Triamterene (Monograph)
Brand name: Dyrenium
Drug class: Potassium-sparing Diuretics
Triamterene (Systemic) is also contained as an ingredient in the following combinations:
Triamterene and Hydrochlorothiazide
Warning
-
Hyperkalemia (i.e., serum potassium concentrations ≥5.5 mEq/L) may occur with all potassium-sparing agents, including triamterene.b c d More likely to occur in patients with renal impairment and diabetes (even without evidence of renal impairment), and in geriatric or severely ill patients or those receiving prolonged therapy with large doses.a b c d
-
Uncorrected hyperkalemia may be fatal; monitor serum potassium concentrations at frequent intervals especially during initial therapy, after dosage adjustment, or in patients with concurrent illness that may affect renal function.b c d
Introduction
Potassium-sparing diuretic; pteridine derivative.b
Uses for Triamterene
Edema
Management of edema associated with heart failure, cirrhosis of the liver, or nephrotic syndrome.b
Management of steroid-induced edema, idiopathic edema, and edema caused by secondary hyperaldosteronism.b
May be used alone but most valuable when used in combination with other diuretics to promote diuresis and/or decrease potassium excretion caused by kaliuretic diuretics.b
May be particularly useful in patients excreting excessive amounts of potassium (especially those who cannot tolerate potassium supplements) and for those in whom potassium loss could be detrimental, such as patients receiving digitalis glycosides or those with myasthenia gravis.a b
Promotes increased diuresis in patients resistant or only partially responsive to thiazides or other diuretics because of secondary hyperaldosteronism.b
May be effective in some patients unresponsive to spironolactone; unlike spironolactone, diuretic effect of triamterene is independent of aldosterone concentrations.a
Used in fixed combination with hydrochlorothiazide for treatment of edema in patients who require a thiazide diuretic and in whom the development of hypokalemia cannot be risked and in patients who develop hypokalemia during hydrochlorothiazide monotherapy.c d
Do not use for routine therapy in pregnant women with mild edema who are otherwise healthy.b c d
Heart Failure
In the management of edema associated with heart failure, generally used in conjunction with other more effective, rapidly acting diuretics (e.g., thiazides, chlorthalidone, loop diuretics).a Some patients resistant to triamterene monotherapy may respond to such combined therapy.a
Most experts state that all patients with symptomatic heart failure who have evidence for, or a history of, fluid retention generally should receive diuretic therapy in conjunction with moderate sodium restriction, an agent to inhibit the renin-angiotensin-aldosterone (RAA) system (e.g., ACE inhibitor, angiotensin II receptor antagonist, angiotensin receptor-neprilysin inhibitor [ARNI]), a β-adrenergic blocking agent (β-blocker), and in selected patients, an aldosterone antagonist.524 700 713
Most experts state that the diuretics of choice for most patients with heart failure are loop diuretics (e.g., bumetanide, ethacrynic acid, furosemide, torsemide).a
Hypertension
Has been used alone or in combination with other classes of antihypertensive agents in the management of hypertension† [off-label];a however, other agents (i.e., ACE inhibitors, angiotensin II receptor antagonists, calcium-channel blockers, thiazide diuretics) are preferred for initial management according to current evidence-based practice guidelines for the management of hypertension in adults.501 502 503 504 1200 f
Triamterene alone has little if any hypotensive effect, but may be used with another diuretic (e.g., hydrochlorothiazide) or antihypertensive agent in the management of mild to moderate hypertension.a Used principally in patients with diuretic-induced hypokalemia or to prevent hypokalemia in patients receiving diuretics who are at risk of this adverse effect.a
Used in fixed combination with hydrochlorothiazide for treatment of hypertension in patients who require a thiazide diuretic and in whom the development of hypokalemia cannot be risked and in patients who develop hypokalemia during hydrochlorothiazide monotherapy.c d
Triamterene/hydrochlorothiazide fixed combination may be used as an adjunct to other antihypertensive drugs (e.g., β-blockers).c d
Individualize choice of therapy; consider patient characteristics (e.g., age, ethnicity/race, comorbidities, cardiovascular risk) as well as drug-related factors (e.g., ease of administration, availability, adverse effects, cost).501 502 503 504 515 1200 1201
A 2017 ACC/AHA multidisciplinary hypertension guideline classifies BP in adults into 4 categories: normal, elevated, stage 1 hypertension, and stage 2 hypertension.1200 (See Table 1.)
Source: Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018;71:e13-115.
Individuals with SBP and DBP in 2 different categories (e.g., elevated SBP and normal DBP) should be designated as being in the higher BP category (i.e., elevated BP).
|
Category |
SBP (mm Hg) |
DBP (mm Hg) |
|
|---|---|---|---|
|
Normal |
<120 |
and |
<80 |
|
Elevated |
120–129 |
and |
<80 |
|
Hypertension, Stage 1 |
130–139 |
or |
80–89 |
|
Hypertension, Stage 2 |
≥140 |
or |
≥90 |
The goal of hypertension management and prevention is to achieve and maintain optimal control of BP.1200 However, the BP thresholds used to define hypertension, the optimum BP threshold at which to initiate antihypertensive drug therapy, and the ideal target BP values remain controversial.501 503 504 505 506 507 508 515 523 526 530 1200 1201 1207 1209 1222 1223 1229
The 2017 ACC/AHA hypertension guideline generally recommends a target BP goal (i.e., BP to achieve with drug therapy and/or nonpharmacologic intervention) of <130/80 mm Hg in all adults regardless of comorbidities or level of atherosclerotic cardiovascular disease (ASCVD) risk.1200 In addition, an SBP goal of <130 mm Hg generally is recommended for noninstitutionalized ambulatory patients ≥65 years of age with an average SBP of ≥130 mm Hg.1200 These BP goals are based upon clinical studies demonstrating continuing reduction of cardiovascular risk at progressively lower levels of SBP.1200 1202 1210
Other hypertension guidelines generally have based target BP goals on age and comorbidities.501 504 536 Guidelines such as those issued by the JNC 8 expert panel generally have targeted a BP goal of <140/90 mm Hg regardless of cardiovascular risk, and have used higher BP thresholds and target BPs in elderly patients501 504 536 compared with those recommended by the 2017 ACC/AHA hypertension guideline.1200
Some clinicians continue to support previous target BPs recommended by JNC 8 due to concerns about the lack of generalizability of data from some clinical trials (e.g., SPRINT study) used to support the 2017 ACC/AHA hypertension guideline and potential harms (e.g., adverse drug effects, costs of therapy) versus benefits of BP lowering in patients at lower risk of cardiovascular disease.1222 1223 1224 1229
Consider potential benefits of hypertension management and drug cost, adverse effects, and risks associated with the use of multiple antihypertensive drugs when deciding a patient's BP treatment goal.1200 1220 1229
For decisions regarding when to initiate drug therapy (BP threshold), the 2017 ACC/AHA hypertension guideline incorporates underlying cardiovascular risk factors.1200 1207 ASCVD risk assessment is recommended by ACC/AHA for all adults with hypertension.1200
ACC/AHA currently recommend initiation of antihypertensive drug therapy in addition to lifestyle/behavioral modifications at an SBP ≥140 mm Hg or DBP ≥90 mm Hg in adults who have no history of cardiovascular disease (i.e., primary prevention) and a low ASCVD risk (10-year risk <10%).1200
For secondary prevention in adults with known cardiovascular disease or for primary prevention in those at higher risk for ASCVD (10-year risk ≥10%), ACC/AHA recommend initiation of antihypertensive drug therapy at an average SBP ≥130 mm Hg or an average DBP ≥80 mm Hg.1200
Adults with hypertension and diabetes mellitus, CKD, or age ≥65 years are assumed to be at high risk for cardiovascular disease; ACC/AHA state that such patients should have antihypertensive drug therapy initiated at a BP ≥130/80 mm Hg.1200 Individualize drug therapy in patients with hypertension and underlying cardiovascular or other risk factors.502 1200
In stage 1 hypertension, experts state that it is reasonable to initiate drug therapy using the stepped-care approach in which one drug is initiated and titrated and other drugs are added sequentially to achieve the target BP.1200 Initiation of antihypertensive therapy with 2 first-line agents from different pharmacologic classes recommended in adults with stage 2 hypertension and average BP >20/10 mm Hg above BP goal.1200
Triamterene Dosage and Administration
General
Monitoring and BP Treatment Goals
-
Monitor BP regularly (i.e., monthly) during therapy and adjust dosage of the antihypertensive drug(s) until BP controlled.1200
-
If unacceptable adverse effects occur, discontinue drug and initiate another antihypertensive agent from a different pharmacologic class.1216
-
If adequate BP response not achieved with a single antihypertensive agent, either increase dosage of single drug or add a second drug with demonstrated benefit and preferably a complementary mechanism of action (e.g., ACE inhibitor, angiotensin II receptor antagonist, calcium-channel blocker, thiazide diuretic).1200 1216 Many patients will require ≥2 drugs from different pharmacologic classes to achieve BP goal; if goal BP still not achieved with 2 antihypertensive agents, add a third drug.1200 1216 1220
-
Assess patient's renal function and electrolytes 2–4 weeks after initiation of diuretic therapy.1200
-
Monitor serum potassium concentrations following changes in dosage or with concurrent illness or drug therapy.b d (See Hyperkalemia under Cautions and also see Interactions.)
-
Avoid use of potassium-sparing diuretics, including triamterene, in patients with renal insufficiency, in those with hyperkalemia who have serum potassium concentrations >5 mEq/L while not receiving drug therapy, and in those who develop hyperkalemia during therapy.b c d
-
Do not use concurrent potassium supplementation or potassium-containing salt substitutes.b Discontinue potassium supplementation when triamterene is added to other diuretic therapy or when patients are switched to triamterene from other diuretics.b
-
Do not use fixed-combination triamterene/hydrochlorothiazide tablets or capsules for initial therapy of edema or hypertension, except in patients in whom the clinical consequences of hypokalemia represent an important risk (e.g., patients receiving cardiac glycosides or patients with cardiac arrhythmias).a c d
-
Do not use as initial monotherapy in severe heart failure since bowel edema or intestinal hypoperfusion may delay absorption and subsequent therapeutic effect.a
-
Careful etiologic diagnosis should precede the use of any diuretic.a
Administration
Oral Administration
Capsules: Administer orally twice daily after meals.b
Fixed-combination triamterene/hydrochlorothiazide tablets or capsules: Administer orally once daily.c d
Twice-daily administration of the fixed combination of triamterene and hydrochlorothiazide may increase risk of electrolyte imbalance and renal dysfunction.d
Dosage
Individualize dosage according to patient’s requirements and response.b
If added to an existing antihypertensive regimen, initially reduce dosage of each antihypertensive agent and then individualize dosage according to patient’s requirements and response.b
Abrupt discontinuance may result in rebound kaliuresis; taper dosage gradually.b
For the management of fluid retention associated with heart failure, experts state that diuretics should be administered at a dosage sufficient to achieve optimal volume status and relieve congestion without inducing an excessively rapid reduction in intravascular volume, which could result in hypotension, renal dysfunction, or both.524
Pediatric Patients
Usual Dosage† [off-label]
Oral
Initially, 2–4 mg/kg daily or 115 mg/m2 daily, given in a single dose or 2 divided doses after meals.a e
If necessary, increase dosage to 6 mg/kg daily.a Do not exceed 300 mg daily.b e
Hypertension† [off-label]
Oral
Some experts have recommended an initial dosage of 1–2 mg/kg daily given in 2 divided doses after meals.120 Increase dosage as necessary up to 3–4 mg/kg daily given in 2 divided doses.120 Do not exceed 300 mg daily.120
Adults
Edema
Triamterene Therapy
OralInitially, 100 mg twice daily after meals.b After edema is controlled, usual maintenance dosage is 100 mg daily or every other day.a Do not exceed 300 mg daily.b
For management of fluid retention (e.g., edema) associated with heart failure, some experts recommend initiating triamterene at a low dosage (e.g., 50–75 mg twice daily) and increasing dosage (maximum 200 mg daily) until urine output increases and weight decreases, generally by 0.5–1 kg daily.524
Triamterene/Hydrochlorothiazide Fixed-combination Therapy
OralWhen Dyazide, Maxzide or Maxzide-25 mg, or therapeutically equivalent formulations of these combinations are used, the usual dosage in terms of triamterene is 37.5–75 mg once daily.c d
Patients receiving 25 mg of hydrochlorothiazide who become hypokalemic may be switched to Maxzide-25 mg (37.5 mg triamterene/25 mg hydrochlorothiazide).121
Patients receiving 50 mg of hydrochlorothiazide who become hypokalemic may be switched to Maxzide (75 mg triamterene/50 mg hydrochlorothiazide).121
Patients who require hydrochlorothiazide and in whom hypokalemia cannot be risked may initiate therapy with Maxzide-25 mg (37.5 mg triamterene/25 mg hydrochlorothiazide) daily.121
Risk of electrolyte imbalance and renal dysfunction may be increased when triamterene 75 mg daily (with hydrochlorothiazide 50 mg daily) is administered in 2 divided doses rather than 1 daily dose.121
Hypertension
Triamterene Therapy
OralUsually combined with a kaliuretic diuretic.a Some experts state that the usual dosage range is 50–100 mg daily (given in 1 or 2 divided doses).1200
Triamterene/Hydrochlorothiazide Fixed-combination Therapy
OralWhen Dyazide, Maxzide or Maxzide-25 mg, or therapeutically equivalent formulations of these combinations are used, the usual dosage in terms of triamterene is 37.5–75 mg once daily.d
Patients receiving 25 mg of hydrochlorothiazide who become hypokalemic may be switched to Maxzide-25 mg (37.5 mg triamterene/25 mg hydrochlorothiazide).121
Patients receiving 50 mg of hydrochlorothiazide who become hypokalemic may be switched to Maxzide (75 mg triamterene/50 mg hydrochlorothiazide).121
Patients who require hydrochlorothiazide and in whom hypokalemia cannot be risked may initiate therapy with Maxzide-25 mg (37.5 mg triamterene/25 mg hydrochlorothiazide) daily.121
If BP is not adequately controlled by use of 75 mg once daily (of triamterene in the fixed combination of triamterene/hydrochlorothiazide), another antihypertensive agent may be added.d
Risk of electrolyte imbalance and renal dysfunction may be increased when triamterene 75 mg daily (with hydrochlorothiazide 50 mg daily) is administered in 2 divided doses rather than 1 daily dose.121
Prescribing Limits
Pediatric Patients
Oral
Maximum 300 mg daily.120
Adults
Oral
Maximum recommended by manufacturer: 300 mg daily.b
Maximum total daily dose recommended by ACCF/AHA for management of fluid retention in heart failure: 200 mg.524
The manufacturer states there is no clinical experience to date with dosages of fixed-combination Maxzide or Maxzide-25 mg exceeding 75 mg of triamterene and 50 mg of hydrochlorothiazide daily.d
Special Populations
Hepatic Impairment
No specific dosage recommendations for hepatic impairment; caution if using fixed combination with hydrochlorothiazide because of risk of precipitating hepatic coma.c d (See Contraindications under Cautions.)
Renal Impairment
No specific dosage recommendations for renal impairment; do not use in patients with renal impairment and elevated serum potassium; discontinue in patients who develop hyperkalemia while on the drug.b ((See Contraindications under Cautions.) and also see Hyperkalemia under Cautions.)
Cautions for Triamterene
Contraindications
-
Anuria, severe or progressive renal disease or dysfunction (except possibly nephrosis), acute or chronic renal insufficiency, substantial renal impairment.b c d
-
Concurrent potassium supplementation, including potassium salts or potassium-containing salt substitutes.b (See Interactions.)
-
Concurrent therapy with potassium-sparing agents (e.g., spironolactone, amiloride hydrochloride, or fixed-combination formulations containing triamterene).b (See Interactions.)
-
Severe hepatic disease.b
-
Known hypersensitivity to triamterene or any ingredient in the formulation.b c d
Warnings/Precautions
Warnings
Hyperkalemia
Hyperkalemia (i.e., serum potassium concentrations ≥5.5 mEq/L) may occur with all potassium-sparing agents, including triamterene.b c d (See Boxed Warning.) Serum potassium concentrations persistently >6 mEq/L require careful observation and treatment.b
If hyperkalemia occurs, discontinue triamterene; if using a triamterene/hydrochlorothiazide fixed combination, switch to a thiazide alone.b c d
Evaluate BUN and serum potassium concentrations regularly, especially in patients with suspected or confirmed renal insufficiency.b Monitor serum potassium concentrations closely in geriatric and diabetic patients.b
Warning signs of hyperkalemia include paresthesias, muscular weakness, fatigue, flaccid paralysis of the extremities, bradycardia, and shock.c d
Hyperkalemia has been associated with cardiac irregularities.b Obtain ECG if hyperkalemia present or suspected.b If ECG does not show widening of QRS or arrhythmia in the presence of hyperkalemia, usually sufficient to discontinue triamterene and any potassium supplementation and switch to a thiazide alone.b May administer sodium polystyrene sulfonate to enhance excretion of excess potassium.b
Presence of widened QRS complex or arrhythmia in association with hyperkalemia requires prompt additional therapy.b For tachyarrhythmia, infuse 44 mEq of sodium bicarbonate or 10 mL of 10% calcium gluconate or calcium chloride over several minutes.b For asystole, bradycardia, or AV block, transvenous pacing also is recommended.b The effect of calcium and sodium bicarbonate is transient and repeated administration may be required.b When indicated by the clinical situation, excess potassium may be removed by dialysis or oral or rectal administration of sodium polystyrene sulfonate.b Infusion of glucose and insulin has also been used to treat hyperkalemia.b
Potassium Supplementation
Do not use potassium supplementation (e.g., potassium salts, high potassium diet, salt substitutes) in patients receiving triamterene alone.b Discontinue potassium supplements when triamterene is added to existing diuretic therapy or when patients are switched to triamterene from other diuretics.b
Do not use potassium supplementation with fixed-combination triamterene/hydrochlorothiazide except in severe cases of hypokalemia or if dietary intake of potassium is markedly impaired.a c Such concomitant therapy may be associated with rapid increases in serum potassium concentrations.c Monitor serum potassium concentrations frequently if potassium supplementation is used, especially in patients receiving digitalis or with a history of cardiac arrhythmias.c (See Interactions.)
If serious hypokalemia (serum potassium <3.0 mEq/L demonstrated by repeat serum potassium determinations) occurs in a patient receiving fixed-combination triamterene/hydrochlorothiazide, discontinue fixed combination and initiate potassium supplementation.c
If hyperkalemia occurs in a patient receiving fixed-combination triamterene/hydrochlorothiazide and supplemental potassium therapy, discontinue supplementation and substitute a thiazide diuretic alone for fixed-combination triamterene/hydrochlorothiazide until potassium concentrations return to normal.c
Sensitivity Reactions
Hypersensitivity Reactions
Hypersensitivity reactions (e.g., anaphylaxis, rash, photosensitivity) reported; monitor for blood dyscrasias, liver damage or other idiosyncratic reactions.b
General Precautions
Use of Fixed Combinations
When triamterene is used in fixed combination with hydrochlorothiazide, consider the cautions, precautions, and contraindications associated with hydrochlorothiazide.d
Use during Pregnancy
Routine use of diuretics, including triamterene, in otherwise healthy women exposes mother and fetus to unnecessary risk and is not generally indicated.b c d Diuretics do not prevent development of toxemia of pregnancy and do not appear to be beneficial in the treatment of toxemia.b c d
Edema may develop during pregnancy due to comorbid pathology or the physiologic and mechanical consequences of pregnancy.b c d Diuretic therapy may be appropriate in the management of edema due to a pathologic cause manifesting during pregnancy.b c d However, dependent edema in pregnancy resulting from restriction of venous return by the gravid uterus may be treated by elevating the lower extremities and using support hose; diuretic therapy to lower intravascular volume is not appropriate in such cases.b c d
Hypervolemia and associated edema, including generalized edema, occurs in the majority of pregnant women and is not harmful to fetus or mother.b c d Increased recumbency will generally provide relief; however, edema may cause extreme discomfort which is not relieved by rest.b c d Rarely, in such cases, a short course of diuretic therapy may be appropriate to provide relief.b c d
Electrolyte Imbalance
Electrolyte imbalance may worsen or develop during diuretic therapy, including triamterene.b Risk of electrolyte imbalance is increased in patients with heart failure, renal disease, or cirrhosis.b Full-dose diuretic therapy in patients on restricted salt intake may cause a low-salt syndrome.b
Monitor serum electrolytes regularly.d
Renal Effects
Elevations in BUN and/or Scr may occur, possibly secondary to a reversible reduction of GFR or a depletion of the intravascular fluid volume.d May occur more frequently in patients receiving twice-daily dosing with fixed combination of triamterene and hydrochlorothiazide.d
Monitor BUN and Scr, especially in geriatric patients and those with suspected or confirmed hepatic or renal disease.d If azotemia increases, discontinue fixed-combination triamterene/hydrochlorothiazide preparation.d
Nitrogen Retention
May cause mild nitrogen retention, which is reversible upon drug discontinuance; seldom observed with intermittent (every-other-day) therapy.b
Metabolic Acidosis
May cause a decreasing alkali reserve with the possibility of metabolic acidosis.b
Avoid use of potassium-sparing diuretics in severely ill patients in whom respiratory or metabolic acidosis may occur; acidosis may result in rapid increases in serum potassium concentrations.c d Perform frequent assessments of acid-base balance and serum electrolytes.c d
Megaloblastosis
Triamterene is a weak folic acid antagonist and may contribute to the appearance of megaloblastosis, especially in patients with depleted folic acid stores (e.g., pregnant women, alcoholics).a b Patients with cirrhosis and splenomegaly may have marked hematologic abnormalities; these patients should have periodic blood studies and be observed for exacerbations of underlying liver disease.b
Hyperuricemia
May cause elevations in serum uric acid concentrations, especially in patients predisposed to gouty arthritis.b
Renal Calculi
Has been reported in renal calculi associated with usual calculus components.b c d Manufacturers state that triamterene may be used with caution in patients with histories of renal calculi;b c d however, some clinicians recommend that the drug not be used in these patients because of the risk of triamterene nephrolithiasis.a
If a patient passes a urinary calculus during triamterene therapy, the drug should be discontinued and the calculus analyzed for the presence of triamterene and/or its metabolites.a
Rebound Kaliuresis
Because triamterene conserves potassium, it has been suggested that patients who have received intensive therapy or have been given the drug for prolonged periods may develop a rebound kaliuresis if such therapy is discontinued abruptly.b Discontinue drug gradually in such patients.b
Specific Populations
Pregnancy
Lactation
Distributed into milk in animals and is likely to distribute into human milk.b Discontinue nursing or the drug.b
Pediatric Use
Safety and efficacy in pediatric patients remain to be fully established for triamterene or triamterene in fixed combination with hydrochlorothiazide;b c however, some experts have suggested a triamterene dosage for hypertension based on limited clinical experience.120
Geriatric Use
Reduced clearance and increased risk of hyperkalemia; monitor serum potassium concentrations frequently.b c d (See Hyperkalemia under Cautions.)
Hepatic Impairment
Use with caution in patients with impaired hepatic function.a Do not use in patients with severe hepatic disease.a Diuretic therapy in such patients should be initiated while the patient is hospitalized, because rapid alterations in fluid and electrolyte balance may precipitate hepatic coma.a Monitor serum potassium concentrations closely in patients with hepatic cirrhosis and administer potassium supplementation if required.a (See Contraindications under Cautions.)
Potassium loss has been reported during triamterene therapy in some patients with hepatic cirrhosis and may result in signs and symptoms of hepatic coma or precoma.a
Patients with cirrhosis and splenomegaly may have marked hematologic abnormalities; these patients should have periodic blood studies and be observed for exacerbations of underlying liver disease.b (See Megablastosis under Cautions.)
Renal Impairment
Use with caution; increased risk of hyperkalemia.b Monitor serum potassium concentrations closely.b Do not use in patients with renal impairment and elevated serum potassium; discontinue in patients who develop hyperkalemia while on the drug.b (See Contraindications under Cautions and also see Hyperkalemia under Cautions.)
Common Adverse Effects
Hyperkalemia, azotemia, increased BUN and creatinine, renal calculi, jaundice and/or liver enzyme abnormalities, nausea and vomiting, diarrhea, thrombocytopenia, megaloblastic anemia, weakness, fatigue, dizziness, headache, dry mouth.b
Drug Interactions
Specific Drugs, Foods, and Laboratory Tests
|
Drug, Food, or Test |
Interaction |
Comments |
|---|---|---|
|
ACE inhibitors |
Use caution with concomitant ACE inhibitor therapy; monitor serum potassium concentrations frequentlya b d Use potassium-sparing diuretics with great caution, if at all, in patients receiving an ACE inhibitor (e.g., enalapril) for heart failurea Discontinue or reduce dosage of potassium-sparing diuretics as necessary in patients receiving an ACE inhibitora |
|
|
Anesthetic agents |
Possible potentiation of anesthetic effectsb |
|
|
Antidiabetic agents (e.g., insulin, oral agents) |
Possible increase in blood glucose concentrationb |
Adjust dosage of antidiabetic agent during triamterene therapy and after discontinuanceb |
|
Antihypertensive agents |
Possible additive antihypertensive effectsb |
|
|
Blood products |
Increased risk of hyperkalemiab May promote potassium accumulation; plasma from blood bank may contain up to 30 mEq/L of potassium and whole blood may contain up to 65 mEq/L if stored for >10 daysb |
|
|
Chlorpropamide |
||
|
Diuretics |
Possible potentiation of diuretic effectsb |
|
|
Diuretics, potassium-sparing (e.g., amiloride, spironolactone, other fixed-dose combination formulations containing triamterene) |
Increased risk of hyperkalemia; fatalities reportedb |
Concomitant use contraindicatedb |
|
Laxatives |
Possible decreased potassium-retaining effects of triamterenec Chronic use or overuse of laxatives may reduce serum potassium concentrations by promoting excessive potassium loss from Gl tractc |
|
|
Lithium |
Reduced renal clearance of lithium and increased risk of lithium toxicityb c |
Concomitant use generally contraindicated; if concomitant therapy is necessary, monitor serum lithium concentrations closely and adjust dosageb c |
|
Nondepolarizing neuromuscular blocking agents |
Potential increase in neuromuscular blockadeb |
|
|
NSAIAs (e.g., indomethacin) |
Concomitant use with indomethacin may adversely affect renal function (e.g., decreased Clcr, acute anuric renal failure)105 106 |
Concomitant use with indomethacin not recommendeda |
|
Preanesthetic agents |
Possible potentiation of effects of preanesthetic agentb |
|
|
Potassium supplements, potassium-containing medications (e.g., parenteral penicillin G potassium) and/or foods containing potassium (e.g., salt substitutes, low-salt milk) |
Increased risk of hyperkalemia, especially in patients with renal insufficiencyb |
Concomitant use generally contraindicatedb |
|
Tests, fluorometric (e.g., lactic dehydrogenase activity) |
Possible interference due to pale blue fluorescence in urinea |
|
|
Tests, fluorometric assay for quinidine |
Interferes with the fluorometric assay of quinidine; the two drugs have similar fluorescence spectrab c |
Triamterene Pharmacokinetics
Absorption
Bioavailability
Triamterene and fixed combinations with hydrochlorothiazide are rapidly absorbed following oral administration;c d peak plasma concentrations achieved within 1–4 hours.a b d Interindividual variation in degree of absorption reported.a
Oral bioavailabilities of triamterene and hydrochlorothiazide from Dyazide capsules are comparable to those of aqueous suspensions of the individual drugs, averaging 85 and 82%, respectively, for the fixed-dose formulation and 100 and 100%, respectively, for the suspensions.111 Dyazide capsules also are bioequivalent to single-entity 25-mg hydrochlorothiazide tablets and 37.5-mg triamterene capsules.110
Oral bioavailabilities of triamterene and hydrochlorothiazide from Maxzide tablets are comparable to those of aqueous suspensions of the individual drugs.d The hydrochlorothiazide component of Maxzide tablets is bioequivalent to single-entity hydrochlorothiazide tablet formulations.d
Onset
Onset of diuresis following oral administration of triamterene usually occurs within 2–4 hours; maximum therapeutic effect may not occur until after several days of therapy.b
Onset of diuresis after oral administration of Dyazide usually occurs within 1 hour and peaks at 2–3 hours.c
Duration
After oral administration of triamterene, diuresis diminishes in approximately 7–9 hours,a b although the total duration of action may be ≥24 hours.a
After oral administration of Dyazide, diuresis diminishes in approximately 7–9 hours.c
Food
Administration of Dyazide with a high-fat meal in healthy adults increased the average bioavailabilities of triamterene, 6-p-hydroxytriamterene, and hydrochlorothiazide by about 67, 50, and 17%, respectively; increased the peak concentrations of triamterene and its p-hydroxy metabolite; and delayed absorption of the active drugs by up to 2 hours.110
Administration with food does not affect absorption of triamterene or hydrochlorothiazide from Maxzide tablets.d
Distribution
Extent
Distributed into bile.a
Crosses the placenta and distributes into milk in animals.b
Plasma Protein Binding
Approximately 67%.b
Elimination
Metabolism
Primarily metabolized to 6-p-hydroxytriamterene and its sulfate conjugate.b 107
Elimination Route
Excreted in urine, primarily as 6-p-hydroxytriamterene.b
Half-life
100–150 minutes.a
Special Populations
Renal clearances of triamterene, hydroxytriamterene sulfate, and hydrochlorothiazide may be reduced in geriatric patients receiving combined triamterene and hydrochlorothiazide therapy, principally as a result of age-related reductions in renal function.107 a
Stability
Storage
Oral
Capsules
Tight, light resistant containers at 15–30°C.a b
Fixed-dose Combination Formulations
Dyazide capsules: Tight, light resistant containers at 20–25°C.c
Maxzide tablets: Tight, light resistant containers at 15–30°C.d
Actions
-
A pteridine derivative, potassium-sparing diuretic that is structurally related to folic acid.a b
-
Does not competitively inhibit aldosterone; activity is independent of aldosterone concentrations.b
-
Does not inhibit carbonic anhydrase.a
-
Acts directly on the distal renal tubule of the nephron to depress aldosterone-stimulated reabsorption of sodium and excretion of potassium and hydrogen at that site.b
-
Increases excretion of sodium, calcium, magnesium, and bicarbonate.a
-
Potassium excretion usually reduced; serum concentrations of potassium and chloride are usually increased.a b
-
Serum bicarbonate concentrations consistently decreased; urinary pH increased slightly.a
-
Reductions in glomerular filtration observed during daily, but not intermittent, administration; suggests a reversible effect on renal blood flow.a
-
Although effective alone, often used in combination with other diuretics that act at different sites in the nephron.a
-
Little if any hypotensive effect when used alone.a
Advice to Patients
-
Importance of taking drug after meals to help avoid stomach upset.b
-
Importance of informing patients that if a single daily dose is prescribed, it may be preferable to take it in the morning to minimize the effect of increased frequency of urination on nighttime sleep.b
-
Importance of informing patients that if a dose is missed, the patient should take only the prescribed dose at the next dosing interval.b
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.b c d
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.b c d
-
Importance of informing patients of other important precautionary information.b c d (See Cautions.)
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
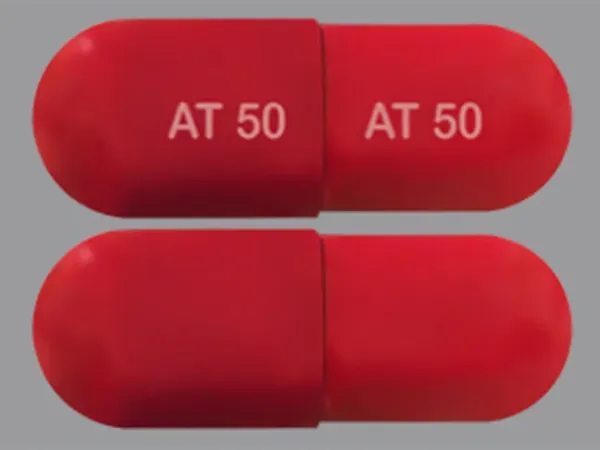
Oral |
Capsules |
50 mg |
Dyrenium |
WellSpring |
|
100 mg |
Dyrenium |
WellSpring |
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Capsules |
37.5 mg Triamterene and Hydrochlorothiazide 25 mg* |
Dyazide |
GlaxoSmithKline |
|
Triamterene and Hydrochlorothiazide Capsules |
||||
|
Tablets |
37.5 mg Triamterene and Hydrochlorothiazide 25 mg* |
Maxzide-25 (scored) |
Mylan |
|
|
Triamterene and Hydrochlorothiazide Tablets |
||||
|
75 mg Triamterene and Hydrochlorothiazide 50 mg* |
Maxzide (scored) |
Mylan |
||
|
Triamterene and Hydrochlorothiazide Tablets |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
Only references cited for selected revisions after 1984 are available electronically.
100. Upton RA, Williams RL, Lin ET et al. Absence of a significant pharmacokinetic interaction between hydrochlorothiazide and triamterene when coadministered. J Pharmacokinet Biopharm. 1984; 12:575-86. https://pubmed.ncbi.nlm.nih.gov/6533293
101. Blume CD, Williams RL, Upton RA et al. Bioequivalence study of a new tablet formulation of triamterene and hydrochlorothiazide. Am J Med. 1984; 77(Suppl 5A):59-61. https://pubmed.ncbi.nlm.nih.gov/6496560
102. Blume CD, Williams RL. A new antihypertensive agent: Maxzide (75 mg triamterene/50 mg hydrochlorothiazide). Am J Med. 1984; 77(Suppl 5A):52-8. https://pubmed.ncbi.nlm.nih.gov/6388327
104. Houston MC. Thiazides and thiazide-like diuretics in hypertension. Ann Intern Med. 1985; 103:303. https://pubmed.ncbi.nlm.nih.gov/4014913
105. Favre L, Glasson P, Vallotton MB. Reversible acute renal failure from combined triamterene and indomethacin. Ann Intern Med. 1982; 96:317-20. https://pubmed.ncbi.nlm.nih.gov/6949485
106. Weinberg MS, Quigg RJ, Salant DJ et al. Anuric renal failure precipitated by indomethacin and triamterene. Nephron. 1985; 40:216-8. https://pubmed.ncbi.nlm.nih.gov/4000350
107. Williams RL, Thornhill MD, Upton RA et al. Absorption and disposition of two combination formulations of hydrochlorothiazide and triamterene: influence of age and renal function. Clin Pharmacol Ther. 1986; 40:226-32. https://pubmed.ncbi.nlm.nih.gov/3731685
108. Lederle Laboratories. Maxzide and Maxzide-25 MG tablets prescribing information. Pearl River, NY; 1988 May.
110. SmithKline Beecham. Dyazide (triamterene and hydrochlorothiazide) capsules prescribing information (DZ:L65A). In: Physicians’ desk reference. 52nd ed. Montvale, NJ; 1998:2819-20.
111. SmithKline Beecham, Philadelphia, PA: Personal communication.
113. The Captopril-Digoxin Multicenter Research Group. Comparative effects of therapy with captopril and digoxin in patients with mild to moderate heart failure. JAMA. 1988; 259:539-44. https://pubmed.ncbi.nlm.nih.gov/2447297
114. Richardson A, Bayliss J, Scriven AJ et al. Double-blind comparison of captopril alone against frusemide plus amiloride in mild heart failure. Lancet. 1987; 2:709-11. https://pubmed.ncbi.nlm.nih.gov/2888942
115. Sherman LG, Liang CS, Baumgardner S et al. Piretanide, a potent diuretic with potassium-sparing properties, for the treatment of congestive heart failure. Clin Pharmacol Ther. 1986; 40:587-94. https://pubmed.ncbi.nlm.nih.gov/3533372
116. Patterson JH, Adams KF Jr, Applefeld MM et al. Oral torsemide in patients with chronic congestive heart failure: effects on body weight, edema, and electrolyte excretion. Pharmacotherapy. 1994; 14:514-21. https://pubmed.ncbi.nlm.nih.gov/7997385
117. Wilson JR, Reichek N, Dunkman WB et al. Effect of diuresis on the performance of the failing left ventricle in man. Am J Med. 1981;70:234-9.
118. Parker JO. The effects of oral ibopamine in patients with mild heart failure—a double blind placebo controlled comparison to furosemide. Int J Cardiol. 1993; 40:221-7. https://pubmed.ncbi.nlm.nih.gov/8225657
120. National High Blood Pressure Education Program Working Group on Hypertension Control in Children and Adolescents. The fourth report on the diagnosis, evaluation, and treatment of high blood pressure in children and adolescents. Pediatrics. 2004; 114(Suppl 2):555-76.
121. Mylan Pharmaceuticals. Maxzide and Maxzide-25 (triamterene and hydrochlorothiazide) tablets prescribing information. Morgantown, WV; 2011 Jan.
500. National Heart, Lung, and Blood Institute National High Blood Pressure Education Program. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC 7). Bethesda, MD: National Institutes of Health; 2004 Aug. (NIH publication No. 04-5230.)
501. James PA, Oparil S, Carter BL et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014; 311:507-20. https://pubmed.ncbi.nlm.nih.gov/24352797
502. Mancia G, Fagard R, Narkiewicz K et al. 2013 ESH/ESC Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2013; 31:1281-357. https://pubmed.ncbi.nlm.nih.gov/23817082
503. Go AS, Bauman MA, Coleman King SM et al. An effective approach to high blood pressure control: a science advisory from the American Heart Association, the American College of Cardiology, and the Centers for Disease Control and Prevention. Hypertension. 2014; 63:878-85. https://pubmed.ncbi.nlm.nih.gov/24243703
504. Weber MA, Schiffrin EL, White WB et al. Clinical practice guidelines for the management of hypertension in the community: a statement by the American Society of Hypertension and the International Society of Hypertension. J Clin Hypertens (Greenwich). 2014; 16:14-26. https://pubmed.ncbi.nlm.nih.gov/24341872
505. Wright JT, Fine LJ, Lackland DT et al. Evidence supporting a systolic blood pressure goal of less than 150 mm Hg in patients aged 60 years or older: the minority view. Ann Intern Med. 2014; 160:499-503. https://pubmed.ncbi.nlm.nih.gov/24424788
506. Mitka M. Groups spar over new hypertension guidelines. JAMA. 2014; 311:663-4. https://pubmed.ncbi.nlm.nih.gov/24549531
507. Peterson ED, Gaziano JM, Greenland P. Recommendations for treating hypertension: what are the right goals and purposes?. JAMA. 2014; 311:474-6. https://pubmed.ncbi.nlm.nih.gov/24352710
508. Bauchner H, Fontanarosa PB, Golub RM. Updated guidelines for management of high blood pressure: recommendations, review, and responsibility. JAMA. 2014; 311:477-8. https://pubmed.ncbi.nlm.nih.gov/24352759
515. Thomas G, Shishehbor M, Brill D et al. New hypertension guidelines: one size fits most?. Cleve Clin J Med. 2014; 81:178-88. https://pubmed.ncbi.nlm.nih.gov/24591473
523. Fihn SD, Gardin JM, Abrams J et al. 2012 ACCF/AHA/ACP/AATS/PCNA/SCAI/STS guideline for the diagnosis and management of patients with stable ischemic heart disease: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines, and the American College of Physicians, American Association for Thoracic Surgery, Preventive Cardiovascular Nurses Association, Society for Cardiovascular Angiography and Interventions, and Society of Thoracic Surgeons. Circulation. 2012; 126:e354-471.
524. WRITING COMMITTEE MEMBERS, Yancy CW, Jessup M et al. 2013 ACCF/AHA guideline for the management of heart failure: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2013; 128:e240-327.
526. Kernan WN, Ovbiagele B, Black HR et al. Guidelines for the Prevention of Stroke in Patients With Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals From the American Heart Association/American Stroke Association. Stroke. 2014; 45:2160-2236. https://pubmed.ncbi.nlm.nih.gov/24788967
530. Myers MG, Tobe SW. A Canadian perspective on the Eighth Joint National Committee (JNC 8) hypertension guidelines. J Clin Hypertens (Greenwich). 2014; 16:246-8. https://pubmed.ncbi.nlm.nih.gov/24641124
536. Kidney Disease: Improving Global Outcomes (KDIGO) Blood Pressure Work Group. KDIGO clinical practice guideline for the management of blood pressure in chronic kidney disease. Kidney Int Suppl. 2012: 2: 337-414.
700. Yancy CW, Jessup M, Bozkurt B et al. 2016 ACC/AHA/HFSA Focused Update on New Pharmacological Therapy for Heart Failure: An Update of the 2013 ACCF/AHA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Failure Society of America. Circulation. 2016; :.
713. Gupta D, Georgiopoulou VV, Kalogeropoulos AP et al. Dietary sodium intake in heart failure. Circulation. 2012; 126:479-85. https://pubmed.ncbi.nlm.nih.gov/22825409
714. Hospira. Dopamine hydrochloride prescribing information. Lake Forest, IL; 2014 Mar.
715. Hospira. Dopamine hydrochloride and 5% dextrose injection prescribing information. Lake Forest, IL; 2014 May.
716. Cicci JD, Reed BN, McNeely EB et al. Acute decompensated heart failure: evolving literature and implications for future practice. Pharmacotherapy. 2014; 34:373-88. https://pubmed.ncbi.nlm.nih.gov/24214219
717. Triposkiadis FK, Butler J, Karayannis G et al. Efficacy and safety of high dose versus low dose furosemide with or without dopamine infusion: the Dopamine in Acute Decompensated Heart Failure II (DAD-HF II) trial. Int J Cardiol. 2014;172(1):115-21.
718. Torres-Courchoud I, Chen HH. Is there still a role for low-dose dopamine use in acute heart failure?. Curr Opin Crit Care. 2014; 20:467-71. https://pubmed.ncbi.nlm.nih.gov/25137402
719. Houston BA, Kalathiya RJ, Kim DA et al. Volume Overload in Heart Failure: An Evidence-Based Review of Strategies for Treatment and Prevention. Mayo Clin Proc. 2015; 90:1247-61. https://pubmed.ncbi.nlm.nih.gov/26189443
720. Chen HH, Anstrom KJ, Givertz MM et al. Low-dose dopamine or low-dose nesiritide in acute heart failure with renal dysfunction: the ROSE acute heart failure randomized trial. JAMA. 2013; 310:2533-43. https://pubmed.ncbi.nlm.nih.gov/24247300 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3934929/
723. Hummel SL, Konerman MC. Dietary Sodium Restriction in Heart Failure: A Recommendation Worth its Salt?. JACC Heart Fail. 2016; 4:36-8. https://pubmed.ncbi.nlm.nih.gov/26738950
724. Yancy CW. The Uncertainty of Sodium Restriction in Heart Failure: We Can Do Better Than This. JACC Heart Fail. 2016; 4:39-41. https://pubmed.ncbi.nlm.nih.gov/26738951
1200. Whelton PK, Carey RM, Aronow WS et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA Guideline for the Prevention, Detection, Evaluation, and Management of High Blood Pressure in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Hypertension. 2018; 71:el13-e115. https://pubmed.ncbi.nlm.nih.gov/29133356
1201. Bakris G, Sorrentino M. Redefining hypertension - assessing the new blood-pressure guidelines. N Engl J Med. 2018; 378:497-499. https://pubmed.ncbi.nlm.nih.gov/29341841
1202. Carey RM, Whelton PK, 2017 ACC/AHA Hypertension Guideline Writing Committee. Prevention, detection, evaluation, and management of high blood pressure in adults: synopsis of the 2017 American College of Cardiology/American Heart Association hypertension guideline. Ann Intern Med. 2018; 168:351-358. https://pubmed.ncbi.nlm.nih.gov/29357392
1207. Burnier M, Oparil S, Narkiewicz K et al. New 2017 American Heart Association and American College of Cardiology guideline for hypertension in the adults: major paradigm shifts, but will they help to fight against the hypertension disease burden?. Blood Press. 2018; 27:62-65. https://pubmed.ncbi.nlm.nih.gov/29447001
1209. Qaseem A, Wilt TJ, Rich R et al. Pharmacologic treatment of hypertension in adults aged 60 years or older to higher versus lower blood pressure targets: a clinical practice guideline from the American College of Physicians and the American Academy of Family Physicians. Ann Intern Med. 2017; 166:430-437. https://pubmed.ncbi.nlm.nih.gov/28135725
1210. SPRINT Research Group, Wright JT, Williamson JD et al. A randomized trial of intensive versus standard blood-pressure control. N Engl J Med. 2015; 373:2103-16. https://pubmed.ncbi.nlm.nih.gov/26551272
1216. Taler SJ. Initial treatment of hypertension. N Engl J Med. 2018; 378:636-644. https://pubmed.ncbi.nlm.nih.gov/29443671
1220. Cifu AS, Davis AM. Prevention, detection, evaluation, and management of high blood pressure in adults. JAMA. 2017; 318:2132-2134. https://pubmed.ncbi.nlm.nih.gov/29159416
1222. Bell KJL, Doust J, Glasziou P. Incremental benefits and harms of the 2017 American College of Cardiology/American Heart Association high blood pressure guideline. JAMA Intern Med. 2018; 178:755-7. https://pubmed.ncbi.nlm.nih.gov/29710197
1223. LeFevre M. ACC/AHA hypertension guideline: what is new? what do we do?. Am Fam Physician. 2018; 97(6):372-3. https://pubmed.ncbi.nlm.nih.gov/29671534
1224. Brett AS. New hypertension guideline is released. From NEJM Journal Watch website. Accessed 2018 Jun 18. https://www.jwatch.org/na45778/2017/12/28/nejm-journal-watch-general-medicine-year-review-2017
1229. Ioannidis JPA. Diagnosis and treatment of hypertension in the 2017 ACC/AHA guidelines and in the real world. JAMA. 2018; 319(2):115-6. https://pubmed.ncbi.nlm.nih.gov/29242891
a. AHFS Drug Information 2017. McEvoy GK, ed. Triamterene. American Society of Health-System Pharmacists; 2017: .
b. WellSpring Pharmaceutical Corporation. Dyrenium (triamterene) capsules prescribing information. Neptune, NJ; 2001 June.
c. GlaxoSmithKline. Dyazide capsules prescribing information. Philadelphia, PA; 1999 Feb.
d. Bertek. Maxzide and Maxzide-25 mg tablets prescribing information. Sugar Land, TX; 2002 Dec.
e. Laboratory medicine, drug therapy, and reference tables. In: Behrman RE, Kliegman RM, Jenson HB, eds. Nelson textbook of pediatrics. 17th ed. Philadelphia: Saunders; 2004:2482.
f. AHFS drug information 2019. McEvoy GK, ed. Thiazides general statement. Bethesda, MD: American Society of Health-System Pharmacists; 2019: .
Related/similar drugs
More about triamterene
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (10)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Drug class: potassium-sparing diuretics
- Breastfeeding
- En español