Venclexta Dosage
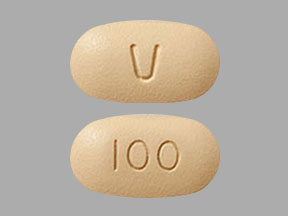
Generic name: Venetoclax 10mg; Venetoclax 50mg; Venetoclax 100mg
Dosage form: tablets
Drug class: Miscellaneous antineoplastics
Medically reviewed by Drugs.com. Last updated on Jul 12, 2024.
2.1 Important Safety Information
Assess patient-specific factors for level of risk of tumor lysis syndrome (TLS) and provide prophylactic hydration and anti-hyperuricemics to patients prior to first dose of VENCLEXTA to reduce risk of TLS.
2.2 Recommended Dosage for Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
VENCLEXTA dosing begins with a 5-week ramp-up. The 5-week ramp-up dosing schedule is designed to gradually reduce tumor burden (debulk) and decrease the risk of TLS.
VENCLEXTA 5-week Dose Ramp-Up Schedule
Administer VENCLEXTA according to the 5-week ramp-up dosing schedule to the recommended dosage of 400 mg orally once daily as shown in Table 1.
| VENCLEXTA Oral Daily Dose |
|
| Week 1 | 20 mg |
| Week 2 | 50 mg |
| Week 3 | 100 mg |
| Week 4 | 200 mg |
| Week 5 and beyond | 400 mg |
The CLL/SLL Starting Pack provides the first 4 weeks of VENCLEXTA according to the ramp-up schedule.
In Combination with Obinutuzumab
Start obinutuzumab administration at 100 mg on Cycle 1 Day 1, followed by 900 mg on Cycle 1 Day 2. Administer 1000 mg on Days 8 and 15 of Cycle 1 and on Day 1 of each subsequent 28-day cycle for a total of 6 cycles. Refer to the obinutuzumab prescribing information for additional dosing information.
On Cycle 1 Day 22, start VENCLEXTA according to the 5-week ramp-up dosing schedule (see Table 1). After completing the ramp-up phase on Cycle 2 Day 28, continue VENCLEXTA at a dose of 400 mg orally once daily from Cycle 3 Day 1 until the last day of Cycle 12.
In Combination with Rituximab
Start rituximab administration after the patient has completed the 5-week ramp-up dosing schedule for VENCLEXTA (see Table 1) and has received VENCLEXTA at the recommended dosage of 400 mg orally once daily for 7 days. Administer rituximab on Day 1 of each 28-day cycle for 6 cycles, at a dose of 375 mg/m2 intravenously for Cycle 1 and 500 mg/m2 intravenously for Cycles 2-6. Continue VENCLEXTA 400 mg orally once daily for 24 months from Cycle 1 Day 1 of rituximab.
Refer to the rituximab prescribing information for additional dosing information.
Monotherapy
The recommended dosage of VENCLEXTA is 400 mg once daily after completion of the 5-week ramp-up dosing schedule (see Table 1). Continue VENCLEXTA until disease progression or unacceptable toxicity.
2.3 Recommended Dosage for Acute Myeloid Leukemia
The recommended dosage and ramp-up of VENCLEXTA depends upon the combination agent. Follow the dosing schedule, including the 3-day or 4-day dose ramp-up, as shown in Table 2. Start VENCLEXTA administration on Cycle 1 Day 1 in combination with:
- Azacitidine 75 mg/m2 intravenously or subcutaneously once daily on Days 1-7 of each 28-day cycle; OR
- Decitabine 20 mg/m2 intravenously once daily on Days 1-5 of each 28-day cycle; OR
- Cytarabine 20 mg/m2 subcutaneously once daily on Days 1-10 of each 28-day cycle.
| VENCLEXTA Oral Daily Dose |
||
| Day 1 | 100 mg | |
| Day 2 | 200 mg | |
| Day 3 | 400 mg | |
| Days 4 and beyond | 400 mg orally once daily of each 28-day cycle in combination with azacitidine or decitabine |
600 mg orally once daily of each 28-day cycle in combination with low-dose cytarabine |
Continue VENCLEXTA, in combination with azacitidine or decitabine or low-dose cytarabine, until disease progression or unacceptable toxicity.
Refer to Clinical Studies (14.2) and Prescribing Information for azacitidine, decitabine, or cytarabine for additional dosing information.
2.4 Risk Assessment and Prophylaxis for Tumor Lysis Syndrome
Patients treated with VENCLEXTA may develop tumor lysis syndrome (TLS). Refer to the appropriate section below for specific details on management. Assess patient-specific factors for level of risk of TLS and provide prophylactic hydration and anti-hyperuricemics to patients prior to first dose of VENCLEXTA to reduce risk of TLS.
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
VENCLEXTA can cause rapid reduction in tumor and thus poses a risk for TLS in the initial 5-week ramp-up phase. Changes in blood chemistries consistent with TLS that require prompt management can occur as early as 6 to 8 hours following the first dose of VENCLEXTA and at each dose increase. TLS can also occur upon resumption of VENCLEXTA following a dosage interruption. See Table 4 and Table 5 for dose modifications of VENCLEXTA after interruption.
The risk of TLS is a continuum based on multiple factors, particularly reduced renal function (creatinine clearance [CLcr] <80 mL/min) and tumor burden; splenomegaly may also increase the risk of TLS.
Perform tumor burden assessments, including radiographic evaluation (e.g., CT scan), assess blood chemistry (potassium, uric acid, phosphorus, calcium, and creatinine) in all patients and correct pre-existing abnormalities prior to initiation of treatment with VENCLEXTA. The risk may decrease as tumor burden decreases.
Table 3 below describes the recommended TLS prophylaxis and monitoring during VENCLEXTA treatment based on tumor burden determination from clinical trial data. Consider all patient comorbidities before final determination of prophylaxis and monitoring schedule. Reassess the risk of TLS when reinitiating VENCLEXTA after a dosage interruption lasting more than 1 week during the ramp-up phase, or more than 2 weeks after completion of ramp-up. Institute prophylaxis and monitoring as needed.
| Tumor Burden | Prophylaxis | Blood Chemistry Monitoringc,d |
||
| Hydrationa | Anti- hyperuricemicsb |
Setting and Frequency of Assessments |
||
| Low | All LN <5 cm AND ALC <25 x109/L |
Oral (1.5 to 2 L) |
Allopurinol | Outpatient
|
| Medium | Any LN 5 to <10 cm OR ALC ≥25 x109/L |
Oral (1.5 to 2 L) and consider additional intravenous |
Allopurinol | Outpatient
|
| High | Any LN ≥10 cm OR ALC ≥25 x109/L AND any LN ≥5 cm |
Oral (1.5 to 2 L) and intravenous (150 to 200 mL/hr as tolerated) |
Allopurinol; consider rasburicase if baseline uric acid is elevated | In hospital
|
| ALC = absolute lymphocyte count; CLcr = creatinine clearance; LN = lymph node. aAdminister intravenous hydration for any patient who cannot tolerate oral hydration. bStart allopurinol or xanthine oxidase inhibitor 2 to 3 days prior to initiation of VENCLEXTA. cEvaluate blood chemistries (potassium, uric acid, phosphorus, calcium, and creatinine); review in real time. dFor patients at risk of TLS, monitor blood chemistries at 6 to 8 hours and at 24 hours at each subsequent ramp-up dose. |
||||
Acute Myeloid Leukemia
- All patients should have white blood cell count less than 25 × 109/L prior to initiation of VENCLEXTA. Cytoreduction prior to treatment may be required.
- Prior to first VENCLEXTA dose, provide all patients with prophylactic measures including adequate hydration and anti-hyperuricemic agents and continue during ramp-up phase.
- Assess blood chemistry (potassium, uric acid, phosphorus, calcium, and creatinine) and correct pre-existing abnormalities prior to initiation of treatment with VENCLEXTA.
- Monitor blood chemistries for TLS at pre-dose, 6 to 8 hours after each new dose during ramp-up, and 24 hours after reaching final dose.
- For patients with risk factors for TLS (e.g., circulating blasts, high burden of leukemia involvement in bone marrow, elevated pretreatment lactate dehydrogenase [LDH] levels, or reduced renal function), consider additional measures, including increased laboratory monitoring and reducing VENCLEXTA starting dose.
2.5 Dosage Modifications for Adverse Reactions
Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma
The recommended dosage modifications for VENCLEXTA for adverse reactions are provided in Table 4 and the recommended dose reductions for VENCLEXTA for adverse reactions are provided in Table 5.
For patients having a dosage interruption lasting more than 1 week during the ramp-up phase, or more than 2 weeks after completion of ramp-up, reassess for risk of TLS to determine if reinitiation with a reduced dose is necessary (e.g., all or some levels of the dose ramp-up schedule).
| Adverse Reaction | Occurrence | Dosage Modification |
| Tumor Lysis Syndrome | ||
| Blood chemistry changes or symptoms suggestive of TLS | Any | Withhold the next day’s dose. If resolved within 24 to 48 hours of last dose, resume at same dose. |
| For any blood chemistry changes requiring more than 48 hours to resolve, resume at reduced dose (see Table 5). | ||
| For any events of clinical TLS,b resume at reduced dose following resolution (see Table 5). | ||
| Non-Hematologic Adverse Reactions | ||
| Grade 3 or 4 non-hematologic toxicities | 1st occurrence | Interrupt VENCLEXTA. Upon resolution to Grade 1 or baseline level, resume VENCLEXTA at the same dose. |
| 2nd and subsequent occurrences | Interrupt VENCLEXTA. Follow dose reduction guidelines in Table 5 when resuming treatment with VENCLEXTA after resolution. A larger dose reduction may occur at the discretion of the physician. |
|
| Hematologic Adverse Reactions | ||
| Grade 3 neutropenia with infection or fever; or Grade 4 hematologic toxicities (except lymphopenia) | 1st occurrence | Interrupt VENCLEXTA. Upon resolution to Grade 1 or baseline level, resume VENCLEXTA at the same dose. |
| 2nd and subsequent occurrences | Interrupt VENCLEXTA. Follow dose reduction guidelines in Table 5 when resuming treatment with VENCLEXTA after resolution. A larger dose reduction may occur at the discretion of the physician. |
|
| Consider discontinuing VENCLEXTA for patients who require dose reductions to less than 100 mg for more than 2 weeks. aAdverse reactions were graded using NCI CTCAE version 4.0. bClinical TLS was defined as laboratory TLS with clinical consequences such as acute renal failure, cardiac arrhythmias, or sudden death and/or seizures. |
||
| Dose at Interruption, mg | Restart Dose, mga,b |
| 400 | 300 |
| 300 | 200 |
| 200 | 100 |
| 100 | 50 |
| 50 | 20 |
| 20 | 10 |
| aDuring the ramp-up phase, continue the reduced dose for 1 week before increasing the dose. bIf a dosage interruption lasts more than 1 week during the ramp-up phase or more than 2 weeks after completion of ramp-up, reassess the risk of TLS and determine if reinitiation at a reduced dosage is necessary. |
|
Acute Myeloid Leukemia
Monitor blood counts frequently through resolution of cytopenias. Dose modification and interruptions for cytopenias are dependent on remission status. Dose modifications of VENCLEXTA for adverse reactions are provided in Table 6.
| Adverse Reaction | Occurrence | Dosage Modification |
| Hematologic Adverse Reactions | ||
| Grade 4 neutropenia with or without fever or infection; or Grade 4 thrombocytopenia | Occurrence prior to achieving remissiona | In most instances, do not interrupt VENCLEXTA in combination with azacitidine, decitabine, or low-dose cytarabine due to cytopenias prior to achieving remission. |
| First occurrence after achieving remission and lasting at least 7 days | Delay subsequent cycle of VENCLEXTA in combination with azacitidine, decitabine, or low-dose cytarabine and monitor blood counts. Upon resolution to Grade 1 or 2, resume VENCLEXTA at the same dose in combination with azacitidine, decitabine, or low-dose cytarabine. |
|
| Subsequent occurrences in cycles after achieving remission and lasting 7 days or longer | Delay subsequent cycle of VENCLEXTA in combination with azacitidine, or decitabine, or low-dose cytarabine and monitor blood counts. Upon resolution to Grade 1 or 2, resume VENCLEXTA at the same dose in combination with azacitidine, decitabine, or low-dose cytarabine, and reduce VENCLEXTA duration by 7 days during each of the subsequent cycles, such as 21 days instead of 28 days. |
|
| Non-Hematologic Adverse Reactions | ||
| Grade 3 or 4 non-hematologic toxicities | Any occurrence | Interrupt VENCLEXTA if not resolved with supportive care. Upon resolution to Grade 1 or baseline level, resume VENCLEXTA at the same dose. |
| aRecommend bone marrow evaluation. | ||
2.6 Dosage Modifications for Drug Interactions
Strong or Moderate CYP3A Inhibitors or P-gp Inhibitors
Table 7 describes VENCLEXTA contraindication or dosage modification based on concomitant use with a strong or moderate CYP3A inhibitor or a P-gp inhibitor at initiation, during, or after the ramp-up phase.
Resume the VENCLEXTA dosage that was used prior to concomitant use of a strong or moderate CYP3A inhibitor or a P-gp inhibitor 2 to 3 days after discontinuation of the inhibitor.
| Coadministered Drug |
Initiation and Ramp-Up Phase |
Steady Daily Dose (After Ramp-Up Phase)a |
|
| Posaconazole | CLL/SLL | Contraindicated | Reduce VENCLEXTA dose to 70 mg. |
| AML | Day 1 – 10 mg Day 2 – 20 mg Day 3 – 50 mg Day 4 – 70 mg |
||
| Other strong CYP3A inhibitor |
CLL/SLL | Contraindicated | Reduce VENCLEXTA dose to 100 mg. |
| AML | Day 1 – 10 mg Day 2 – 20 mg Day 3 – 50 mg Day 4 – 100 mg |
||
| Moderate CYP3A inhibitor |
Reduce the VENCLEXTA dose by at least 50%. | ||
| P-gp inhibitor | |||
| aIn patients with CLL/SLL, consider alternative medications or reduce the VENCLEXTA dose as described in Table 7. | |||
2.7 Dosage Modifications for Patients with Severe Hepatic Impairment
Reduce the VENCLEXTA once daily dose by 50% for patients with severe hepatic impairment (Child-Pugh C); monitor these patients more closely for adverse reactions.
2.8 Administration
Instruct patients of the following:
- Take VENCLEXTA with a meal and water.
- Take VENCLEXTA at approximately the same time each day.
- Swallow VENCLEXTA tablets whole. Do not chew, crush, or break tablets prior to swallowing.
The recommended dosage of VENCLEXTA may be delivered using any of the approved tablet strengths (e.g., patients can take 2 x 50 mg tablets or 10 x 10 mg tablets instead of 1 x 100 mg tablet as needed).
If the patient misses a dose of VENCLEXTA within 8 hours of the time it is usually taken, instruct the patient to take the missed dose as soon as possible and resume the normal daily dosing schedule. If a patient misses a dose by more than 8 hours, instruct the patient not to take the missed dose and resume the usual dosing schedule the next day.
If the patient vomits following dosing, instruct the patient to not take an additional dose that day and to take the next prescribed dose at the usual time.
Frequently asked questions
- Is Venclexta (venetoclax) chemotherapy?
- How effective is Venclexta?
- How long do you take Venclexta for?
- Can Venclexta be used for Multiple Myeloma?
- How is Venclexta (venetoclax) used for AML?
- How does Venclexta work?
More about Venclexta (venetoclax)
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (11)
- Drug images
- Side effects
- Patient tips
- During pregnancy
- FDA approval history
- Drug class: miscellaneous antineoplastics
- Breastfeeding
Patient resources
Professional resources
Related treatment guides
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.