Seglentis Disease Interactions
There are 21 disease interactions with Seglentis (celecoxib / tramadol).
- Asthma
- Fluid retention
- GI toxicity
- Rash
- Renal toxicities
- Thrombosis
- Gastrointestinal obstruction
- Acute alcohol intoxication
- Drug dependence
- Respiratory depression
- Anemia
- Hepatotoxicity
- Hyperkalemia
- Gastrointestinal conditions
- Hypoglycemia
- Hypotension
- Intracranial pressure
- Liver disease
- Renal dysfunction
- Seizure disorders
- Suicidal
NSAIDs (applies to Seglentis) asthma
Major Potential Hazard, Moderate plausibility.
Nonsteroidal anti-inflammatory drugs (NSAIDs) are contraindicated in patients with history of asthma, urticaria, or other allergic-type reactions after taking aspirin or other NSAIDs; severe, sometimes fatal, anaphylactic reactions to NSAIDs have been reported in such patients. A subpopulation of patients with asthma may have aspirin-sensitive asthma which may include chronic rhinosinusitis complicated by nasal polyps, severe potentially fatal bronchospasm, and/or intolerance to aspirin and other NSAIDs. Since cross-reactivity between aspirin and other NSAIDs has been reported in such aspirin-sensitive patients, therapy with any NSAID should be avoided in patients with this form of aspirin sensitivity. NSAIDs should be used with caution in patients with preexisting asthma (without known aspirin sensitivity), and these patients should be monitored for changes in the signs and symptoms of asthma.
NSAIDs (applies to Seglentis) fluid retention
Major Potential Hazard, Moderate plausibility. Applicable conditions: Congestive Heart Failure, Hypertension
Fluid retention and edema have been reported in association with the use of nonsteroidal anti-inflammatory drugs (NSAIDs), including some topical formulations. NSAIDs (including topicals) can lead to new onset of hypertension or worsening of preexisting hypertension, either of which can contribute to the increased incidence of cardiovascular events. NSAIDs should be used with caution in patients with preexisting fluid retention, hypertension, or history of heart failure. NSAIDs should be avoided in patients with severe heart failure unless the benefits are expected to outweigh the risk of worsening heart failure; if an NSAID is used in such patients, they should be monitored for signs of worsening heart failure. Blood pressure and cardiovascular status should be monitored closely during the initiation of NSAID treatment and throughout the course of therapy.
NSAIDs (applies to Seglentis) GI toxicity
Major Potential Hazard, Moderate plausibility. Applicable conditions: Smoking, Duodenitis/Gastritis, Colitis/Enteritis (Noninfectious), History - Peptic Ulcer, Gastrointestinal Perforation, Alcoholism, Peptic Ulcer, Colonic Ulceration, Gastrointestinal Hemorrhage
Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause serious gastrointestinal (GI) adverse events including inflammation, bleeding, ulceration, and perforation of the esophagus, stomach, small intestine, or large intestine, which can be fatal. These serious adverse events can develop at any time, with or without warning symptoms. NSAIDs should be used with caution in patients with history of peptic ulcer disease and/or GI bleeding, as these patients had a greater than 10-fold increased risk for developing a GI bleed compared to patients without these risk factors. Caution is also advised if NSAIDs are prescribed to patients with other factors that increase risk of GI bleeding, such as: prolonged NSAID therapy; concomitant use of oral corticosteroids, antiplatelet agents (e.g., aspirin), anticoagulants, selective serotonin reuptake inhibitors; alcohol use; smoking; history of gastrointestinal surgery or anastomosis, older age; poor general health status; and advanced liver disease and/or coagulopathy. Particular vigilance is necessary when treating older adult or debilitated patients since most postmarketing reports of fatal GI events occurred in these patients.
NSAIDs (applies to Seglentis) rash
Major Potential Hazard, Moderate plausibility. Applicable conditions: Dermatitis - Drug-Induced
Nonsteroidal anti-inflammatory drugs (NSAIDs) can cause serious skin adverse reactions (e.g., Stevens-Johnson syndrome, toxic epidermal necrolysis, and exfoliative dermatitis), which can be fatal. NSAIDs can also cause fixed drug eruption, and may present as generalized bullous fixed drug eruption, which can be life-threatening. These serious events may occur without warning. Patients should be advised to discontinue the NSAID and seek medical attention promptly at the first sign of skin rash or any other sign of hypersensitivity. NSAIDs are contraindicated in patients with previous serious skin reactions to these drugs.
NSAIDs (applies to Seglentis) renal toxicities
Major Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease, Congestive Heart Failure, Renal Dysfunction, Dehydration, Hyponatremia
Long-term use of nonsteroidal anti-inflammatory drugs (NSAIDs) has resulted in renal papillary necrosis and other renal injury. Renal toxicity has been seen in patients in whom renal prostaglandins have a compensatory role in the maintenance of renal perfusion; in such patients, NSAIDs may cause a dose-dependent reduction in prostaglandin synthesis and, secondarily, in renal blood flow, which may precipitate overt renal decompensation. Patients at greatest risk for this reaction include those with impaired renal function, dehydration, hypovolemia, heart failure, liver dysfunction; those taking diuretics, angiotensin-converting enzyme inhibitors, or angiotensin receptor blockers; and older adult patients. Discontinuation of NSAID therapy generally leads to recovery to the pretreatment state. No information is available regarding NSAID use in patients with advanced renal disease; the renal effects of NSAIDs may hasten the progression of renal dysfunction in patients with preexisting renal disease. Volume status should be corrected in dehydrated or hypovolemic patients prior to initiating treatment. Renal function should be monitored in patients with renal or liver dysfunction, heart failure, dehydration, or hypovolemia during therapy. NSAIDs should be avoided in patients with advanced renal disease unless the benefits are expected to outweigh the risk of worsening renal function; if an NSAID is used in such patients, they should be monitored for signs of worsening renal function.
NSAIDs (applies to Seglentis) thrombosis
Major Potential Hazard, Moderate plausibility. Applicable conditions: Ischemic Heart Disease, History - Myocardial Infarction, Cerebrovascular Insufficiency, History - Cerebrovascular Disease
Nonsteroidal anti-inflammatory drugs (NSAIDs) cause an increased risk of serious cardiovascular thrombotic events, including myocardial infarction and stroke, which can be fatal. This risk may occur early in treatment and may increase with duration of use. Clinical trials of several cyclooxygenase-2 (COX-2) selective and nonselective NSAIDs of up to 3 years duration have supported this increased risk. It is unclear from available data if the risk for cardiovascular thrombotic events is similar for all NSAIDs. Therapy with NSAIDs should be administered cautiously in patients with a history of cardiovascular or cerebrovascular disease. Patients should be treated with the lowest effective dosage for the shortest duration necessary. Appropriate antiplatelet therapy should be administered to patients requiring cardioprotection; however, there is no consistent evidence that concurrent use of aspirin mitigates the increased risk of serious cardiovascular thrombotic events associated with NSAID use, while the risk of serious gastrointestinal events is increased. Physicians and patients should remain alert for the development of adverse cardiovascular events throughout the entire duration of therapy, even without prior cardiovascular symptoms. Patients should be advised to promptly seek medical attention if they experience symptoms of cardiovascular thrombotic events (including chest pain, shortness of breath, weakness, or slurring of speech).
NSAIDs are contraindicated in the setting of coronary artery bypass graft (CABG) surgery. Two large clinical trials of a COX-2 selective NSAID for the treatment of pain in the first 10 to 14 days following CABG surgery found an increased incidence of myocardial infarction and stroke.
The use of NSAIDs should be avoided in patients with a recent myocardial infarction unless the benefits are expected to outweigh the risk of recurrent cardiovascular thrombotic events. If an NSAID is used in patients with a recent myocardial infarction, they should be monitored for signs of cardiac ischemia.
Opioid agonists (applies to Seglentis) gastrointestinal obstruction
Major Potential Hazard, Moderate plausibility.
Opioid analgesics are contraindicated in patients with known or suspected gastrointestinal obstruction, including paralytic ileus.
Tramadol (applies to Seglentis) acute alcohol intoxication
Major Potential Hazard, High plausibility. Applicable conditions: Alcoholism
The CNS depressant effects of tramadol may be additive with those of alcohol and may lead to profound sedation, respiratory depression, coma, and death. Therapy with tramadol should be administered cautiously (and only when alternative treatment options are inadequate) in patients who might be prone to acute alcohol intake. Dosages and durations should be limited to the minimum required and patients should be monitored for signs and symptoms of respiratory depression and sedation. Prescribing naloxone for the emergency treatment of opioid overdose should be considered; naloxone will reverse some, but not all, symptoms caused by overdosage with tramadol, but it also increases the risk of seizures.
Tramadol (applies to Seglentis) drug dependence
Major Potential Hazard, High plausibility. Applicable conditions: Alcoholism, Drug Abuse/Dependence, Depression, History - Psychiatric Disorder
Tramadol exposes patients and other users to the risks of addiction, abuse, and misuse. Each patient's risk should be assessed before prescribing tramadol, and all patients should be monitored regularly for development of such behaviors and conditions. Risks are increased in patients with personal or family history of substance abuse (including drug or alcohol abuse or addiction) or mental illness (e.g., major depression); the potential for such risks should not prevent proper pain management in any given patient. Patients at increased risk may be prescribed tramadol, but use in such patients requires intensive counseling about the risks and proper use of tramadol, as well as intensive monitoring for signs of addiction, abuse, and misuse; prescribing naloxone for the emergency treatment of opioid overdose should be considered.
Opioids are sought by drug abusers and patients with addiction disorders and are subject to criminal diversion. These risks should be considered when prescribing or dispensing tramadol. Strategies to reduce such risks include prescribing the smallest appropriate quantity and advising the patient about proper disposal of unused drug.
Tramadol (applies to Seglentis) respiratory depression
Major Potential Hazard, Moderate plausibility. Applicable conditions: Pulmonary Impairment, Altered Consciousness, Asphyxia, Brain/Intracranial Tumor, Cerebral Vascular Disorder, Head Injury, Respiratory Arrest, Cachexia, Cor Pulmonale
Tramadol is contraindicated in patients with significant respiratory depression. Serious, life-threatening, or fatal respiratory depression may occur with tramadol. Patients should be monitored closely for respiratory depression, especially within the first 24 to 72 hours of initiating therapy and after a dosage increase.
The use of tramadol in patients with acute or severe bronchial asthma in an unmonitored setting or without resuscitative equipment is contraindicated. Tramadol-treated patients with significant chronic obstructive pulmonary disease or cor pulmonale, and those with substantially decreased respiratory reserve, hypoxia, hypercapnia, or preexisting respiratory depression are at increased risk of decreased respiratory drive (including apnea), even at recommended dosages of tramadol. In patients who may be susceptible to the intracranial effects of carbon dioxide (CO2) retention (e.g., those with evidence of increased intracranial pressure or brain tumors), tramadol may reduce respiratory drive, and the resulting CO2 retention can further increase intracranial pressure; these patients should be monitored for signs of sedation and respiratory depression, especially when starting tramadol.
Life-threatening respiratory depression is more likely to occur in elderly, cachectic, or debilitated patients as they may have altered pharmacokinetics (or altered clearance) compared to younger, healthier patients. These patients should be monitored closely, especially when starting and titrating tramadol and when coadministering with other drugs that depress respiration; alternatively, the use of nonopioid analgesics should be considered.
NSAIDs (applies to Seglentis) anemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Bleeding
Anemia has been reported in patients treated with nonsteroidal anti-inflammatory drugs (NSAIDs). This may be due to fluid retention, occult/gross blood loss, or an incompletely described effect on erythropoiesis. Hemoglobin or hematocrit should be monitored in patients with any signs/symptoms of anemia or blood loss, especially during long-term therapy. NSAIDs may increase risk of bleeding events; comorbid conditions (e.g., coagulation disorders; concomitant use of warfarin/other anticoagulants, antiplatelet agents, serotonin/serotonin norepinephrine reuptake inhibitors) may increase this risk, and patients with these conditions should be monitored for signs of bleeding. Therapy with NSAIDs should be administered cautiously in patients with or predisposed to anemia. Clinical monitoring of hematopoietic function may be appropriate, particularly during chronic therapy.
NSAIDs (applies to Seglentis) hepatotoxicity
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Liver Disease
Therapy with nonsteroidal anti-inflammatory drugs (NSAIDs) should be administered cautiously in patients with preexisting liver disease. Periodic monitoring of liver function is recommended during prolonged therapy. NSAIDs are also highly protein-bound and some are extensively metabolized by the liver. Metabolic activity and/or plasma protein binding may be altered in patients with hepatic impairment. A dosage reduction may be required in some cases.
NSAIDs (applies to Seglentis) hyperkalemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Renal Dysfunction
Increases in serum potassium concentration (including hyperkalemia) have been reported with use of nonsteroidal anti-inflammatory drugs (NSAIDs), even in some patients without renal impairment. In patients with normal renal function, these effects have been attributed to a hyporeninemic-hypoaldosteronism state. Caution is advised in patients with hyperkalemia.
Tramadol (applies to Seglentis) gastrointestinal conditions
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Biliary Obstruction, Gallbladder Disease, Pancreatitis
Tramadol may cause spasm of the sphincter of Oddi. Opioids may increase serum amylase. Patients with biliary tract disease (including acute pancreatitis) should be monitored for worsening symptoms.
Tramadol (applies to Seglentis) hypoglycemia
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Diabetes Mellitus
Cases of tramadol-associated hypoglycemia have been reported, some resulting in hospitalization. In most cases, patients had predisposing risk factors (e.g., diabetes); caution is recommended in these patients. If hypoglycemia is suspected, blood glucose levels should be monitored and discontinuation of therapy should be considered as appropriate.
Tramadol (applies to Seglentis) hypotension
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Dehydration, Shock
Tramadol may cause severe hypotension (including orthostatic hypotension, syncope) in ambulatory patients. Risk is increased in patients whose ability to maintain blood pressure has already been compromised by reduced blood volume or coadministration of certain CNS depressant drugs; these patients should be monitored for signs of hypotension after starting or titrating tramadol. In patients with circulatory shock, tramadol may cause vasodilation that can further reduce cardiac output and blood pressure; tramadol should be avoided in patients with circulatory shock.
Tramadol (applies to Seglentis) intracranial pressure
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Head Injury, Intracranial Hypertension
Opioids may obscure the clinical course in a patient with a head injury. The use of tramadol should be avoided in patients with impaired consciousness or coma.
Tramadol (applies to Seglentis) liver disease
Moderate Potential Hazard, High plausibility.
Tramadol is converted by the liver to several metabolites, one of which (referred to as M1) is pharmacologically active and a more potent analgesic than tramadol itself. The metabolism of both tramadol and M1 has been shown to decrease in patients with advanced cirrhosis of the liver, resulting in increased exposure to tramadol as well as substantially prolonged elimination half-lives for both tramadol and M1. Therapy with tramadol should be administered cautiously in patients with liver dysfunction. In patients with severe liver dysfunction, dosage reduction is recommended with the immediate-release formulations, while the extended-release formulations should not be used.
Tramadol (applies to Seglentis) renal dysfunction
Moderate Potential Hazard, High plausibility.
Tramadol and its metabolites, one of which (referred to as M1) is pharmacologically active and a more potent analgesic than tramadol itself, are primarily excreted in the urine. The rate and extent of excretion of both tramadol and M1 have been shown to decrease in patients with impaired renal function. Therapy with tramadol should be administered cautiously in such patients. In patients with CrCl less than 30 mL/min, dosage reduction is recommended with the immediate-release formulations, while the extended-release formulations should not be used.
Tramadol (applies to Seglentis) seizure disorders
Moderate Potential Hazard, High plausibility. Applicable conditions: Alcoholism, Drug Abuse/Dependence, CNS Disorder
Seizures have been reported in patients receiving tramadol within the recommended dosage range. The risk appears to increase with doses above the recommended range and with concomitant use of certain drugs (e.g., those that reduce the seizure threshold). Risk of seizure may also increase in patients with epilepsy, those with a history of seizures, or in patients with a recognized risk for seizure (e.g., head trauma, metabolic disorders, alcohol and drug withdrawal, CNS infections). In tramadol overdose, naloxone administration may increase the risk of seizures.
Tramadol (applies to Seglentis) suicidal
Moderate Potential Hazard, Moderate plausibility. Applicable conditions: Depression, Alcoholism, Psychosis
Tramadol should not be prescribed for patients who are suicidal or addiction-prone. The use of nonnarcotic analgesics should be considered for patients who are suicidal or depressed. Tramadol should be prescribed with caution for patients with history of misuse and/or are currently taking CNS-active drugs, antidepressant drugs, alcohol in excess, and patients who suffer from emotional disturbance or depression. Patients should be advised not to exceed the recommended dose and to limit their intake of alcohol.
Switch to professional interaction data
Seglentis drug interactions
There are 993 drug interactions with Seglentis (celecoxib / tramadol).
Seglentis alcohol/food interactions
There are 2 alcohol/food interactions with Seglentis (celecoxib / tramadol).
More about Seglentis (celecoxib / tramadol)
- Seglentis consumer information
- Check interactions
- Compare alternatives
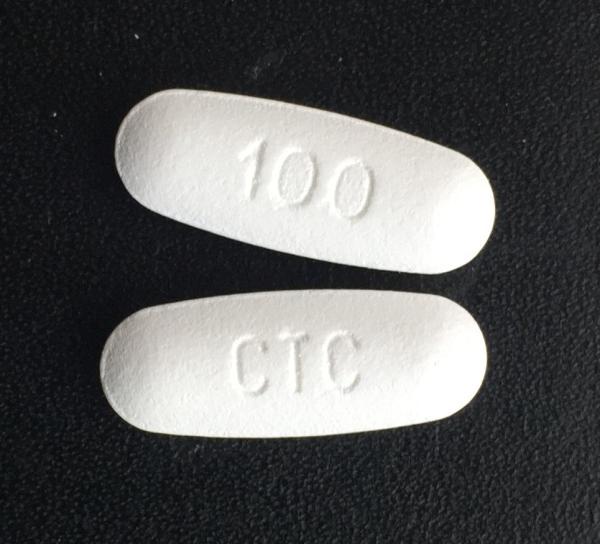
- Drug images
- Side effects
- Dosage information
- During pregnancy
- FDA approval history
- Drug class: narcotic analgesic combinations
- En español
Related treatment guides
Drug Interaction Classification
| Highly clinically significant. Avoid combinations; the risk of the interaction outweighs the benefit. | |
| Moderately clinically significant. Usually avoid combinations; use it only under special circumstances. | |
| Minimally clinically significant. Minimize risk; assess risk and consider an alternative drug, take steps to circumvent the interaction risk and/or institute a monitoring plan. | |
| No interaction information available. |
See also:
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.