Rucaparib (Monograph)
Brand name: Rubraca
Drug class: Antineoplastic Agents
Introduction
Antineoplastic agent; an inhibitor of poly(adenosine diphosphate [ADP]-ribose) polymerase (PARP).
Uses for Rucaparib
Ovarian Cancer
Used for maintenance treatment of adults with deleterious germline or somatic BRCA-mutated recurrent epithelial ovarian, fallopian tube, or primary peritoneal cancer who are in complete or partial response to platinum-based chemotherapy; designated an orphan drug by FDA for this use.
American Society of Clinical Oncology (ASCO) guidelines state that PARP inhibitor monotherapy may be used for second-line or greater maintenance treatment in PARP inhibitor-naïve patients with epithelial ovarian cancer who have responded to platinum-based regimens, regardless of BRCA mutation status. However, FDA-labeled use for rucaparib maintenance therapy is restricted to patients with a tumor BRCA mutation.
Prostate Cancer
Used for the treatment of adults with deleterious germline or somatic BRCA-mutated metastatic castration-resistant prostate cancer previously treated with androgen receptor-directed therapy and a taxane-based chemotherapy. Accelerated approval based on objective response rate and duration of response. Continued approval may be contingent on verification and description of clinical benefit in confirmatory studies. FDA-approved companion diagnostic test required to confirm BRCA mutation status prior to initiation of therapy.
American Urological Association (AUA) guidelines recommend offering a PARP inhibitor to patients with confirmed or suspected deleterious germline or somatic homologous recombination repair (HRR) gene-mutated (including BRCA-mutated) metastatic castration-resistant prostate cancer following prior treatment with enzalutamide or abiraterone acetate, and/or a taxane-based chemotherapy.
Rucaparib Dosage and Administration
General
Pretreatment Screening
-
Confirm presence of deleterious germline and/or somatic BRCA mutation prior to initiation of rucaparib therapy. Consult FDA website for list of FDA-approved companion diagnostic tests ([Web]).
-
Obtain CBC at baseline.
-
Perform pregnancy testing for females of reproductive potential prior to starting therapy.
Patient Monitoring
-
Monitor CBC monthly during therapy.
Other General Considerations
-
Tachyphylaxis of nausea symptoms usually occurs during the first cycle of PARP inhibitor therapy, often without antiemetic therapy or dose reduction.
-
A light meal or snack prior to each dose of a PARP inhibitor may mitigate nausea.
-
If persistent nausea/vomiting, weight loss >5%, and/or reduction in performance status occurs in the absence of other etiology (e.g., bowel obstruction), ASCO recommends temporarily withholding therapy followed by dosage reduction.
Administration
Oral Administration
Administer orally twice daily without regard to meals.
If a dose is missed or vomited, the next dose should be taken at the regularly scheduled time. Do not replace vomited doses.
Dosage
Available as rucaparib camsylate; dosage expressed in terms of rucaparib.
Adults
Ovarian Cancer
Oral
600 mg (two 300-mg tablets) twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Prostate Cancer
Oral
600 mg (two 300-mg tablets) twice daily. Continue therapy until disease progression or unacceptable toxicity occurs.
Use with a gonadotropin-releasing hormone (GnRH) analog in patients who have not previously undergone bilateral orchiectomy.
Dosage Modification for Toxicity
If adverse reactions occur, consider interruption of therapy or dosage reduction.
If a first dosage reduction is necessary, reduce dosage to 500 mg twice daily.
If a second dosage reduction from 500 mg twice daily is necessary, reduce dosage to 400 mg twice daily.
If a third dosage reduction is necessary, reduce dosage to 300 mg twice daily.
Special Populations
Hepatic Impairment
Mild or moderate hepatic impairment (total bilirubin ≤3 times ULN or AST >ULN): Dosage adjustment not necessary.
Severe hepatic impairment (total bilirubin >3 times ULN with any AST): Not studied in this population; no specific dosage recommendations at this time.
Renal Impairment
Mild or moderate renal impairment (Clcr 30–89 mL/minute): Dosage adjustment not necessary.
Severe renal impairment (Clcr <30 mL/minute) or dialysis: Not studied in this population; no specific dosage recommendations at this time.
Geriatric Patients
No specific dosage recommendations at this time.
Cautions for Rucaparib
Contraindications
-
None.
Warnings/Precautions
Myelodysplastic Syndrome (MDS)/Acute Myeloid Leukemia (AML)
MDS and AML reported rarely; some cases were fatal. All patients had received previous chemotherapy with platinum-containing agents and/or other DNA-damaging antineoplastic agents. T
Monitor CBC at baseline and monthly thereafter. Delay initiation of rucaparib until hematologic toxicity caused by previous chemotherapy resolves to grade 1 or less.
If prolonged (>4 weeks) hematologic toxicity occurs, interrupt therapy or reduce dosage, and monitor CBC counts weekly until recovery to grade 1 or less.
If hematologic toxicity persists for >4 weeks following dosage modification or if MDS/AML is suspected, refer patient to a hematologist for further evaluation, including bone marrow analysis and cytogenetic testing of a blood sample. If MDS/AML is confirmed, discontinue rucaparib.
Fetal/Neonatal Morbidity and Mortality
May cause fetal harm based on mechanism of action and animal findings; embryotoxicity demonstrated in animals.
Avoid pregnancy during therapy. Verify pregnancy status prior to initiating rucaparib therapy.
Females of reproductive potential should use effective contraceptive methods while receiving rucaparib and for 6 months after the drug is discontinued. Males with female partners of reproductive potential or partners who are pregnant should use effective contraceptive methods while receiving rucaparib and for 3 months after the drug is discontinued.
Males should refrain from donating sperm while receiving rucaparib and for 3 months after the drug is discontinued.
If used during pregnancy or patient becomes pregnant, apprise of potential fetal hazard and risk for loss of the pregnancy.
Specific Populations
Pregnancy
May cause fetal harm.
Avoid pregnancy during therapy. Verify pregnancy status prior to initiating rucaparib therapy.
Lactation
Not known whether rucaparib is distributed into milk. Discontinue breast-feeding during therapy and for 2 weeks after drug discontinuance.
Females and Males of Reproductive Potential
May cause fetal harm. Verify pregnancy status prior to intiating rucaparib therapy.
Advise females of reproductive potential to use effective contraception while receiving rucaparib and for 6 months following the last dose.
Advise male patients with female partners of reproductive potential or partners who are pregnant to use effective contraception while receiving rucaparib and for 3 months following drug discontinuance.
Advise male patients to avoid donating sperm while receiving rucaparib and for 3 months following the last dose.
Pediatric Use
Safety and efficacy not established.
Geriatric Use
No overall differences in safety relative to younger patients, but increased sensitivity cannot be ruled out.
Hepatic Impairment
Mild hepatic impairment (total bilirubin <ULN with AST >ULN, or total bilirubin 1–1.5 times ULN with any AST) has no clinically meaningful effect on rucaparib pharmacokinetics. Dosage modification not required.
Systemic exposure to rucaparib increased by 45% in moderate hepatic impairment (total bilirubin 1.5—3 times ULN with any AST) compared to normal hepatic function. Dosage modification not required.
No data in patients with severe hepatic impairment (total bilirubin >3 times ULN with any AST).
Renal Impairment
Systemic exposure not substantially altered by mild or moderate renal impairment (Clcr ≥30 mL/minute); dosage adjustment not necessary.
Pharmacokinetics not established in patients with severe renal impairment (Clcr 15—29 mL/minute) or end-stage renal disease (Clcr <15 mL/minute).
Not studied in patients receiving dialysis.
Common Adverse Effects
Ovarian cancer (≥10%): Nausea, fatigue/asthenia, vomiting, anemia, dysgeusia, AST/ALT elevation, decreased appetite, diarrhea, thrombocytopenia, neutropenia, increased blood creatinine, dyspnea, dizziness, dyspepsia, photosensitivity reactions, leukopenia.
Metastatic castration-resistant prostate cancer (≥20%): Fatigue/asthenia, nausea, anemia, AST/ALT elevation, decreased appetite, rash, constipation, thrombocytopenia, vomiting, diarrhea.
Drug Interactions
Metabolized principally by CYP2D6 and, to a lesser extent, by CYP isoenzymes 1A2 and 3A4.
Inhibits CYP isoenzymes 1A2, 2C19, 2C9, 3A, 2C8, and 2D6, as well as UGT1A1. At clinically relevant concentrations, induces CYP1A2.
Inhibits organic anion transporting polypeptide (OATP) 1B1, OATP1B3, organic anion transporter (OAT) 1, OAT3, multidrug and toxic compound extrusion (MATE) 1, MATE2K, organic cation transporter (OCT) 1, OCT2, and multidrug resistance protein (MRP) 4. Does not inhibit MRP2, MRP3, or bile salt export pump (BSEP).
Substrate of P-glycoprotein (P-gp) and breast cancer resistance protein (BCRP), but not a substrate of OAT1, OAT3, OCT2, OATP1B1, or OATP1B3.
Drugs Metabolized by Hepatic Microsomal Enzymes
Substrates of CYP1A2, 3A, 2C9, or 2C19: Possible increased systemic exposure of substrate drugs and possible toxicity. If concomitant administration of CYP1A2, 3A, 2C9, and 2C19 substrate drugs with rucaparib is unavoidable, reduce substrate dosage in accordance with the drug's prescribing information.
Specific Drugs
|
Drug |
Interaction |
Comments |
|---|---|---|
|
Caffeine |
CYP1A2 substrate: Possible increased systemic exposure of substrate drug Caffeine: AUC of caffeine increased 2.6-fold |
Reduce dosage of caffeine in accordance with prescribing information if minimal concentration change could increase the frequency or severity of adverse reactions |
|
Digoxin |
Digoxin: AUC of digoxin increased 1.2-fold |
|
|
Hormonal contraceptives (ethinyl estradiol/levonorgestrel) |
CYP3A substrates: Possible increased systemic exposure of substrate drug Ethinyl estradiol/levonorgestrel: AUC increased 1.4 and 1.6-fold, respectively |
|
|
Midazolam |
CYP3A4 substrate: Possible increased systemic exposure of substrate drug Midazolam: AUC of midazolam increased 1.4-fold |
Reduce dosage of midazolam in accordance with prescribing information if minimal concentration change could increase the frequency or severity of adverse reactions |
|
Omeprazole |
CYP2C19 substrate: Possible increased systemic exposure of substrate drug Omeprazole: AUC of omeprazole increased 1.6-fold |
Reduce dosage of omeprazole in accordance with prescribing information if minimal concentration change could increase the frequency or severity of adverse reactions |
|
Proton-pump inhibitors |
No clinically meaningful effect on rucaparib exposure |
|
|
Rosuvastatin |
No clinically meaningful effect on rosuvatatin concentrations |
|
|
Warfarin |
CYP2C9 substrate: Possible increased systemic exposure of substrate drug Warfarin: AUC of warfarin increased by 1.5-fold |
Consider more frequent monitoring of INR Reduce dosage of warfarin in accordance with prescribing information if minimal concentration change could increase the frequency or severity of adverse reactions |
Rucaparib Pharmacokinetics
Absorption
Bioavailability
Pharmacokinetics are linear, time independent, and dose proportional over dosage range of 240–840 mg twice daily; mean systemic accumulation is 3.5- to 6.2-fold following repeated administration.
Median time to peak plasma concentrations is 1.9 hours following oral administration.
Mean absolute oral bioavailability is 36%.
Food
Administration with a high-fat meal decreased rate and modestly increased extent of absorption; time to peak plasma concentration delayed by 2.5 hours, and peak plasma concentration and AUC increased by 20 and 38%, respectively.
Special Populations
Mild hepatic impairment does not significantly affect pharmacokinetics of rucaparib.
Moderate hepatic impairment increased systemic exposure to rucaparib by 45%.
Mild to moderate renal impairment (Clcr ≥30 mL/minute) does not significantly affect pharmacokinetics of rucaparib.
Effects of severe renal impairment (Clcr 15—29 mL/minute, end-stage renal disease (Clcr<15 mL/minute), dialysis, and severe hepatic impairment on rucaparib pharmacokinetics not established.
Age (20—86 years), body weight (41—171 kg), sex, and race (white, Black, Asian) do not affect exposure to rucaparib.
Genetic polymorphisms of CYP2D6 (i.e., poor, intermediate, or ultrarapid metabolizer) or CYP1A2 (i.e., hyperinducers) do not substantially affect exposure to rucaparib.
Distribution
Extent
Not known whether rucaparib distributes into human milk.
Plasma Protein Binding
70%.
Elimination
Metabolism
Metabolized principally by CYP2D6 and, to a lesser extent, by CYP isoenzymes 1A2 and 3A4.
Oxidation, N-demethylation, N-methylation, and glucuronidation are major metabolic pathways.
Elimination Route
Unchanged drug accounts for 64% of plasma radioactivity.
Eliminated in feces (95% of recovered dose) and urine (45%).
Half-life
Terminal half-life: 26 hours.
Stability
Storage
Oral
Tablets
20–25°C (excursions permitted between 15–30°C).
Actions
-
Inhibits mammalian PARP enzymes, including PARP-1, PARP-2, and PARP-3. PARP enzymes are involved in normal cellular homeostasis, including DNA transcription, cell cycle regulation, and DNA repair.
-
Rucaparib-induced cytotoxicity may involve inhibition of PARP enzymatic activity and increased formation of PARP-DNA complexes, which result in disruption of cellular homeostasis and apoptosis.
-
PARP inhibitors, including rucaparib, appear to be selective for tumors cells harboring certain homologous recombination deficiencies (e.g., BRCA1 and BRCA2 mutations).
-
Reduces tumor growth of xenograft models of human cancer (with or without deficiencies in BRCA) in mice.
Advice to Patients
-
Advise patients to read the manufacturer's patient information.
-
If a dose is missed or vomited, take the next dose at the regularly scheduled time; do not take an extra dose to replace the missed or vomited dose.
-
Risk of MDS and AML. Inform a clinician if fatigue/asthenia, fever, weight loss, frequent infections, bruising, unusual bleeding (including hematuria or bloody stool), shortness of breath, abnormal CBC counts, or requirement for blood product transfusions occurs.
-
Importance of hematologic monitoring during rucaparib therapy.
-
Risk of photosensitivity reactions. Limit exposure to sunlight, wear protective clothing, and use sunscreen when exposure cannot be avoided.
-
Risk of fetal harm and pregnancy loss. Advise females of reproductive potential to avoid pregnancy and to use an effective method of contraception while receiving rucaparib and for 6 months following discontinuance of therapy. Advise males with female partners of reproductive potential or partners who are pregnant to use an effective method of contraception while receiving rucaparib and for 3 months following discontinuance of therapy. Advise males not to donate sperm while receiving rucaparib and for 3 months following discontinuance of therapy. Importance of women informing clinicians immediately if they are pregnant or become pregnant during therapy. If pregnancy occurs, advise pregnant women of potential risk to the fetus.
-
Advise women to avoid breast-feeding while receiving rucaparib and for 2 weeks following discontinuance of therapy.
-
Advise patients to inform their clinicians of existing or contemplated concomitant therapy, including prescription and OTC drugs and dietary or herbal supplements, as well as any concomitant illnesses.
-
Inform patients of other important precautionary information.
Additional Information
The American Society of Health-System Pharmacists, Inc. represents that the information provided in the accompanying monograph was formulated with a reasonable standard of care, and in conformity with professional standards in the field. Readers are advised that decisions regarding use of drugs are complex medical decisions requiring the independent, informed decision of an appropriate health care professional, and that the information contained in the monograph is provided for informational purposes only. The manufacturer’s labeling should be consulted for more detailed information. The American Society of Health-System Pharmacists, Inc. does not endorse or recommend the use of any drug. The information contained in the monograph is not a substitute for medical care.
Preparations
Excipients in commercially available drug preparations may have clinically important effects in some individuals; consult specific product labeling for details.
Please refer to the ASHP Drug Shortages Resource Center for information on shortages of one or more of these preparations.
Distribution of rucaparib is restricted. Contact manufacturer or consult the Rubraca Healthcare Provider website ([Web]) for specific availability information.
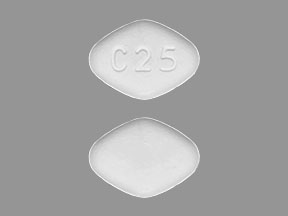
|
Routes |
Dosage Forms |
Strengths |
Brand Names |
Manufacturer |
|---|---|---|---|---|
|
Oral |
Tablets, film-coated |
200 mg (of rucaparib) |
Rubraca |
pharma& |
|
250 mg (of rucaparib) |
Rubraca |
pharma& |
||
|
300 mg (of rucaparib) |
Rubraca |
pharma& |
AHFS DI Essentials™. © Copyright 2025, Selected Revisions May 10, 2024. American Society of Health-System Pharmacists, Inc., 4500 East-West Highway, Suite 900, Bethesda, Maryland 20814.
Reload page with references included
Related/similar drugs
Frequently asked questions
More about rucaparib
- Check interactions
- Compare alternatives
- Reviews (1)
- Side effects
- Dosage information
- During pregnancy
- Drug class: PARP inhibitors
- Breastfeeding
- En español