Flecainide Disease Interactions
There are 5 disease interactions with flecainide.
Antiarrhythmics (applies to flecainide) cardiovascular dysfunction
Major Potential Hazard, Low plausibility. Applicable conditions: Hypotension, Congestive Heart Failure
Antiarrhythmic agents can induce severe hypotension (particularly with IV administration) or induce or worsen congestive heart failure (CHF). Patients with primary cardiomyopathy or inadequately compensated CHF are at increased risk. Antiarrhythmic agents should be administered cautiously and dosage and/or frequency of administration modified in patients with hypotension or adequately compensated CHF. Alternative therapy should be considered unless these conditions are secondary to cardiac arrhythmia.
Flecainide (applies to flecainide) sinus-AV node dysfunction
Major Potential Hazard, High plausibility. Applicable conditions: Heart Block
The use of flecainide is contraindicated in patients with cardiogenic shock, second- or third-degree AV block or right bundle-branch block when associated with a left hemiblock(bifascicular block) in the absence of a functional artificial pacemaker, or congenital QT prolongation. Therapy with flecainide should be administered with extreme caution in patients with sick sinus syndrome or bradycardia-tachycardia syndrome due to the risk of sinus bradycardia, pause or arrest.
Antiarrhythmics (applies to flecainide) electrolyte imbalance
Moderate Potential Hazard, High plausibility. Applicable conditions: Hyperkalemia, Hypokalemia, Magnesium Imbalance
Electrolyte imbalance can alter the therapeutic effectiveness of antiarrhythmic agents. Hypokalemia and hypomagnesemia can reduce the effectiveness of antiarrhythmic agents. In some cases, these disorders can exaggerate the degree of QTc prolongation and increase the potential for torsade de pointes. Hyperkalemia can potentiate the toxic effects of antiarrhythmic agents. Electrolyte imbalance should be corrected prior to initiating antiarrhythmic therapy. Clinical monitoring of cardiac function and electrolyte concentrations is recommended.
Flecainide (applies to flecainide) hepatic dysfunction
Moderate Potential Hazard, High plausibility. Applicable conditions: Liver Disease
Since flecainide elimination from plasma can be markedly slower in patients with significant hepatic impairment, flecainide should not be used in such patients unless the potential benefits clearly outweigh the risks. If used, frequent and early plasma level monitoring is required to guide dosage. Additionally, dosage increases should be made very cautiously when plasma levels have plateaued (after more than four days).
Flecainide (applies to flecainide) renal dysfunction
Moderate Potential Hazard, High plausibility.
Flecainide is primarily eliminated by the kidney. Approximately 30% (10% to 50%) of flecainide is excreted in the urine unchanged. The serum concentration of flecainide is increased and the half-life prolonged in patients with renal impairment. Rare conditions such as a strict vegetarian diet or renal tubular acidosis that significantly increase the urinary pH slow the urinary elimination of flecainide. Adjustment of dosage is necessary and modification should be based on the degree of renal impairment. Clinical monitoring of cardiac function (ECG) and renal function is recommended.
Switch to professional interaction data
Flecainide drug interactions
There are 372 drug interactions with flecainide.
Flecainide alcohol/food interactions
There is 1 alcohol/food interaction with flecainide.
More about flecainide
- flecainide consumer information
- Check interactions
- Compare alternatives
- Pricing & coupons
- Reviews (179)
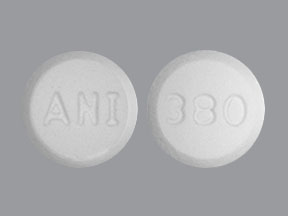
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Support group
- Drug class: group I antiarrhythmics
- Breastfeeding
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.