Ubrogepant (Monograph)
Brand name: Ubrelvy
Drug class: Calcitonin Gene-related Peptide (CGRP) Antagonists
Introduction
Antimigraine agent; small molecule calcitonin gene-related peptide (CGRP) receptor antagonist (gepant).
Uses for Ubrogepant
Acute Treatment of Migraine
Acute treatment of migraine with or without aura in adults.
In the short-term ACHIEVE clinical studies, ubrogepant was substantially more effective than placebo in relieving migraine pain and the patient's self-identified most bothersome symptom (e.g., photophobia, phonophobia, nausea) at 2 hours post-dose. Efficacy was maintained during long-term intermittent use in a 1-year, randomized, open-label extension trial.
The American Headache Society (AHS) guidelines include the oral CGRP antagonists (gepants) as one of several drugs with established efficacy in the acute treatment of migraine. Unlike 5-HT1 receptor agonists (triptans) and ergot alkaloids, CGRP antagonists do not cause constriction of blood vessels, and therefore may have a role in patients with cardiovascular contraindications to triptans. Because of the relatively high cost of CGRP antagonists compared with oral triptans in the acute treatment of migraine, AHS recommends that oral CGRP antagonists be considered for use only in patients who have contraindications to triptans and/or who have an inadequate response or intolerance to at least 2 oral triptans.
Not indicated for the preventive treatment of migraine.
Ubrogepant Dosage and Administration
General
Patient Monitoring
-
Monitor patients for new-onset hypertension, or worsening of pre-existing hypertension.
-
Monitor patients with a history of Raynaud's phenomenon for worsening or recurrence of signs and symptoms.
Administration
Oral Administration
Administer tablets orally without regard to food.
Dosage
Adults
Acute Treatment of Migraine
Oral
Initially, 50 or 100 mg orally as a single dose. If needed, may administer a second dose at least 2 hours after the first dose. In a long-term (1-year) study, approximately one-third of patients required a second dose.
Dosage adjustments recommended with concomitant use of moderate or weak CYP3A4 inhibitors or inducers, breast cancer resistance protein (BCRP) inhibitors, and/or P-glycoprotein (P-gp) only inhibitors. Avoid concomitant use of potent CYP3A4 inhibitors or potent CYP3A4 inducers.
Special Populations
Hepatic Impairment
Mild (Child-Pugh class A) or moderate (Child-Pugh class B) hepatic impairment: Dosage adjustment not necessary.
Severe hepatic impairment (Child-Pugh class C): Manufacturer recommends initial single dose of 50 mg; if needed, may administer second 50-mg dose after at least 2 hours.
Renal Impairment
Mild or moderate renal impairment (Clcr 30–89 mL/minute): Dosage adjustment not necessary.
Severe renal impairment (Clcr 15–29 mL/minute): Manufacturer recommends initial single dose of 50 mg; if needed, may administer a second 50-mg dose after at least 2 hours.
End-stage renal disease (Clcr <15 mL/minute): Avoid use.
Geriatric Patients
Select dosage carefully, usually starting at the low end of the dosage range.
Cautions for Ubrogepant
Contraindications
-
Concomitant use of potent CYP3A4 inhibitors.
-
History of serious hypersensitivity to ubrogepant or any of its components.
Warnings/Precautions
Hypersensitivity Reactions
Hypersensitivity reactions including anaphylaxis, dyspnea, facial or throat edema, rash, urticaria, and pruritus reported. Reactions may occur minutes to days after administration. Majority of reactions were not serious and occurred within hours after administration. Some reactions led to treatment discontinuation. If serious hypersensitivity reaction occurs, discontinue ubrogepant and initiate appropriate therapy.
Hypertension
In postmarketing, hypertension development and worsening of pre-existing hypertension reported. Some cases required initiation of pharmacological treatment for hypertension and/or hospitalization; discontinuation of ubrogepant occurred in many cases. Hypertension may develop at any time during treatment, but was most frequently reported within 7 days of therapy initiation. Monitor patients for new-onset hypertension, or worsening of pre-existing hypertension. Discontinuation may be warranted if an alternative etiology for hypertension is not identified or blood pressure is inadequately controlled.
Raynaud's Phenomenon
In postmarketing, Raynaud’s phenomenon development and recurrence or worsening of pre-existing Raynaud’s phenomenon reported. Symptom onset occurred a median of 1.5 days following dosing. Many cases involved serious outcomes, including hospitalizations and disability, generally related to debilitating pain. Discontinuation of therapy resulted in symptom resolution in most cases. Discontinue therapy if signs or symptoms of Raynaud’s phenomenon develop, and evaluate patients if symptoms do not resolve. Monitor patients with a history of Raynaud’s phenomenon for, and inform about the possibility of, worsening or recurrence of signs and symptoms.
Specific Populations
Pregnancy
No adequate data to date on the developmental risk associated with use of ubrogepant in pregnant women. Based on animal studies, may cause fetal harm. In animal studies, adverse effects on embryofetal development (increased embryofetal mortality, decreased body weight of offspring) observed at dosages higher than those used clinically and that were associated with maternal toxicity.
Estimated rates of major birth defects and miscarriage among deliveries to women with migraine (2.2–2.9 and 17%, respectively) are similar to rates reported in women without migraine. Possible increased risk of preeclampsia and gestational hypertension during pregnancy in women with migraine.
Patients may enroll in a registry that monitors outcomes during pregnancy by calling 833-277-0206 or visiting [Web]
Lactation
Not known whether distributed into human milk; distributed into milk in rats in concentrations comparable to peak plasma concentrations. Effects on the breast-fed infant and on milk production also unknown. Consider developmental and health benefits of breast-feeding, mother's clinical need for ubrogepant, and potential adverse effects on the breast-fed infant from the drug or underlying maternal condition.
Pediatric Use
Safety and efficacy not established in pediatric patients.
Geriatric Use
Insufficient experience in patients ≥65 years of age to determine whether geriatric patients respond differently than younger adults. Clinically important pharmacokinetic differences not observed between geriatric and younger individuals.
Select dosage with caution, usually starting at the low end of the dosage range.
Hepatic Impairment
Exposure is increased in patients with hepatic impairment.
Dosage adjustment not necessary in patients with mild (Child-Pugh class A) or moderate hepatic impairment (Child-Pugh class B). In patients with severe (Child-Pugh class C) hepatic impairment, manufacturer recommends an initial dose of 50 mg followed by a second 50-mg dose after at least 2 hours, if needed.
Renal Impairment
Pharmacokinetics not substantially affected in patients with mild or moderate renal impairment (Clcr 30–89 mL/minute); dosage adjustment not necessary.
Not studied in patients with severe renal impairment (Clcr 15–29 mL/minute). Based on its pharmacokinetic profile and a conservative estimate that severe renal impairment is unlikely to cause more than a twofold increase in exposure to ubrogepant, manufacturer recommends an initial dose of 50 mg followed by a second 50-mg dose after at least 2 hours, if needed, in patients with severe renal impairment.
Avoid use in patients with end-stage renal disease (Clcr <15 mL/minute).
Common Adverse Effects
Nausea, somnolence (including sedation and fatigue), dry mouth.
Drug Interactions
Metabolized principally by CYP3A4. Substrate of BCRP and P-gp and a weak substrate of organic anion transporting polypeptide (OATP) 1B1 and 1B3 and organic anion transporter (OAT) 1, but not a substrate of OAT3.
Weak inhibitor of CYP isoenzymes 2C8, 2C9, 2D6, and 2C19; monoamine oxidase-A (MAO-A); and UGT1A1 in vitro; not expected to be clinically important. Weak inhibitor of OATP1B1, OATP1B3, and organic cation transporter (OCT) 2.
Does not inhibit CYP isoenzymes 1A2, 2B6, or 3A4; does not induce CYP isoenzymes 1A2, 2B6, or 3A4 at clinically relevant concentrations. Does not inhibit P-gp, BCRP, bile salt export pump (BSEP), multidrug resistance-associated protein (MRP) 3 or 4, OAT1, OAT3, or sodium taurocholate cotransporting polypeptide (NTCP).
Drugs Affecting Hepatic Microsomal Enzymes
CYP3A4 inhibitors: Concomitant use of ubrogepant and CYP3A4 inhibitors may result in increased systemic exposure to ubrogepant. Specific studies with known moderate or potent inhibitors of CYP3A4 indicate magnitude of increase may be substantial with concurrent use of these drugs.
Weak CYP3A4 inhibitors: No dedicated drug interaction study has been conducted with concomitant use of ubrogepant and weak CYP3A4 inhibitors. If used concomitantly with a weak CYP3A4 inhibitor, recommended dosage is a single 50-mg dose initially followed by a second 50-mg dose, if needed, after at least 2 hours.
Moderate CYP3A4 inhibitors: If used concomitantly with a moderate CYP3A4 inhibitor, recommended dosage is a 50-mg dose initially; avoid taking a second dose within 24 hours of initial dose.
Potent CYP3A4 inhibitors: Avoid concomitant use of potent CYP3A4 inhibitors.
Potent CYP3A4 inducers: Concomitant use of ubrogepant and potentCYP3A4 inducers may result in decreased systemic exposure and efficacy of ubrogepant. Avoid concomitant use with potent CYP3A4 inducers.
Weak or moderate CYP3A4 inducers: Because of potential for decreased ubrogepant exposure in patients receiving a weak or moderate CYP3A4 inducer, recommended dosage is a single 100-mg dose initially followed by a second 100-mg dose after at least 2 hours, if needed.
BCRP and/or P-gp Only Inhibitors
Based on clinical interaction studies with drugs that are dual inhibitors of CYP3A4 and P-gp, concomitant use of ubrogepant and BCRP or P-gp only inhibitors may result in increased systemic exposure of ubrogepant. Highest predicted potential increase in ubrogepant exposure not expected to be more than twofold.
In patients receiving P-gp only inhibitors and/or BCRP inhibitors, recommended dosage is an initial single 50-mg dose followed by a second 50-mg dose after at least 2 hours, if needed.
Specific Drugs and Food
|
Drug or Food |
Interaction |
Comments |
|---|---|---|
|
Acetaminophen |
No clinically important pharmacokinetic interactions observed |
|
|
Antifungals, azole (fluconazole, itraconazole, ketoconazole) |
Possible increased systemic exposure to ubrogepant Fluconazole (moderate CYP3A4 inhibitor): Possible increased systemic exposure to ubrogepant Ketoconazole (potent CYP3A4 inhibitor): Increased peak plasma concentration and exposure to ubrogepant 5.3- and 9.7-fold, respectively |
Fluconazole: Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose Itraconazole, ketoconazole: Avoid concomitant use |
|
Atogepant |
No clinically important pharmacokinetic interactions observed |
|
|
Barbiturates (e.g., phenobarbital) |
Barbiturates (potent CYP3A4 inducers): Possible decreased exposure and loss of efficacy of ubrogepant |
Avoid concomitant use |
|
Carvedilol |
Possible increased systemic exposure to ubrogepant (not expected to exceed twofold) |
Administer initial single 50-mg dose of ubrogepant followed by a second 50-mg dose after 2 hours, if needed |
|
Ciprofloxacin |
Possible increased systemic exposure to ubrogepant |
Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose |
|
Clarithromycin |
Possible increased systemic exposure to ubrogepant |
Avoid concomitant use |
|
Curcumin |
Possible increased systemic exposure to ubrogepant (not expected to exceed twofold) |
Administer initial single 50-mg dose of ubrogepant followed by a second 50-mg dose after 2 hours, if needed |
|
Cyclosporine |
Possible increased systemic exposure to ubrogepant |
Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose |
|
Eltrombopag |
Possible increased systemic exposure to ubrogepant (not expected to exceed twofold) |
Administer initial single 50-mg dose of ubrogepant followed by a second 50-mg dose after 2 hours, if needed |
|
Erenumab |
No clinically important pharmacokinetic interactions observed |
|
|
Esomeprazole |
No clinically important pharmacokinetic interactions observed |
|
|
Fluvoxamine |
Possible increased systemic exposure to ubrogepant |
Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose |
|
Galcanezumab |
No clinically important pharmacokinetic interactions observed |
|
|
Grapefruit or grapefruit juice |
Possible increased systemic exposure to ubrogepant with consumption of grapefruit (moderate CYP3A4 inhibitor) |
Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose if grapefruit or grapefruit juice is consumed |
|
Naproxen |
No clinically important pharmacokinetic interactions observed |
|
|
Oral contraceptives |
No clinically important pharmacokinetic interactions observed with oral contraceptive containing norgestimate and ethinyl estradiol |
|
|
Phenytoin |
Phenytoin (potent CYP3A4 inducer): Possible decreased exposure and loss of efficacy of ubrogepant |
Avoid concomitant use |
|
Quinidine |
Possible increased systemic exposure to ubrogepant (not expected to exceed twofold) |
Administer initial single 50-mg dose of ubrogepant followed by a second 50-mg dose after 2 hours, if needed |
|
Rifampin |
Rifampin (potent CYP3A4 and P-gp inducer): Substantially decreased peak plasma concentration and exposure to ubrogepant (by approximately 70 and 80%, respectively); potential for loss of efficacy of ubrogepant |
Avoid concomitant use |
|
St. John's wort (Hypericum perforatum) |
St. John's wort (potent CYP3A4 inducer): Possible decreased exposure and loss of efficacy of ubrogepant |
Avoid concomitant use |
|
Sumatriptan |
Slight alterations in ubrogepant and sumatriptan pharmacokinetics observed in a phase 1 study; unlikely to be clinically important Concurrent administration well tolerated in healthy individuals in a phase 1 study; combined use of ubrogepant and 5-HT1 receptor agonists (triptans) well tolerated in patients with migraine in the ACHIEVE clinical trials |
|
|
Verapamil |
Verapamil (moderate CYP3A4 inhibitor) increased peak plasma concentrations and exposure of ubrogepant 2.8- and 3.5-fold, respectively |
Administer initial single 50-mg dose of ubrogepant; avoid taking a second dose within 24 hours of initial dose |
Ubrogepant Pharmacokinetics
Absorption
Bioavailability
Exhibits dose-proportional pharmacokinetics within the recommended dosage range.
Rapidly absorbed; peak plasma concentrations occur approximately 1.5 hours following oral administration.
Food
High-fat meal delays time to peak plasma concentration by 2 hours and decreases peak concentration by 22%, but does not affect systemic exposure to the drug.
Special Populations
Mild hepatic impairment (Child-Pugh class A): Exposure increased by 7%.
Moderate hepatic impairment (Child-Pugh class B): Exposure increased by 50%.
Severe hepatic impairment (Child-Pugh class C): Exposure increased by 115%.
Mild or moderate renal impairment (Clcr 30–89 mL/minute): Pharmacokinetics not substantially affected.
Severe renal impairment (Clcr 15–29 mL/minute): Not studied; unlikely to cause more than a twofold increase in exposure to ubrogepant.
End-stage renal disease (Clcr <15 mL/minute): Not studied.
Age, sex, race, and body weight do not substantially affect pharmacokinetics.
Distribution
Extent
Not known whether distributed into human milk; distributed into milk in rats at concentrations comparable to peak plasma concentrations.
Plasma Protein Binding
87%.
Elimination
Metabolism
Eliminated mainly through metabolism, primarily by CYP3A4. Parent compound (ubrogepant) and 2 glucuronide conjugate metabolites are most prevalent circulating components in human plasma; the glucuronide metabolites are not expected to contribute to pharmacologic activity.
Elimination Route
Excreted mainly by the biliary/fecal route; renal route is a minor route of elimination. Following a single oral dose, eliminated in feces (42%) and urine (6%) as unchanged drug.
Half-life
Approximately 5–7 hours.
Stability
Storage
Oral
Tablets
20–25°C (may be exposed to 15–30°C).
Actions
-
Small molecule calcitonin gene-related peptide (CGRP) receptor antagonist (sometimes referred to as a gepant); binds to CGRP receptors with high affinity, blocking the binding of CGRP to the receptor and preventing subsequent receptor activation.
-
CGRP is a potent vasodilator and pain-signaling neuropeptide that has been associated with migraine pathophysiology. CGRP and its receptors are located at sites that are relevant to migraine development such as the trigeminal neurons and are also widely distributed throughout the central and peripheral nervous systems as well as in nonneuronal tissues throughout the body.
-
Increased serum CGRP concentrations observed in individuals during acute migraine attacks; these return to normal after resolution of the migraine. IV infusion of CGRP induces migraines in patients with a history of migraines.
-
Unlike 5-HT1 receptor agonists (triptans) and ergot alkaloids, ubrogepant does not appear to cause vasoconstriction. Also does not appear to prolong the QT interval in dosages up to twice the maximum recommended daily dosage.
Advice to Patients
-
Advise patients to read the manufacturer's patient information.
-
Inform patients about the signs and symptoms of hypersensitivity reactions. Advise patients to discontinue ubrogepant and seek immediate medical attention if a hypersensitivity reaction occurs.
-
Inform patients that high blood pressure can develop, or pre-existing high blood pressure can worsen, with therapy. Advise patients to contact their clinician if increases in blood pressure occur.
-
Inform patients that Raynaud's phenomenon can develop or worsen with therapy. Advise patients to discontinue therapy and contact their clinician if signs or symptoms of Raynaud's phenomenon occur.
-
Inform patients that ubrogepant may interact with certain other drugs. Advise patients to inform their clinician about concomitant use of any prescription and OTC drugs and dietary or herbal supplements (e.g., curcumin, St. John's wort) as well as any concomitant illnesses (e.g., hepatic or renal disease). Importance of advising patients to inform their clinician of grapefruit or grapefruit juice consumption because dosage adjustment is recommended during concurrent use.
-
Advise patients to inform clinicians if they are or plan to become pregnant or are breast-feeding or plan to breast-feed.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
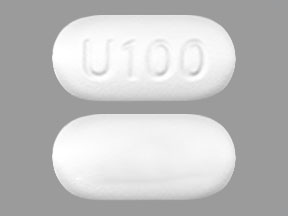
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets |
50 mg |
Ubrelvy |
Abbvie |
|
100 mg |
Ubrelvy |
Abbvie |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions June 10, 2025. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
- What are the newest migraine medications in 2025?
- Ubrelvy vs Imitrex (sumatriptan): How do they compare?
- What is the mechanism of action for Ubrelvy?
- Is Ubrelvy a narcotic used for migraine?
- What is Ubrelvy used for and how fast does Ubrelvy work?
- Ubrelvy Coupon Card: Do I Qualify, How Much Can I Save?
- Ubrelvy vs Emgality: How do they compare for migraines?
- How do you take Ubrelvy tablets?
More about ubrogepant
- Check interactions
- Compare alternatives
- Reviews (287)
- Side effects
- Dosage information
- During pregnancy
- Drug class: CGRP inhibitors
- Breastfeeding
- En español