Sotalol (Monograph)
Brand names: Betapace, Betapace AF, Sorine, Sotylize
Drug class: beta-Adrenergic Blocking Agents
Warning
-
Risk of life-threatening ventricular tachycardia associated with QT interval prolongation.1 402 403 404
-
Initiate or reinitiate therapy (or perform conversion from IV to oral therapy) in a facility that can provide cardiac resuscitation, continuous ECG monitoring, and Clcr calculations.1 402 403 404 (See Proarrhythmic Effects under Cautions.)
-
Do not initiate sotalol if baseline QTc >450 msec.402 403 If prolongation of QT interval to ≥500 msec occurs during therapy, reduce dose, increase dosing interval, or discontinue therapy.1 402 403 404
-
Calculate Clcr and adjust dosing interval accordingly.1 402 403 404 (See General under Dosage and Administration.)
Introduction
Nonselective β-adrenergic blocking agent; exhibits antiarrhythmic activity characteristic of class II antiarrhythmic agents and electrophysiologic effects characteristic of class III antiarrhythmic agents.1 2 7 8 12 13 14 15 402 403 404
Uses for Sotalol
Ventricular Arrhythmias
Used to suppress and prevent recurrence of documented life-threatening ventricular arrhythmias (e.g., sustained ventricular tachycardia);1 4 5 6 7 8 11 12 26 400 401 402 403 404 405 designated an orphan drug by FDA for such use.9
Shown to be effective in patients with life-threatening ventricular arrhythmias (e.g., sustained ventricular tachycardia or fibrillation) as well as those with less severe arrhythmias (e.g., premature ventricular complexes [PVCs], paired PVCs, nonsustained ventricular tachycardia)1 4 5 6 7 11 12 402 403 404
Although antiarrhythmic drugs, including sotalol, may suppress the recurrence of arrhythmias and improve symptoms, there is no evidence from randomized controlled studies indicating that these drugs have a beneficial effect on mortality or sudden death.1 405
Because of arrhythmogenic potential, lack of evidence for improved survival, and risk of serious adverse effects (see Proarrhythmic Effects under Cautions), use in patients with less severe arrhythmias, even if symptomatic, generally notrecommended.1 402 403
Avoid treatment of asymptomatic PVCs.1 3 4 7 8 12 14 402 403 404
Not a first-line drug of choice during cardiac arrest, but may be used for treatment of hemodynamically stable sustained monomorphic ventricular tachycardia; included in current ACLS guidelines for adult tachycardia.400 401 405
Supraventricular Arrhythmias
Used to maintain normal sinus rhythm in patients with symptomatic atrial fibrillation or flutter who are currently in sinus rhythm.1 301 402 403 404
Because of potential for life-threatening ventricular arrhythmias, reserve use for highly symptomatic atrial fibrillation/flutter.1 42 51 56 57 402 403 404 (See Proarrhythmic Effects under Cautions.) Do not use in patients with easily reversible (e.g., with Valsalva maneuver) paroxysmal atrial fibrillation.1 402 403 404
Efficacy in preventing atrial fibrillation or flutter recurrences is comparable to that of quinidine or propafenone and less than that of amiodarone.43 44 45 47 301
Also has been used for treatment of other supraventricular tachycardias (SVTs), including paroxysmal supraventricular tachycardia (PSVT)† [off-label] due to AV nodal reentry tachycardia (AVNRT) or AV reentry tachycardia (AVRT).64 300
Sotalol Dosage and Administration
General
-
Initiate or reinitiate therapy and adjust dosage (or perform conversion from IV to oral therapy) in an institutional setting where patient can be monitored by personnel trained in the management of serious arrhythmias.1 7 8 42 48 402 403 404 (See Boxed Warning.)
-
Closely monitor patient for ≥3 days (or until steady-state plasma concentrations are achieved) whenever treatment is initiated, reinitiated, or dosage is increased.1 402 403 404
-
Prior to treatment, calculate Clcr and determine QTc interval.1 402 403 404 (See Contraindications under Cautions.) When titrating dosage, monitor QT interval 2–4 hours after each dose increase (if given orally) or after completion of each IV infusion.1 402 403 404
-
Individualize dosage according to Clcr and QTc.1 403 404 Discontinue therapy, reduce dose, or increase dosing interval if QTc ≥500 msec.1 403 404
-
Measure serum potassium and magnesium concentrations prior to initiating therapy and correct any imbalances.1 404
-
Ensure adequate anticoagulation in patients with atrial fibrillation/flutter.402
Conversion from Other Antiarrhythmic Agents
-
A transition period is recommended for patients converting from another antiarrhythmic agent to sotalol.1 404
-
In general, delay initiation of sotalol for a period of at least 2–3 elimination half-lives of the previously administered antiarrhythmic drug; monitor patients carefully during transition.1 404 (See Specific Drugs under Interactions.)
Administration
Administer orally or by IV infusion (when oral administration not feasible).1 402 403 404
Oral Administration
Administer orally as a tablet or oral solution (using the commercially available oral solution or an extemporaneously prepared solution).1 403 404
Administer oral solution using appropriate measuring device (e.g., oral dosing syringe); use of a teaspoon or tablespoon may result in dosing errors and is not recommended.403
Do not administer aluminum oxide and magnesium hydroxide-containing antacids within 2 hours of administration of sotalol.1 (See Specific Drugs under Interactions.)
Extemporaneous Oral Solution
To prepare extemporaneous oral solution, add 5 tablets (120 mg each) to a 180-mL polyethylene terephthalate (PET) prescription bottle containing 120 mL of simple syrup with 0.1% sodium benzoate (syrup NF); an oversized bottle is used to allow more effective shaking of the mixture.1 404
May add tablets intact to syrup, add syrup to tablets, or crush tablets (making sure to add entire quantity of tablet powder to syrup).1 404
Shake mixture to wet tablets, allow to hydrate for ≥2 hours, then shake intermittently over another 2 hours until dispersion of fine particles is obtained; may hydrate overnight to simplify disintegration process.1 404
If tablets are crushed, shake until a dispersion of fine particles is obtained.1 404
Resulting preparation contains 5 mg/mL of sotalol hydrochloride in solution with suspended inactive solid particles (water-insoluble tablet ingredients).1 (See Storage under Stability.)
IV Administration
For solution and drug compatibility information, see Compatibility under Stability.
Administer by IV infusion over 5 hours.402 Use a volumetric pump to ensure that drug is delivered at a constant rate.402
Must dilute commercially available injection concentrate with a suitable diluent (i.e., 0.9% sodium chloride injection, 5% dextrose injection, lactated Ringer’s injection) prior to administration.402 Manufacturer recommends that the volume of injection concentrate used to prepare the infusion solution and the final infusion solution volume exceed those required for the intended dose to account for dead space in infusion set.402 Preparation of a final volume of 120 or 300 mL is recommended; however, actual volume that should be infused is 100 or 250 mL, respectively.402 (See Table 1.)
|
Target IV Dose |
Amount of Injection Concentrate (mL) |
Amount of Diluent (mL) |
Total Volume Prepared (mL) |
Volume to Infuse (mL) |
|---|---|---|---|---|
|
75 mg |
6 |
114 |
120 |
100 |
|
6 |
294 |
300 |
250 |
|
|
112.5 mg |
9 |
111 |
120 |
100 |
|
9 |
291 |
300 |
250 |
|
|
150 mg |
12 |
108 |
120 |
100 |
|
12 |
288 |
300 |
250 |
Dosage
Available as sotalol hydrochloride; dosage expressed in terms of the salt.1 402 403 404 Adjust dosage carefully according to individual requirements and response, patient tolerance, renal function, and QT interval.1 4 8 402 403 404
If a dose is missed, skip dose and take next dose at regularly scheduled time.1 403 404 Do not take a double dose or increase dosing frequency to compensate for missed dose.1 403 404
Pediatric Patients
Life-threatening Ventricular Arrhythmias or Atrial Fibrillation/Flutter
Dosage in pediatric patients is based on pharmacokinetic data; safety and efficacy not evaluated in this population.1 402 403 404 Take the same precautions as in adults.1 402 403 404 Individualize dosage based on clinical response, heart rate, and QTc.1 402 404
There are no studies of IV sotalol in pediatric patients.402
Oral
Children ≥2 years of age with normal renal function: Initially, 30 mg/m2 3 times daily (total daily dose of 90 mg/m2).1 402 403 404 May titrate dosage to maximum of 60 mg/m2 3 times daily (equivalent to total daily dose of 360 mg in adults).1 402 403 404 Allow ≥36 hours to elapse between dosage escalations to achieve steady-state concentrations.1 402 403 404
Children ≤2 years of age: Calculate dosage by multiplying the recommended initial dosage for children ≥2 years of age (i.e., 30 mg/m2 3 times daily) by an age-dependent factor obtained from manufacturer’s prescribing information.1 402 403 404 The age-dependent factor is approximately 0.3 in neonates 1 week old, 0.68 in infants 1 month of age, and 0.97 in infants 20 months of age.1 402 403 404 (See Table 2.) Use similar calculations for dosage increases.402 403 404
To obtain dosages for ages not mentioned in this table, see age/factor graph in manufacturer’s prescribing information
See age/factor graph in manufacturer’s prescribing information for age-dependent factor
|
Age |
Initial Dosage Calculation (dosage for children ≥2 years of age [30 mg/m2 3 times daily] multiplied by an age-dependent factor)1 402 403 404 |
|---|---|
|
Neonates about 1 week of age |
30 mg/m2 × 0.3 = 9 mg/m2 administered 3 times daily |
|
Infants 1 month of age |
30 mg/m2 × 0.68 = 20 mg/m2 administered 3 times daily |
|
Infants 20 months of age |
30 mg/m2 × 0.97 = 29.1 mg/m2 administered 3 times daily |
Adults
Life-threatening Ventricular Arrhythmias
Oral
Initially, 80 mg twice daily in adults with normal renal function (Clcr >60 mL/minute).1 403 404 405 May increase dosage in increments of 80 mg per day every 3 days if QTc <500 msec.1 403 404
Usual maintenance dosage: 160–320 mg daily in 2 or 3 divided doses;1 404 dosing >2 times a day usually not necessary.1 404
Dosages as high as 480–640 mg daily have been used in patients with refractory life-threatening arrhythmias; however, risk of arrhythmic events increases with increasing dosage.1 8 403 404 (See Proarrhythmic Effects under Cautions.)
IV
Equivalent IV doses of sotalol hydrochloride are lower than oral doses; corresponding IV doses are as follows: 75 mg for an oral dose of 80 mg, 112.5 mg for an oral dose of 120 mg, and 150 mg for an oral dose of 160 mg.402
Initially, 75 mg once or twice daily (depending on Clcr) by IV infusion over 5 hours.402 405 (See Renal Impairment under Dosage and Administration.) If desired response not achieved and drug is well tolerated without excessive QT interval prolongation, may increase dosage to 112.5 mg once or twice daily (depending on Clcr); manufacturer recommends that dosage be increased in increments of 75 mg daily every 3 days.402 Closely monitor ECG and QT interval during dose increases.402
Based on experience with oral sotalol hydrochloride, the usual therapeutic effect should be observed with IV dosages of 75–150 mg once or twice daily; however, patients with life-threatening refractory ventricular arrhythmias have received higher dosages (e.g., oral dosages of 240–320 mg once or twice daily corresponding to IV dosages of 225–300 mg once or twice daily).402
Atrial Fibrillation or Flutter
Oral
For maintenance of normal sinus rhythm in adults with atrial fibrillation or flutter who have normal renal function (Clcr >60 mL/minute): Initially, 80 mg twice daily.1 42 61 403 404 May increase dosage in increments of 80 mg per day every 3 days if QTc <500 msec.1 403 404
In a dose-response study, the most effective dosage was 120 mg once or twice daily.1 42 45 403 404 Some clinicians state that dosage may be increased up to a maximum of 160 mg twice daily (provided drug is well tolerated and QTc <500 msec).26 47 50 403
IV
Equivalent IV doses of sotalol hydrochloride are lower than oral doses; corresponding IV doses are as follows: 75 mg for an oral dose of 80 mg, 112.5 mg for an oral dose of 120 mg, and 150 mg for an oral dose of 160 mg.402
For maintenance of normal sinus rhythm in adults with atrial fibrillation or flutter: Initially, 75 mg once or twice daily (depending on Clcr) by IV infusion over 5 hours.402 (See Renal Impairment under Dosage and Administration.)
If desired response not achieved and drug is well tolerated without excessive QT interval prolongation, may increase dosage after at least 3 days to 112.5 mg once or twice daily (depending on Clcr).402 Closely monitor ECG and QT interval during dose increases.402
Based on experience with oral sotalol hydrochloride, the usual therapeutic effect should be observed with an IV dosage of 112.5 mg once or twice daily; however, manufacturer states that dosage may be increased up to 150 mg once or twice daily if necessary provided drug is well tolerated.402
Prescribing Limits
Pediatric Patients
Life-threatening Ventricular Arrhythmias or Atrial Fibrillation/Flutter
Oral
Children ≥2 years of age: Maximum of 60 mg/m2 3 times daily.1
Children ≤2 years of age: Reduce maximum dosage in children ≥2 years of age (i.e., 60 mg/m2 3 times daily) by an age-dependent factor obtained from manufacturer’s prescribing information.1 (See Dosage: Pediatric Patients, under Dosage and Administration.)
Adults
Atrial Fibrillation or Flutter
Oral
Some clinicians recommend maximum of 320 mg daily (160 mg twice daily);26 47 50 404 increased incidence of torsades de pointes with higher dosages.1 47 403 (See Proarrhythmic Effects under Cautions.)
Special Populations
Hepatic Impairment
Manufacturers make no specific dosage recommendations.1 402 403 404
Renal Impairment
Reduce dose or dosing frequency to minimize risk of proarrhythmia; as in patients with normal renal function, closely monitor QT interval and heart rate.1 26 402 403 404 (See Proarrhythmic Effects under Cautions.)
Modify dosing interval according to Clcr.1 402 403 404 In general, administer the initial oral adult dose of 80 mg and subsequent doses twice daily in adults with Clcr>60 mL/minute and once daily in adults with Clcr 40–60 mL/minute.402 403 Generally contraindicated in patients with Clcr<40 mL/minute.1 402 403 404 In patients with ventricular arrhythmias, some manufacturers recommend a dosing interval of 36–48 hours in adults with Clcr 10–29 mL/minute and individualized dosing in those with Clcr<10 mL/minute.1 404
Since elimination half-life is prolonged in patients with renal impairment, dosage increases generally should be made after administration of at least 5 doses at appropriate intervals.1 8 404
Dosage in children with renal impairment not established.1 404 However, reduced doses and increased dosing intervals recommended for all age groups with renal impairment.1 404
Sotalol is partially removed by dialysis; however, manufacturers make no dosing recommendations for patients undergoing dialysis.1 404
Geriatric Patients
Modification of dosage based on age alone is not necessary.1
Because geriatric patients may have decreased renal function and because patients with renal impairment may be at increased risk of sotalol-induced toxicity, monitor closely and adjust dosage accordingly.1 (See Renal Impairment under Dosage and Administration.)
Cautions for Sotalol
Contraindications
-
Bronchial asthma or related bronchospastic conditions.1 42 43 44 47 48 49 402 403 404
-
Sinus bradycardia (<50 bpm while awake).1 42 43 44 47 48 49 402 403 404
-
Sick sinus syndrome or second or third degree AV block unless a functioning pacemaker is present.1 42 43 44 45 47 48 49 402 403 404
-
Congenital or acquired long QT interval syndromes.1 42 43 44 47 48 49 402 403 404
-
Baseline QT interval >450 msec (some manufacturers state this is a contraindication only in patients being treated for atrial fibrillation or flutter).1 42 402 403 404
-
Clcr <40 mL/minute (some manufacturers state this is a contraindication only in patients being treated for atrial fibrillation or flutter).1 402 403 404
-
Known hypersensitivity to sotalol or any ingredient in the formulation.1 42 43 44 47 48 49 403 404
Warnings/Precautions
Warnings
Proarrhythmic Effects
Can cause serious ventricular arrhythmias, principally torsades de pointes, associated with prolonged QT interval; risk increases progressively with QT interval prolongation.1 6 8 28 402 403 404 (See Boxed Warning.)
Arrhythmogenic events occur not only when initiating therapy, but with every upward dosage adjustment.1 3 4 7 47 402 404
QT interval prolongation is dose related.1 402 403 404
Risk of torsades de pointes increases with decreased Clcr, female gender, larger doses, reduction of heart rate, hypokalemia,1 3 402 404 presence of sustained ventricular tachycardia, excessive QTc interval prolongation, history of cardiomegaly or heart failure.1 402 Decrease risk by adjusting dosage based on Clcr and monitoring ECG for excessive QT interval prolongation.1 402 404 Take appropriate precautions during administration.1 402 403 404 (See General under Dosage and Administration.)
Heart Failure
New onset or worsening heart failure may occur.1 403 404 Use contraindicated in patients with decompensated heart failure.1 403 404 (See Contraindications under Cautions.)
Monitor for signs and symptoms of heart failure and discontinue therapy if symptoms occur.1
Electrolyte Disturbances
Electrolyte abnormalities (e.g., hypokalemia or hypomagnesemia) may exaggerate the degree of QT interval prolongation and increase the risk of torsades de pointes.1 3 403 404 Use not recommended until these imbalances are corrected.1 42 45 48 403 404
Carefully monitor electrolyte and acid-base balance in patients with severe or prolonged diarrhea and in patients receiving diuretics concomitantly.1 45 47 50 402 403 404
Bradycardia
Potential bradycardia in patients treated for supraventricular arrhythmias; associated with increased risk of torsades de pointes.1 403 404
Abrupt Withdrawal of Therapy
Abrupt withdrawal may exacerbate angina symptoms and/or precipitate MI, particularly in patients with ischemic heart disease, or may precipitate thyroid storm in patients with thyroid disease.1 402 403 404
Avoid abrupt discontinuance.1 402 403 404 If possible, gradually decrease dosage over a period of 1–2 weeks when discontinuing therapy, particularly in patients with ischemic heart disease; monitor patients.1 402 403 404
If exacerbation of angina occurs or acute coronary insufficiency develops, initiate appropriate treatment (e.g., temporary use of another β-blocker).1 403 404
Bronchospastic Disease
Use contraindicated in patients with bronchial asthma or related bronchospastic conditions.1 402 403 404 (See Contraindications under Cautions.)
Use not recommended in patients with nonallergic bronchospasm (e.g., chronic bronchitis, emphysema);1 402 404 use smallest effective dosage to minimize inhibition of bronchodilation produced by endogenous or exogenous catecholamine stimulation of β2-adrenergic receptors.1 402 403 404
History of Anaphylactic Reactions
Possible increased reactivity to a variety of allergens; patients may be unresponsive to usual doses of epinephrine used to treat anaphylactic reactions.1 402 403 404
Surgery
Some controversy exists regarding use of β-blockers during surgery.34 402 Hypotension, bradycardia, and stroke have occurred; in addition, it is unclear whether such use confers mortality benefits or risks.34 35 402
Generally continue β-blockers during surgery in patients who are already receiving these drugs for a chronic condition.1 34 404 Consider risks versus benefits in individual patients.1 34 404
Hypotension
Hypotension reported;1 402 403 404 monitor BP in patients with marginal cardiac compensation.1 402 403 404
Diabetes Mellitus
Possible decreased signs and symptoms of acute hypoglycemia (e.g., tachycardia).1 402 404 May increase blood glucose concentrations and insulin requirements in diabetic patients.1 402 404
Sick Sinus Syndrome
Possible increased risk of torsades de pointes in patients with atrial fibrillation and sinus node dysfunction, especially after cardioversion.49 50 402 403 Use contraindicated in patients with sick sinus syndrome unless a functioning pacemaker is present due to risk of sinus bradycardia, sinus pause, or sinus arrest.1 45 48 402 403 (See Contraindications under Cautions.)
Thyroid Abnormalities
Signs of hyperthyroidism (e.g., tachycardia) may be masked.1 402 403 404
Possible thyroid storm if therapy is abruptly withdrawn.1 402 403 404 (See Abrupt Withdrawal of Therapy under Cautions.)
General Precautions
Other Precautions
Shares the toxic potentials of other nonselective β-adrenergic blocking agents; observe usual precautions of these agents.1 3 4 5 6 7 8
Specific Populations
Pregnancy
Lactation
Distributed into milk.1 402 403 404 Discontinue nursing or the drug.1 403 404
Pediatric Use
Safety and efficacy not established in children <18 years of age.1 26 402 403 404
Class III electrophysiologic and β-blocking effects, pharmacokinetics and the relationship between plasma concentrations and effects (e.g., QTc intervals, resting heart rate) have been evaluated in children 3 days to 12 years of age.1 402 403 404
Has been effective in a limited number of infants <3 months of age29 30 and children <18 years of age30 for supraventricular arrhythmias; 29 30 less effective for ventricular arrhythmias.30 Mild sinus bradycardia occurred in most infants;29 fatigue occurred in several children and required discontinuance in a few.30
Similar to adults, serious adverse events including death, torsades de pointes, other proarrhythmias, AV block, and bradycardia have been reported in infants and children; usual precautions in adults should also be observed in pediatric patients.1 402
Geriatric Use
Insufficient experience in geriatric patients to determine whether safety and efficacy in geriatric patients differ from safety and efficacy in younger adults; however clinical trials of sotalol included many patients >50 years of age.3 4 5 6 8
Overall risk of cardiac death was associated with increasing age in clinical trials.8
Monitor closely and adjust dosage accordingly due to greater frequency of decreased renal function and increased risk of toxicity observed in the elderly.1 403
Hepatic Impairment
Clearance of sotalol not altered by hepatic impairment.1 402 403 404
Renal Impairment
Clearance is decreased depending on degree of renal impairment.1 (See Special Populations under Pharmacokinetics.)
Dosage adjustments necessary based on degree of renal impairment.1 404 (See Renal Impairment under Dosage and Administration.)
Partially removed by dialysis;1 404 monitor closely for efficacy of arrhythmia control and adverse effects (changes in heart rate and/or QT interval).1
Common Adverse Effects
Common adverse effects based on use of oral sotalol: Sinus bradycardia (heart rate <50 bpm),1 3 4 5 28 402 arrhythmogenic effects,1 402 chest pain,1 3 28 402 palpitation,1 3 28 402 hypotension,1 402 fatigue,1 3 28 42 402 dizziness,1 3 28 42 asthenia,1 3 28 hyperhidrosis,1 402 lightheadedness,1 402 upper respiratory tract problems,1 visual problems,1 sleep problems,1 402 weakness,1 402 dyspnea,1 3 28 402 headache,1 402 cough,1 nausea,1 3 vomiting,1 3 402 diarrhea,1 402 abdominal pain,1 edema,402 extremity pain.402
Drug Interactions
Drugs metabolized by CYP isoenzymes do not alter the pharmacokinetics of sotalol; sotalol does not induce or inhibit any CYP isoenzymes.1 404
Specific Drugs
|
Drug or Test |
Interaction |
Comments |
|---|---|---|
|
Antacids (aluminum- or magnesium-containing) |
Decreased absorption of sotalol and reduced bradycardic effect1 403 404 |
Do not administer within 2 hours of sotalol;1 403 404 no effects on sotalol pharmacokinetics or pharmacodynamics observed when administered 2 hours after sotalol1 404 |
|
Antiarrhythmics, class Ia (e.g., disopyramide, quinidine, procainamide) |
May prolong refractoriness and increase risk of QT interval prolongation1 402 403 404 |
Concomitant use not recommended; withhold for at least 3 half-lives before initiating sotalol1 1 402 403 404 |
|
Antiarrhythmics, class Ib or Ic |
Withhold for at least 3 half-lives before initiating sotalol1 |
|
|
Antiarrhythmics, class II (β-blockers) |
Possible additive class II (β-adrenergic receptor blocking) effects1 404 |
|
|
Antiarrhythmics, class III (e.g., amiodarone) |
May prolong refractoriness and increase risk of QT interval prolongation1 402 403 404 |
Concomitant use not recommended;1 42 402 404 withhold for at least 3 half-lives before initiating sotalol1 402 403 404 |
|
Antidepressants, tricyclics |
||
|
Antidiabetic agents (oral) |
||
|
Calcium-channel blocking agents |
Possible additive effects on AV conduction or ventricular function; also potential for additive bradycardia and hypotensive effects1 402 403 404 |
|
|
Clonidine |
Increased risk of bradycardia; in addition, β-blockers may potentiate rebound hypertension that occasionally occurs after discontinuance of clonidine1 402 403 404 |
To reduce risk of rebound hypertension, withdraw sotalol several days before the gradual withdrawal of clonidine1 404 |
|
Digoxin |
Unclear if proarrhythmias are the result of interaction or presence of heart failure (known proarrhythmia risk factor)1 |
|
|
Hydrochlorothiazide |
No pharmacokinetic interaction observed1 |
|
|
Insulin |
May cause hyperglycemia;1 402 403 404 may mask hypoglycemic symptoms402 |
|
|
Macrolides (e.g., azithromycin, clarithromycin) |
||
|
Phenothiazines |
||
|
Quinolone antibiotics (e.g., ciprofloxacin, levofloxacin) |
||
|
β2-Receptor agonists (e.g., albuterol, terbutaline, isoproterenol) |
Increased dosages of β2-receptor agonists may be required403 |
|
|
Reserpine |
Concomitant use may cause excessive decrease in resting sympathetic tone1 402 404 |
Monitor closely for evidence of hypotension or marked bradycardia that may produce syncope1 402 404 |
|
Warfarin |
Sotalol Pharmacokinetics
Absorption
Bioavailability
Peak plasma concentrations are reached in 2.5–4 hours following oral administration.1 403 404
Steady-state plasma concentrations are reached in 2–3 days following twice-daily oral administration.1 403 404
Food
Food reduces oral bioavailability by about 20%.1 403 404
Distribution
Extent
Crosses the placenta; found in amniotic fluid.402 404
Does not readily cross blood-brain barrier.1 403 404
Plasma Protein Binding
Does not bind to plasma proteins.1 403 404
Elimination
Metabolism
Elimination Route
Eliminated principally by glomerular filtration and tubular secretion; excreted principally unchanged in urine.1 403 404
Half-life
Special Populations
Renal impairment may reduce clearance.1 404 Elimination half-life in anuric patients may be prolonged (up to 69 hours).1 404 (See Renal Impairment under Dosage and Administration.)
In pediatric patients, half-life decreases with decreasing age <2 years of age.402
Stability
Storage
Oral
Solution
Commercially available oral solution: 20–25°C (may be exposed to 15–30°C).403
Extemporaneous oral solution: 15–30°C at ambient humidity; stable for ≤3 months after preparation.1
Tablets
Tight, light-resistant container at 20–25°C (may be exposed to 15–30°C).1 404
Parenteral
Injection
20–25°C.402 Protect from freezing and light.402
Compatibility
Parenteral
Solution Compatibility402
|
Compatible |
|---|
|
Dextrose 5% |
|
Ringer’s injection, lactated |
|
Sodium chloride 0.9% |
Actions
-
Inhibits response to adrenergic stimuli by competitively blocking β1-adrenergic receptors within the myocardium and β2-adrenergic receptors within bronchial and vascular smooth muscle.2 7 8
-
Exhibits antiarrhythmic activity characteristic of class II antiarrhythmic agents.1 2 7 8 404
-
Does not exhibit membrane-stabilizing activity,1 8 but exhibits electrophysiologic effects characteristic of class III antiarrhythmic agents (e.g., prolongs repolarization and refractoriness without affecting conduction).1 2 7 8 12 13 14 15
-
Does not exhibit intrinsic sympathomimetic activity.8
-
Selectively inhibits the rapidly activating component of the potassium channel involved in repolarization of cardiac cells (i.e., the rapidly activated inward component of the delayed rectifier potassium current IKr) in vitro.12 13 14 15
-
Does not appear to block sodium channels at usual doses (although it may at relatively high doses).12 16 26 27
-
Racemic mixture of 2 optical isomers that both exhibit class III antiarrhythmic activity,1 7 11 14 15 but only the l-isomer exhibits β-blocking activity.1 7 11 14 404
Advice to Patients
-
If a dose is missed, importance of taking next scheduled dose at the usual time and not doubling the dose to make up for missed dose.1 403
-
Importance of patients immediately contacting their clinician if syncope, pre-syncopal symptoms, or cardiac palpitations occur.1 402 403 404
-
Importance of advising patients that their electrolytes and ECG will be monitored during treatment.1 404
-
Importance of informing patients (especially those with ischemic heart disease) not to interrupt or discontinue therapy without consulting clinician and to fill their prescriptions on time to avoid treatment interruption.1 404
-
Importance of informing patients not to take sotalol tablets or oral solution 2 hours before or after administration of an antacid containing aluminum oxide or magnesium hydroxide (e.g., Maalox, Mylanta).1 403 404
-
Importance of immediately reporting to their clinician any conditions, concomitant therapy (e.g., diuretics), and/or manifestations associated with altered electrolyte balance (e.g., severe or prolonged diarrhea, unusual sweating, vomiting, loss of appetite, excessive thirst).1 403 404
-
Importance of informing clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs, as well as any concomitant illnesses.1
-
Importance of women informing clinicians if they are or plan to become pregnant or plan to breast-feed.1
-
Importance of informing patients of other important precautionary information. (See Cautions.)
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
* available from one or more manufacturer, distributor, and/or repackager by generic (nonproprietary) name
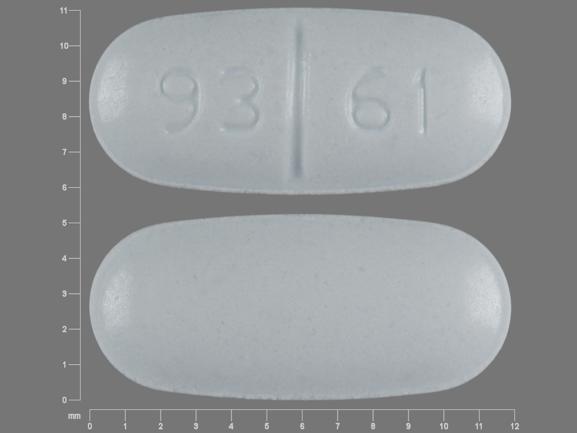
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Solution |
25 mg/5 mL |
Sotylize |
Arbor |
|
Tablets |
80 mg* |
Betapace (scored) |
Covis |
|
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
120 mg* |
Betapace (scored) |
Covis |
||
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
160 mg* |
Betapace (scored) |
Covis |
||
|
Betapace AF (scored) |
Covis |
|||
|
Sorine (scored) |
Upsher-Smith |
|||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
240 mg* |
Sorine (scored) |
Upsher-Smith |
||
|
Sotalol Hydrochloride Tablets (scored) |
||||
|
Parenteral |
Injection concentrate, for IV infusion |
15 mg/mL* |
Sotalol Hydrochloride Injection |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions April 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
† Off-label: Use is not currently included in the labeling approved by the US Food and Drug Administration.
References
1. Covis Pharma. Betapace and Betapace AF (sotalol hydrochloride) tablets prescribing information. Zug, Switzerland; 2016 May.
2. Bigger JT, Hoffman BF. Antiarrhythmic drugs. In: Gilman AG, Rall TW, Nies AS, Taylor P, eds. The pharmacological basis of therapeutics. 8th ed. New York: Pergamon Press; 1990:867.
3. Soyka LF, Wirtz C, Spangenberg RB. Clinical safety profile of sotalol in patients with arrhythmias. Am J Cardiol. 1990; 65:74-81A.
4. Kehoe RF, Zheutlin TA, Dunnington CS et al. Safety and efficacy of sotalol in patients with drug-refractory sustained ventricular tachyarrhythmias. Am J Cardiol. 1990; 65:58-64A.
5. Amiodarone vs Sotalol Study Group. Multicentre randomized trial of sotalol vs amiodarone for chronic malignant ventricular tachyarrhythmias. Eur Heart J. 1989; 10:685-94. https://pubmed.ncbi.nlm.nih.gov/2676535
6. Obel IWP, Jardine R, Haitus B et al. Efficacy of oral sotalol in reentrant ventricular tachycardia. Cardiovasc Drugs Ther. 1990; 4:613-8. https://pubmed.ncbi.nlm.nih.gov/2275891
7. Singh BN. Antiarrhythmic actions of DL-sotalol in ventricular and supraventricular arrhythmias. J Cardiovasc Pharmacol. 1992; 20(Suppl 2):S75-90. https://pubmed.ncbi.nlm.nih.gov/1279313
8. Berlex Laboratories. Betapace (sotalol hydrochloride) product monograph. Wayne, NJ; 1992 Dec.
9. Food and Drug Administration Orphan designations pursuant to Section 526 of the Federal Food and Cosmetic Act as amended by the Orphan Drug Act (P.L. 97-414), to June 28, 1996. Rockville, MD: 1996 Jul.
10. Julian DG, Prescott RJ, Jackson FS et al. Controlled trial of sotalol for one year after myocardial infarction. Lancet. 1982; 1:1142-7. https://pubmed.ncbi.nlm.nih.gov/6122937
11. Anon. Sotalol for cardiac arrhythmias. Med Lett Drugs Ther. 1993; 35:27-8. https://pubmed.ncbi.nlm.nih.gov/8450806
12. Mason JW, for the Electrophysiologic Study versus Electrocardiographic Monitoring Investigators. A comparison of seven antiarrhythmic drugs in patients with ventricular tachyarrhythmias. N Engl J Med. 1993; 329:452-8. https://pubmed.ncbi.nlm.nih.gov/8332150
13. Jurkiewicz NK, Sanguinetti MC. Rate-dependent prolongation of cardiac action potentials by a methanesulfonanilide class III antiarrhythmic agent: specific block of rapidly activating delayed rectifier K+ current by dofetilide. Circ Res. 1993; 72:75-83. https://pubmed.ncbi.nlm.nih.gov/8417848
14. Sanguinetti MC. Modulation of potassium channels by antiarrhythmic and antihypertensive drugs. Hypertension. 1992; 19:228-36. https://pubmed.ncbi.nlm.nih.gov/1548049
15. Sanguinetti MC, Jurkiewicz NK. Two components of cardiac delayed rectifier K+ current: differential sensitivity to block by class III antiarrhythmic agents. J Gen Physiol. 1990; 96:195-215. https://pubmed.ncbi.nlm.nih.gov/2170562 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2228985/
16. Singh BN, Vaughan Williams EM. A third class of anti-arrhythmic action: effects on atrial and ventricular intracellular potentials, and other pharmacological actions on cardiac muscle, of MJ 1999 and AH 3474. Br J Pharmacol. 1970; 39:675-87. https://pubmed.ncbi.nlm.nih.gov/5485144 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1702723/
17. The Cardiac Arrhythmia Suppression Trial (CAST) investigators. Preliminary report: effect of encainide and flecainide on mortality in a randomized trial of arrhythmia suppression after myocardial infarction. N Engl J Med. 1989; 321:406-12. https://pubmed.ncbi.nlm.nih.gov/2473403
18. Ruskin JN. The Cardiac Arrhythmia Suppression Trial (CAST). N Engl J Med. 1989; 321:386-8. https://pubmed.ncbi.nlm.nih.gov/2501683
19. Echt DS, Liebson PR, Mitchell LB et al. Mortality and morbidity in patients receiving encainide, flecainide, or placebo: the Cardiac Arrhythmia Suppression Trial. N Engl J Med. 1991; 324:781-8. https://pubmed.ncbi.nlm.nih.gov/1900101
20. Food and Drug Administration. Enkaid and Tambocor use in non-life-threatening arrhythmias halted. FDA Talk Paper. 1989 Apr 25.
21. Department of Health and Human Services. Background statement regarding encainide, flecainide, and moricizine. Bethesda, MD: National Institutes of Health, National Heart, Lung, and Blood Institute; 1989 Apr.
22. The Cardiac Arrhythmia Suppression Trial II investigators. Effect of the antiarrhythmic agent moricizine on survival after myocardial infarction. N Engl J Med. 1992; 327:227-33. https://pubmed.ncbi.nlm.nih.gov/1377359
26. Berlex Laboratories, Wayne, NJ: Personal communication.
27. Carmeliet E. Electrophysiologic and voltage clamp analysis of the effects of sotalol on isolated cardiac muscle and purkinje fibers. J Pharmacol Exp Ther. 1985; 323: 817-25.
28. MacNeil DJ, Davies RO, Deitchman D. Clinical safety profile of sotalol in the treatment of arrhythmias. Am J Cardiol. 1993; 72:44-50A.
29. Tipple M, Sandor G. Efficacy and safety of oral sotalol in early infancy. PACE Pacing Clin Electrophysiol. 1991; 14(11 Pt 2):2062-5. https://pubmed.ncbi.nlm.nih.gov/1721225
30. Maragnès P, Tipple M, Fournier A. Effectiveness of oral sotalol for treatment of pediatric arrhythmias. Am J Cardiol. 1992; 69:751-4. https://pubmed.ncbi.nlm.nih.gov/1546649
31. O’Hare MF, Murnaghan GA, Russell CJ et al. Sotalol as a hypotensive agent in pregnancy. Br J Obstet Gynaecol. 1980; 87:814-20. https://pubmed.ncbi.nlm.nih.gov/7426541
32. Wagner X, Jouglard J, Moulin M et al. Coadministration of flecainide acetate and sotalol during pregnancy: lack of teratogenic effects, passage across the placenta, and excretion in human breast milk. Am Heart J. 1990; 119:700-2. https://pubmed.ncbi.nlm.nih.gov/1689933
33. Hackett LP, Wojnar-Horton RE, Dusci LJ et al. Excretion of sotalol in breast milk. Br J Clin Pharmacol. 1990; 29:277-8. https://pubmed.ncbi.nlm.nih.gov/2306424 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1380099/
34. Fleisher LA, Fleischmann KE, Auerbach AD et al. 2014 ACC/AHA guideline on perioperative cardiovascular evaluation and management of patients undergoing noncardiac surgery: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014; 130:e278-333. https://pubmed.ncbi.nlm.nih.gov/25085961
35. POISE Study Group, Devereaux PJ, Yang H et al. Effects of extended-release metoprolol succinate in patients undergoing non-cardiac surgery (POISE trial): a randomised controlled trial. Lancet. 2008; 371:1839-47. https://pubmed.ncbi.nlm.nih.gov/18479744
37. Martin DE, Kammerer WS. The hypertensive surgical patient: controversies in management. Surg Clin North Am. 1983; 63:1017-33. https://pubmed.ncbi.nlm.nih.gov/6138862
40. Anon. Consensus recommendations for the management of chronic heart failure. On behalf of the membership of the advisory council to improve outcomes nationwide in heart failure. Part II. Management of heart failure: apporaches to the prevention of heart failure. Am J Cardiol. 1999; 83:9A-38A.
42. Benditt DG, Williams JH, Jin J et al. Maintenance of sinus rhythm with oral d,L-sotalol therapy in patients with symptomatic atrial fibrillation and/or flutter. Am J Cardiol. 1999; 84:270-7. https://pubmed.ncbi.nlm.nih.gov/10496434
43. Roy D, Talajic M, Dorian P et al. Amiodarone to prevent recurrence of atrial fibrillation. N Engl J Med. 2000; 342:913-20. https://pubmed.ncbi.nlm.nih.gov/10738049
44. Southworth MR, Zarembski D, Viana M et al. Comparison of sotalol versus quinidine for maintenance of sinus rhythm in patients with chronic atrial fibrillation. Am J Cardiol. 1999; 83:1629-32. https://pubmed.ncbi.nlm.nih.gov/10392866
45. De Paola AAV, Veloso HH. Efficacy and safety of sotalol versus quindine for the maintenance of sinus rhythm after conversion of atrial fibrillation. Am J Cardiol. 1999; 84:1033-7. https://pubmed.ncbi.nlm.nih.gov/10569659
47. Reimold SC, Cantillon CO, Friedman PL et al. Propafenone versus sotalol for suppression of recurrent atrial fibrillation. Am J Cardiol. 1993; 71:558-63. https://pubmed.ncbi.nlm.nih.gov/8438741
48. Anderson JL, Prystowsky EN. Sotalol: an important new antiarrhythmic. Am Heart J. 1999; 137:388-409. https://pubmed.ncbi.nlm.nih.gov/10047618
49. Chung MK, Schweikert RA, Wilkoff BL et al. Is hospital admission for initiation of antiarrhytmic therapy with sotalol for atrial arrhtymias required? Yield of in-hospital monitoring and prediction of risk for significant arrhtymia complications. J Am Coll Cardiol. 1998; 32:169-76. https://pubmed.ncbi.nlm.nih.gov/9669266
50. Marcus FI. Risks of initiating therapy with sotalol for treatment of atrial fibrillation. J Am Coll Cardiol. 1998; 32:177-80. https://pubmed.ncbi.nlm.nih.gov/9669267
51. Prystowsky EN, Benson W Jr, Fuster V et al. Management of patients with atrial fibrillation: a statement for healthcare professionals from the subcommittee on electrocardiography and electrophysiology, American Heart Association. Circulation. 1996; 93:1262-77. https://pubmed.ncbi.nlm.nih.gov/8653857
52. McClellan KJ, Markham A. Dofetilide: a review of its use in atrial fibrillation and atrial flutter. Drugs. 1999; 58:1043-59. https://pubmed.ncbi.nlm.nih.gov/10651390
53. Singh S, Berk M, Yellen L et al. Restoration and maintenance of sinus rhythm reduces the frequency and severity of symptoms associated with atrial fibrillation and flutter. Pacing Clin Electrophysiol. 1998; 21:813.
54. Prystowsky EN. Prespectives and controversies in atrial fibrillation. Am J Cardiol. 1998; 82(suppl. 4A):3I-6I. https://pubmed.ncbi.nlm.nih.gov/9737648
55. Reiffel JA. Selecting an antiarrhythmic agent for atrial fibrillation should be a patient-specific, data-driven decision. Am J Cardiol. 1998; 82(Suppl. 8A):72N-81N. https://pubmed.ncbi.nlm.nih.gov/9809904
56. Kalus JS, Mauro VF. Doefetilide: a class III-specific antiarrhythmic agent. Ann Pharmacother. 2000; 34:44-56. https://pubmed.ncbi.nlm.nih.gov/10669186
57. Pfizer. Tikosyn (dofetilide) capsules prescribing information. New York, NY; 1999 Nov.
58. Singh BN. Antiarrhythmic drugs: a reorientation in light of recent developments in the control of disorders of rhythm. Am J Cardiol. 1998; 81(Suppl. 6A):3D-13D. https://pubmed.ncbi.nlm.nih.gov/9537217
59. Waldo AL. Management of atrial fibrillation: the need for AFFIRMative action. Am J Cardiol. 1999; 84:698-700. https://pubmed.ncbi.nlm.nih.gov/10498142
60. Roden DM. Mechanisms and management of proarrhythmia. Am J Cardiol. 1998; 82(Suppl. 4A):49I-57I. https://pubmed.ncbi.nlm.nih.gov/9737654
61. Goldschlager N. Electrocardiography. In: Goldman L, Bennett JC, eds. Cecil textbook of medicine. 21st ed. Philadelphia: WB Saunders Company; 2000:185-91.
64. Fitton A, Sorkin EM. Sotalol: an udated review of its pharmacological properties and therapeutic use in cardiac arrhythmias. Drugs. 1993; 46:678-719. https://pubmed.ncbi.nlm.nih.gov/7506652
65. Thadani U. Beta blockers in hypertension. Am J Cardiol. 1983; 52:10-5D.
66. Conolly ME, Kersting F, Dollery CT. The clinical pharmacology of beta-adrenoceptor-blocking drugs. Prog Cardiovasc Dis. 1976; 19:203-34. https://pubmed.ncbi.nlm.nih.gov/10600
67. Shand DG. State-of-the-art: comparative pharmacology of the β-adrenoceptor blocking drugs. Drugs. 1983; 25(Suppl 2):92-9.
68. Breckenridge A. Which beta blocker? Br Med J. 1983; 286:1085-8. (IDIS 169422)
69. Anon. Choice of a beta-blocker. Med Lett Drugs Ther. 1986; 28:20-2. https://pubmed.ncbi.nlm.nih.gov/2869400
70. Wallin JD, Shah SV. β-Adrenergic blocking agents in the treatment of hypertension: choices based on pharmacological properties and patient characteristics. Arch Intern Med. 1987; 147:654-9. https://pubmed.ncbi.nlm.nih.gov/2881524
71. McDevitt DG. β-Adrenoceptor blocking drugs and partial agonist activity: is it clinically relevant? Drugs. 1983; 25:331-8.
72. McDevitt DG. Clinical significance of cardioselectivity: state-of-the-art. Drugs. 1983; 25(Suppl 2):219-26.
73. Frishman WH. β-Adrenoceptor antagonists: new drugs and new indications. N Engl J Med. 1981; 305:500-6. https://pubmed.ncbi.nlm.nih.gov/6114433
74. Thadani U, Davidson C, Chir B et al. Comparison of the immediate effects of five β-adrenoceptor-blocking drugs with different ancillary properties in angina pectoris. N Engl J Med. 1979; 300:750-5. https://pubmed.ncbi.nlm.nih.gov/581782
75. Lewis RV, McDevitt DG. Adverse reactions and interactions with β-adrenoceptor blocking drugs. Med Toxicol. 1986; 1:343-61. https://pubmed.ncbi.nlm.nih.gov/2878346
76. Frishman WH. Clinical differences between beta-adrenergic blocking agents: implications for therapeutic substitution. Am Heart J. 1987; 113:1190-8. https://pubmed.ncbi.nlm.nih.gov/2883867
300. Page RL, Joglar JA, Caldwell MA et al. 2015 ACC/AHA/HRS Guideline for the Management of Adult Patients With Supraventricular Tachycardia: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2016; 67:e27-e115.
301. January CT, Wann LS, Alpert JS et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2014; 64:e1-76. https://pubmed.ncbi.nlm.nih.gov/24685669
400. Link MS, Berkow LC, Kudenchuk PJ et al. Part 7: Adult Advanced Cardiovascular Life Support: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015; 132(18 Suppl 2):S444-64. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4771073/
401. Neumar RW, Otto CW, Link MS et al. Part 8: adult advanced cardiovascular life support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010; 122(18 Suppl 3):S729-67.
402. Academic Pharmaceuticals. Sotalol hydrochloride injection for intravenous use prescribing information. Lake Bluff, IL; 2014 Sept.
403. Arbor Pharmaceuticals. Sotylize (sotalol hydrochloride) oral solution prescribing information. Atlanta, GA; 2014 Oct.
404. Upsher-Smith Laboratories. Sorine (sotalol hydrochloride) tablets prescribing information. Maple Grove, MN; 2017 Jun.
405. Al-Khatib SM, Stevenson WG, Ackerman MJ, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation. 2017. DOI: 10.1161/CIR.0000000000000549
HID. ASHP. Handbook on injectable drugs. 19th ed. Bethesda, MD: American Society of Health-System Pharmacists, Inc; 2018.
Related/similar drugs
Frequently asked questions
More about sotalol
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (59)
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group III antiarrhythmics
- Breastfeeding
- En español