daily thereafter.1
Administer azacitidine 75 mg/m2 IV or sub-Q once daily on days 1–7 of each 28-day cycle.1
Continue therapy until disease progression or unacceptable toxicity occurs.1
Venetoclax in Combination with Decitabine
OralVenetoclax 400 mg once daily; initiate at a low dosage and titrate over 3 days according to following schedule: 100 mg on day 1, 200 mg on day 2, and 400 mg daily thereafter.1
Administer decitabine 20 mg/m2 IV once daily on days 1–5 of each 28-day cycle.1
Continue therapy until disease progression or unacceptable toxicity occurs.1
Venetoclax in Combination with Low-Dose Cytarabine
OralVenetoclax 600 mg once daily; initiate at a low dosage and titrate over 4 days according to following schedule: 100 mg on day 1, 200 mg on day 2, 400 mg on day 3, and 600 mg daily thereafter.1
Administer cytarabine 20 mg/m2 sub-Q once daily on days 1–10 of each 28-day cycle.1
Continue therapy until disease progression or unacceptable toxicity occurs.1
Dosage Modification for Toxicity in Patients with AML
OralIf adverse reactions occur in patients with AML, see Table 5 for recommended dosage modifications.1
|
Adverse Reaction and Severity |
Occurrence |
Modification |
|---|---|---|
|
Hematologic Toxicity |
||
|
Grade 4 neutropenia with or without fever or infection |
Prior to achieving remission |
In most instances, do not interrupt venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine |
|
Bone marrow evaluation recommended |
||
|
First occurrence after achieving remission and lasts ≥7 days |
Delay subsequent cycle of venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine and monitor CBCs |
|
|
Resume venetoclax at same dosage in combination with azacitidine, decitabine, or low-dose cytarabine when toxicity resolves to grade 1 or 2 |
||
|
Subsequent occurrences in cycles after achieving remission and lasting ≥7 days |
Delay subsequent cycle of venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine and monitor CBCs |
|
|
Resume venetoclax at same dosage in combination with azacitidine, decitabine, or low-dose cytarabine when toxicity resolves to grade 1 or 2, and reduce duration of venetoclax therapy by 7 days during each subsequent cycle (e.g., 28 days reduced to 21 days) |
||
|
Grade 4 thrombocytopenia |
Prior to achieving remission |
In most instances, do not interrupt venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine |
|
Bone marrow evaluation recommended |
||
|
First occurrence after achieving remission and lasts ≥7 days |
Delay subsequent cycle of venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine and monitor CBCs |
|
|
Resume venetoclax at same dosage in combination with azacitidine, decitabine, or low-dose cytarabine when toxicity resolves to grade 1 or 2 |
||
|
Subsequent occurrences in cycles after achieving remission and lasting ≥7 days |
Delay subsequent cycle of venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine and monitor CBCs |
|
|
Resume venetoclax at same dosage in combination with azacitidine, decitabine, or low-dose cytarabine when toxicity resolves to grade 1 or 2, and reduce duration of venetoclax therapy by 7 days during each subsequent cycle (e.g., 28 days reduced to 21 days) |
||
|
Nonhematologic Toxicity |
||
|
Grade 3 or 4 |
Any occurrence |
If persists despite supportive care, withhold venetoclax therapy; resume venetoclax at same dosage when toxicity resolves to grade 1 or less |
Dosage Modification for Concomitant Use with CYP3A or P-gp Inhibitors in Patients with AML
OralAvoid concomitant use with a potent or moderate CYP3A inhibitor or a P-gp inhibitor.1 If concomitant use cannot be avoided, dosage reduction may be necessary as described in Table 6.1 When concomitant use of the potent or moderate CYP3A inhibitor or P-gp inhibitor is discontinued, return venetoclax dosage (after 2–3 days) to dosage used prior to initiation of the CYP3A inhibitor or P-gp inhibitor.1
|
Coadministered Drug |
During Dosage Escalation |
After Dosage Escalation |
|---|---|---|
|
Posaconazole |
Day 1: 10 mg |
Reduce venetoclax dosage to 70 mg daily and monitor frequently for toxicities |
|
Day 2: 20 mg |
||
|
Day 3: 50 mg |
||
|
Day 4: 70 mg |
||
|
Other potent CYP3A inhibitor |
Day 1: 10 mg |
Reduce venetoclax dosage to 100 mg daily and monitor frequently for toxicities |
|
Day 2: 20 mg |
||
|
Day 3: 50 mg |
||
|
Day 4: 100 mg |
||
|
Moderate CYP3A inhibitor |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
|
P-gp inhibitor |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Reduce venetoclax dosage by at least 50% and monitor frequently for toxicities |
Special Populations
Dosage in Hepatic Impairment
Mild or moderate hepatic impairment (Child-Pugh class A or B): No dosage adjustment required.1
Severe hepatic impairment (Child-Pugh class C): Reduce once-daily dosage by 50% and closely monitor for adverse reactions.1
Dosage in Renal Impairment
Mild, moderate, or severe (Clcr ≥15 mL/minute) renal impairment: No dosage adjustment required.1
End-stage renal disease (Clcr <15 mL/minute) or dialysis: Not studied.1
Geriatric Patients
No specific dosage recommendations at this time.1
Cautions for Venetoclax
Contraindications
-
Concomitant use of potent CYP3A inhibitors during initiation of venetoclax therapy and the dose-escalation period in patients with CLL/SLL due to increased risk of tumor lysis syndrome.1
Warnings/Precautions
Tumor Lysis Syndrome
Tumor lysis syndrome, sometimes fatal or resulting in renal failure requiring dialysis, reported.1 7 Risk generally greatest when drug is first initiated, during dose-escalation period, and, in patients with CLL or SLL, during reinitiation of therapy following dosage interruption; laboratory abnormalities requiring prompt medical treatment may occur as early as 6–8 hours following initial dose or after each dosage increase.1
Risk is a continuum based on multiple factors (e.g., type of malignancy, tumor burden, renal impairment, splenomegaly).1 Concomitant use of certain drugs (moderate or potent CYP3A inhibitors or P-gp inhibitors) may further increase risk.1
Assess patient's risk of tumor lysis syndrome (i.e., tumor burden, blood chemistries) and correct any abnormalities prior to initiating therapy and during dose-escalation period.1 Institute appropriate measures (e.g., prophylactic antihyperuricemic therapy and adequate hydration) to minimize risk; more intensive medical management (i.e., IV hydration, frequent monitoring, hospitalization) may be necessary as overall risk increases.1
If tumor lysis syndrome occurs, temporary interruption of therapy may be necessary;1 dosage reduction may be necessary in patients with CLL/SLL once therapy resumed.1
Neutropenia
Grade 3 or 4 neutropenia occurs commonly in patients receiving venetoclax as monotherapy or as a component of combination therapy.1 7 Baseline neutrophil count worsened in ≥95% of patients with AML receiving venetoclax in combination with azacitidine, decitabine, or low-dose cytarabine.1 Neutropenia may recur with subsequent cycles.1
Monitor CBC periodically during therapy.1 If hematologic toxicity occurs, temporary interruption of therapy or dosage modification may be required.1 Consider supportive therapy with hematopoietic growth factors (e.g., G-CSF) and/or anti-infective agents.1
Infectious Complications
Fatal and serious infections (e.g., pneumonia, sepsis) reported.1
Monitor for manifestations of infection and promptly initiate appropriate treatment.1 If grade 3 or 4 infection occurs, temporarily withhold therapy until resolution of infection; dosage reduction may be necessary.1 (See Tables 3 and 5 in Dosage and Administration.)
Immunization
Safety and efficacy of immunization with live, attenuated vaccines during or following venetoclax therapy not established.1 Immune response to vaccines may be reduced.1
Avoid immunization with live, attenuated vaccines prior to, during, and following therapy until recovery of B-cell counts.1
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm.1 Embryofetal toxicity (e.g., postimplantation loss, decreased fetal weight) demonstrated in animals; no evidence of teratogenicity.1
Avoid pregnancy during therapy.1 Perform pregnancy testing in females of reproductive potential prior to initiating therapy; such women should use effective contraception during therapy and for ≥30 days after drug is discontinued.1 If used during pregnancy or if patient becomes pregnant, apprise of potential fetal hazard.1
Treatment-related Mortality
Increased mortality reported in patients with multiple myeloma† [off-label] receiving venetoclax in combination with bortezomib and dexamethasone;1 13 14 venetoclax is not currently FDA-labeled for use in patients with multiple myeloma.1 13 Use of this combination for the treatment of multiple myeloma outside of a controlled clinical trial is not recommended.1
In a randomized, controlled phase 3 trial (BELLINI), risk of death was increased by 103% in patients with multiple myeloma receiving venetoclax in combination with bortezomib and dexamethasone compared with those receiving bortezomib and dexamethasone.13 This trial was terminated at FDA's request.13 May continue therapy with venetoclax in combination with bortezomib and dexamethasone in patients experiencing benefit from the drug only after the risks associated with use of the drug combination have been discussed and a new written informed consent has been obtained.13
Specific Populations
Pregnancy
No available data in pregnant women; however, animal data suggest that drug may cause fetal harm.1
Perform pregnancy testing prior to initiating treatment in females of reproductive potential.1
Lactation
Not known whether distributed into human milk or if drug has any effect on milk production or nursing infants.1 Present in milk of lactating animals.1 Discontinue nursing during therapy and for 1 week after final dose.1
Females and Males of Reproductive Potential.
May impair male fertility.1 Perform pregnancy testing prior to initiating treatment in females of reproductive potential.1 Advise females of childbearing potential to use effective contraception during treatment and for ≥30 days after drug is discontinued.1
Pediatric Use
Safety and efficacy not established.1
In a juvenile toxicology study in animals, clinical signs of venetoclax toxicity observed in mice receiving venetoclax from 7 to 60 days of age.1
Geriatric Use
CLL or SLL: No overall differences in safety and efficacy relative to younger patients.1
AML: Insufficient data in younger adults to determine whether they respond differently from geriatric patients.1
Hepatic Impairment
Principally eliminated by liver, but exposure not altered by mild or moderate hepatic impairment.1 Systemic exposure increased 2.7-fold in patients with severe hepatic impairment (Child-Pugh class C) compared with those with normal hepatic function.1
Renal Impairment
Systemic exposure not altered by mild, moderate, or severe renal impairment.1 Not evaluated in patients with end-stage renal disease or those requiring dialysis; not expected to be substantially removed by dialysis.1
Patients with reduced renal function (Clcr <80 mL/minute) are at increased risk for tumor lysis syndrome and require more intensive prophylaxis and monitoring during initiation of therapy.1
Common Adverse Effects
Monotherapy or in combination with obinutuzumab or rituximab in patients with CLL/SLL (≥20%): Neutropenia, thrombocytopenia, anemia, diarrhea, nausea, upper respiratory tract infection, cough, musculoskeletal pain, fatigue, edema.1
Combination therapy with azacitidine, decitabine, or low-dose cytarabine in patients with AML (≥30%): Nausea, diarrhea, thrombocytopenia, constipation, neutropenia, febrile neutropenia, fatigue, vomiting, edema, pyrexia, pneumonia, dyspnea, hemorrhage, anemia, rash, abdominal pain, sepsis, musculoskeletal pain, dizziness, cough, oropharyngeal pain, hypotension.1
Drug Interactions
Principally metabolized by CYP3A4/5.1 5
Weak inhibitor of CYP isoenzymes 2C8 and 2C9 and uridine diphosphate-glucuronosyltransferase (UGT) 1A1;1 however, not expected to be clinically relevant.1 15
In vitro, neither an inhibitor nor inducer of CYP isoenzymes 1A2, 2B6, 2C19, 2D6, or 3A4.1 4 Does not inhibit UGT1A4, 1A6, 1A9, or 2B7.1
Substrate and inhibitor of P-gp and breast cancer resistance protein (BCRP); weak inhibitor of organic anion transport protein (OATP) 1B1.1 4 Does not inhibit OATP1B3, organic cation transporter (OCT) 1, OCT2, renal organic anion transporter (OAT) 1, OAT3, multidrug and toxic compound extrusion (MATE) 1, and MATE2K.1
Drugs and Foods Affecting Hepatic Microsomal Enzymes
Potent or moderate CYP3A inhibitors: Possible increased peak plasma concentrations and AUC of venetoclax, and increased risk of tumor lysis syndrome and other toxicities.1 8 Concomitant use may be contraindicated or dosage modification may be necessary as described in Tables 4 and 6 in patients with CLL/SLL or AML, respectively. 1
Moderate or potent CYP3A inducers: Possible decreased peak plasma concentrations and AUC of venetoclax.1 Avoid concomitant use and consider an alternative agent with no or minimal enzyme induction potential.1
Drugs Affecting Efflux Transport Systems
Inhibitors of P-gp: Possible increased peak plasma concentrations and AUC of venetoclax; increased risk of toxicity.1 Reduce venetoclax dosage by at least 50% and monitor closely for signs of toxicity.1 When the P-gp inhibitor is discontinued, resume prior venetoclax dosage after 2–3 days.1
Substrates of Efflux Transport Systems
P-gp substrates: Possible increased peak plasma concentrations and AUC of P-gp substrate drugs.1 Avoid concomitant use of venetoclax with P-gp substrates.1 If such concomitant use cannot be avoided, administer substrate drug ≥6 hours prior to venetoclax.1
Drugs Affecting Gastric Acidity
Clinically important pharmacokinetic interactions not observed.1 8
Specific Drugs and Foods
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Antacids |
||
|
Azacitidine |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Azithromycin |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Cytarabine |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Decitabine |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Digoxin |
Increased digoxin peak plasma concentration and systemic exposure to digoxin due to P-gp inhibition by 35 and 9%, respectively1 |
Avoid concomitant use1 If concomitant use is necessary, administer digoxin ≥6 hours before venetoclax1 |
|
Grapefruit or grapefruit juice |
Possible increased venetoclax concentrations1 |
Avoid concomitant use1 |
|
Histamine H2-receptor antagonists |
||
|
Ketoconazole |
Increased venetoclax AUC (by 540%) and peak concentrations (by 130%)1 |
Concomitant use may be contraindicated or dosage modification may be necessary as described in Tables 4 and 6 in patients with CLL/SLL or AML, respectively1 |
|
Obinutuzumab |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Posaconazole |
Increased venetoclax AUC (by 90–144%) and peak concentrations (by 61–86%)1 |
Concomitant use may be contraindicated or dosage modification may be necessary as described in Tables 4 and 6 in patients with CLL/SLL or AML, respectively1 |
|
Proton-pump inhibitors |
||
|
Rifampin |
Decreased venetoclax AUC (by 71%) and peak concentrations (by 42%) with repeat dosing of rifampin1 5 Increased venetoclax AUC (by 78%) and peak concentrations (by 106%) with single-dose administration of rifampin1 5 |
Avoid concomitant use1 |
|
Ritonavir |
Increased venetoclax AUC (by 690%) and peak concentrations (by 140%)1 |
Concomitant use may be contraindicated or dosage modification may be necessary as described in Tables 4 and 6 in patients with CLL/SLL or AML, respectively1 |
|
Rituximab |
No substantial change to pharmacokinetics of venetoclax1 |
|
|
Seville oranges |
Possible increased venetoclax concentrations1 |
Avoid concomitant use1 |
|
Starfruit |
Possible increased venetoclax concentrations1 |
Avoid concomitant use1 |
|
Vaccines, inactivated |
Immune response to vaccines may be reduced1 |
|
|
Vaccines, live |
Immune response to vaccines may be reduced1 |
Avoid live vaccines1 |
|
Warfarin |
Increased warfarin AUC and peak concentrations by 18–28%1 |
Closely monitor INR1 |
Venetoclax Pharmacokinetics
Absorption
Bioavailability
Exhibits linear pharmacokinetics over the dose range of 150–800 mg.1 7
Following oral administration under fed conditions, peak plasma concentrations are attained in 5–8 hours.1 7
Food
Oral administration with a low-fat or high-fat meal increases AUC by 3.4- and 5.2-fold, respectively.1 6
Special Populations
In patients with mild or moderate hepatic impairment, systemic exposure similar to that in patients with normal hepatic function.1 In patients with severe hepatic impairment, systemic exposure increased 2.7-fold compared with patients with normal hepatic function.1
In patients with mild to severe renal impairment, systemic exposure similar to that in patients with normal renal function.1 Pharmacokinetics not studied in patients with end-stage renal disease or those requiring dialysis.1
Distribution
Extent
Not known whether distributed into milk.1
Plasma Protein Binding
>99%.1
Elimination
Metabolism
Metabolized principally by CYP3A4/5 to the major metabolite, M27.1
Elimination Route
Eliminated in feces (99.9%) and urine (<0.1%) within 9 days.1
Half-life
Mean terminal half-life approximately 26 hours.1 8
Special Populations
Age (range: 19–93 years), sex, and body weight do not substantially affect pharmacokinetics of venetoclax.1 8
No clinically important pharmacokinetic differences between White, Black, and Asian patients enrolled in clinical studies conducted in the US.1 Venetoclax exposure was 63% higher in Asian patients from Asian countries compared with non-Asian populations.1
Stability
Storage
Oral
Tablets
≤30°C.1
Store tablets in original starting pack packaging during initial 4 weeks of CLL/SLL therapy.1
Actions
-
Binds to BCL-2, displaces pro-apoptotic proteins (e.g., BIM), induces mitochondrial outer membrane permeabilization, and activates caspases resulting in restoration of intrinsic apoptotic pathway.1 9 10
-
Demonstrated cytotoxic activity in tumor cells overexpressing BCL-2.1
Advice to Patients
Advise patients to keep venetoclax in its original container, including the titration pack for CLL/SLL.1 Importance of taking venetoclax exactly as prescribed with food and water.1 Avoid grapefruit products, Seville oranges, and starfruit while taking the drug.1
Importance of advising patients to swallow venetoclax tablets whole and to not chew, crush, or break the tablets.1
If a dose is missed, importance of advising patients to take it as soon as they remember and resume the next dose at the regularly scheduled time unless the dose was missed by more than 8 hours, in which case they should not take the missed dose.1 If a dose is vomited, importance of administering the next dose at the regularly scheduled time; an additional dose should not be administered to make up for a missed dose.1
Risk of tumor lysis syndrome, particularly during initiation of therapy, initial dose escalation, and resumption of therapy following dosage interruption.1 Venetoclax may need to be administered in the hospital or medical office setting to allow monitoring for tumor lysis syndrome.1 Importance of maintaining scheduled appointments for blood work and other laboratory tests.1 Importance of immediately reporting any signs or symptoms of tumor lysis syndrome (e.g., fever, chills, nausea, vomiting, confusion, shortness of breath, seizure, arrhythmia, dark or cloudy urine, fatigue, muscle pain, joint discomfort).1 Importance of advising patients to maintain adequate hydration during venetoclax therapy.1 The recommended volume is 6–8 glasses (approximately 56 ounces) a day.1 Patients should start drinking water 2 days before initiating venetoclax, on the day of the first dose, and each time the dose is increased.1
Risk of neutropenia.1 Importance of monitoring complete blood cell (CBC) counts periodically during venetoclax therapy.1 Importance of immediately reporting any signs or symptoms of infection (e.g., fever).1
Risk of infection; importance of immediately reporting any signs or symptoms of infection (e.g., fever).1
Importance of avoiding vaccination with live vaccines prior to, during, and following venetoclax therapy until B-cell count recovery.1
Risk of fetal harm.1 Necessity of advising females of childbearing potential that they should use an effective method of contraception while receiving the drug and for at least 30 days after discontinuance of therapy.1 Importance of females informing clinicians if they are or plan to become pregnant.1 If pregnancy occurs, advise pregnant patients of potential risk to the fetus.1
Risk of male infertility.1
Importance of advising females to avoid breast-feeding while receiving venetoclax and for 1 week after the last dose.1
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.1
Importance of informing patients of other important precautionary information.1 (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Venetoclax can only be obtained through designated specialty pharmacies and distributors. Contact manufacturer for specific availability information.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
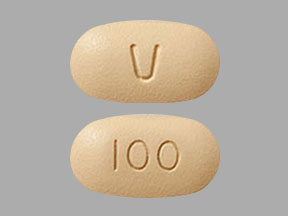
Tablets, film-coated |
10 mg |
Venclexta |
Genentech |
|
50 mg |
Venclexta |
Genentech |
||
|
100 mg |
Venclexta |
Genentech |
||
|
Titration Pack (CLL/SLL) |
14 Tablets, Venetoclax 10 mg (Venclexta) 7 Tablets, Venetoclax 50 mg (Venclexta) 7 Tablets, Venetoclax 100 mg (Venclexta) 14 Tablets, Venetoclax 100 mg (Venclexta) |
Venclexta Starting Pack (CLL/SLL) |
Genentech |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions October 13, 2022. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Genentech. Venclexta (venetoclax) tablets prescribing information. South San Francisco, CA; 2022 Jun.
2. Stilgenbauer S, Eichhorst B, Schetelig J et al. Venetoclax in relapsed or refractory chronic lymphocytic leukaemia with 17p deletion: a multicentre, open-label, phase 2 study. Lancet Oncol. 2016; 17:768-78. https://pubmed.ncbi.nlm.nih.gov/27178240
3. US Food and Drug Administration. Search orphan drug designations and approvals. From FDA website. Accessed 2022 Jul 18. http://www.accessdata.fda.gov/scripts/opdlisting/oopd/index.cfm
4. Weiss J, Gajek T, Köhler BC et al. Venetoclax (ABT-199) Might Act as a Perpetrator in Pharmacokinetic Drug-Drug Interactions. Pharmaceutics. 2016; 8(1):5.
5. Agarwal SK, Hu B, Chien D et al. Evaluation of Rifampin's Transporter Inhibitory and CYP3A Inductive Effects on the Pharmacokinetics of Venetoclax, a Bcl-2 Inhibitor: Results of a Single- and Multiple-dose Study. J Clin Pharmacol. 2016; 56(11):1335-43.
6. Salem AH, Agarwal S, Dunbar M et al. Effect of Low and High Fat Meals on the Pharmacokinetics of Venetoclax, a Selective First-in-Class Bcl-2 Inhibitor. J Clin Pharmacol. 2016; 56(11):1355-61.
7. Roberts AW, Davids MS, Pagel JM et al. Targeting BCL2 with Venetoclax in Relapsed Chronic Lymphocytic Leukemia. N Engl J Med. 2016; 374:311-22. https://pubmed.ncbi.nlm.nih.gov/26639348
8. Jones AK, Freise KJ, Agarwal SK et al. Clinical Predictors of Venetoclax Pharmacokinetics in Chronic Lymphocytic Leukemia and Non-Hodgkin's Lymphoma Patients: a Pooled Population Pharmacokinetic Analysis. AAPS J. 2016; 18(5):1192-1202. https://pubmed.ncbi.nlm.nih.gov/27233802
9. Anderson MA, Deng J, Seymour JF et al. The BCL2 selective inhibitor venetoclax induces rapid onset apoptosis of CLL cells in patients via a TP53 independent mechanism. Blood. 2016; 127(25):3215-24. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4920022/
10. Ng SY, Davids MS. Selective Bcl-2 inhibition to treat chronic lymphocytic leukemia and non-Hodgkin lymphoma. Clin Adv Hematol Oncol. 2014; 12:224-9. https://pubmed.ncbi.nlm.nih.gov/25003352
11. Jones J, Mato A, Coutre S et al. Preliminary results of a phase 2, open-label study of venetoclax (ABT-199/GDC-0199) monotherapy in patients with chronic lymphocytic leukemia relapsed after or refractory to ibrutinib or idelalisib therapy. Oral presentation at 57th Annual Meeting of the American Society of Hematology. Orlando, FL: 2015 Dec 7.
12. US Food and Drug Administration. Medical review(s)/statistical review(s): NDA 208573Orig1S000. From FDA website. http://www.accessdata.fda.gov/drugsatfda_docs/nda/2016/208573Orig1s000MedR.pdf
13. US Food and Drug Administration. FDA warns about the risks associated with the investigational use of Venclexta in multiple myeloma. Silver Spring, MD; 2019 Mar 21. From the FDA website. https://www.fda.gov/drugs/drug-safety-and-availability/fda-warns-about-risks-associated-investigational-use-venclexta-multiple-myeloma
14. Kumar S. A phase 3 study of venetoclax or placebo in combination with bortezomib and dexamethasone in patients with relapsed/refractory multiple myeloma. Oral presentation at 24th Annual Congress of the European Hematology Association. Amsterdam, Netherlands: 2019 Jun 16.
15. Genentech. Venclexta (venetoclax) tablets prescribing information. South San Francisco, CA; 2016 Apr.
16. Fischer K, Al-Sawaf O, Bahlo J et al. Venetoclax and Obinutuzumab in Patients with CLL and Coexisting Conditions. N Engl J Med. 2019; 380:2225-2236. https://pubmed.ncbi.nlm.nih.gov/31166681
17. Al-Sawaf O, Zhang C, Tandon M et al. Venetoclax plus obinutuzumab versus chlorambucil plus obinutuzumab for previously untreated chronic lymphocytic leukaemia (CLL14): follow-up results from a multicentre, open-label, randomised, phase 3 trial. Lancet Oncol. 2020; 21:1188-1200. https://pubmed.ncbi.nlm.nih.gov/32888452
18. Seymour JF, Kipps TJ, Eichhorst B et al. Venetoclax-Rituximab in Relapsed or Refractory Chronic Lymphocytic Leukemia. N Engl J Med. 2018; 378:1107-1120. https://pubmed.ncbi.nlm.nih.gov/29562156
19. Kater AP, Seymour JF, Hillmen P et al. Fixed Duration of Venetoclax-Rituximab in Relapsed/Refractory Chronic Lymphocytic Leukemia Eradicates Minimal Residual Disease and Prolongs Survival: Post-Treatment Follow-Up of the MURANO Phase III Study. J Clin Oncol. 2019; 37:269-277. https://pubmed.ncbi.nlm.nih.gov/30523712
20. Kater AP, Wu JQ, Kipps T et al. Venetoclax Plus Rituximab in Relapsed Chronic Lymphocytic Leukemia: 4-Year Results and Evaluation of Impact of Genomic Complexity and Gene Mutations From the MURANO Phase III Study. J Clin Oncol. 2020; 38:4042-4054. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7768340/ https://pubmed.ncbi.nlm.nih.gov/32986498
21. Roberts AW, Davids MS, Pagel JM et al. Targeting BCL2 with Venetoclax in Relapsed Chronic Lymphocytic Leukemia. N Engl J Med. 2016; 374:311-22. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7107002/ https://pubmed.ncbi.nlm.nih.gov/26639348
22. Jones JA, Mato AR, Wierda WG et al. Venetoclax for chronic lymphocytic leukaemia progressing after ibrutinib: an interim analysis of a multicentre, open-label, phase 2 trial. Lancet Oncol. 2018; 19:65-75. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6027999/ https://pubmed.ncbi.nlm.nih.gov/29246803
23. Coutre S, Choi M, Furman RR et al. Venetoclax for patients with chronic lymphocytic leukemia who progressed during or after idelalisib therapy. Blood. 2018; 131:1704-1711. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC5922273/ https://pubmed.ncbi.nlm.nih.gov/29305552
24. DiNardo CD, Jonas BA, Pullarkat V et al. Azacitidine and Venetoclax in Previously Untreated Acute Myeloid Leukemia. N Engl J Med. 2020; 383:617-629. https://pubmed.ncbi.nlm.nih.gov/32786187
25. DiNardo CD, Pratz K, Pullarkat V et al. Venetoclax combined with decitabine or azacitidine in treatment-naive, elderly patients with acute myeloid leukemia. Blood. 2019; 133:7-17. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6318429/ https://pubmed.ncbi.nlm.nih.gov/30361262
26. DiNardo CD, Pratz KW, Letai A et al. Safety and preliminary efficacy of venetoclax with decitabine or azacitidine in elderly patients with previously untreated acute myeloid leukaemia: a non-randomised, open-label, phase 1b study. Lancet Oncol. 2018; 19:216-228. https://pubmed.ncbi.nlm.nih.gov/29339097
27. Pollyea DA, Pratz K, Letai A et al. Venetoclax with azacitidine or decitabine in patients with newly diagnosed acute myeloid leukemia: Long term follow-up from a phase 1b study. Am J Hematol. 2021; 96:208-217. https://pubmed.ncbi.nlm.nih.gov/33119898
28. Wei AH, Montesinos P, Ivanov V et al. Venetoclax plus LDAC for newly diagnosed AML ineligible for intensive chemotherapy: a phase 3 randomized placebo-controlled trial. Blood. 2020; 135:2137-2145. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC7290090/ https://pubmed.ncbi.nlm.nih.gov/32219442
29. Wei AH, Strickland SA Jr, Hou JZ et al. Venetoclax Combined With Low-Dose Cytarabine for Previously Untreated Patients With Acute Myeloid Leukemia: Results From a Phase Ib/II Study. J Clin Oncol. 2019; 37:1277-1284. https://www.ncbi.nlm.nih.gov/pmc/articles/PMCPMC6524989/ https://pubmed.ncbi.nlm.nih.gov/30892988
30. Wei AH, Panayiotidis P, Montesinos P, et al. 6-month follow-up of VIALE-C demonstrates improved and durable efficacy in patients with untreated AML ineligible for intensive chemotherapy. Blood Cancer J. 2021;11(10):163.
2000. National Cancer Institute. Chronic Lymphocytic Leukemia Treatment (PDQ)–Health Professional Version. From NIH website. Accessed 2022 Jul 19. https://www.cancer.gov/types/leukemia/hp/cll-treatment-pdq/types/leukemia/hp/cll-treatment-pdq
2001. Eichhorst B, Robak T, Montserrat E, et al. Chronic lymphocytic leukaemia: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2021;32(1):23-33.
3015. National Cancer Institute. Acute Myeloid Leukemia Treatment (PDQ)–Health Professional Version. From NIH website. Accessed 2022, Jul 19. https://www.cancer.gov/types/leukemia/hp/adult-aml-treatment-pdq/types/leukemia/hp/adult-aml-treatment-pdq.
3016. Sekeres MA, Guyatt G, Abel G, et al. American Society of Hematology 2020 guidelines for treating newly diagnosed acute myeloid leukemia in older adults. Blood Adv. 2020 11;4(15):3528-3549.
Related/similar drugs
Rituxan
Rituxan infusion is used to treat certain leukemias and lymphomas and some non-cancer conditions ...
Kesimpta
Kesimpta is used to treat relapsing forms of multiple sclerosis (MS), including clinically isolated ...
Imbruvica
Imbruvica (ibrutinib) is used to treat chronic lymphocytic leukemia (CLL), small lymphocytic ...
Brukinsa
Brukinsa is used to treat adults with mantle cell lymphoma, Waldenström’s macroglobulinemia, ma ...
Calquence
Calquence (acalabrutinib) is used to treat chronic lymphocytic leukemia (CLL), and mantle cell ...
Venclexta
Venclexta may be used to treat chronic lymphocytic leukemia (CLL), small lymphocytic lymphoma ...
Acalabrutinib
Acalabrutinib (Calquence) is used to treat chronic lymphocytic leukemia (CLL), and mantle cell ...
Ibrutinib
Ibrutinib (Imbruvica) is a Bruton's tyrosine kinase inhibitor used for certain blood cancers and ...
Cyclophosphamide
Cyclophosphamide is used for acute lymphocytic leukemia, acute nonlymphocytic leukemia, brain ...
Frequently asked questions
- Is Venclexta (venetoclax) chemotherapy?
- How effective is Venclexta?
- How long do you take Venclexta for?
- Can Venclexta be used for Multiple Myeloma?
- How is Venclexta (venetoclax) used for AML?
- How does Venclexta work?
More about venetoclax
- Check interactions
- Compare alternatives
- Reviews (23)
- Side effects
- Dosage information
- During pregnancy
- Drug class: miscellaneous antineoplastics
- Breastfeeding
- En español