Glyset (Oral)
Generic name: miglitol [ MIG-li-tol ]
Drug class: Alpha-glucosidase inhibitors
Medically reviewed by Drugs.com. Last updated on Oct 8, 2024.
Uses for Glyset
Miglitol is used to treat high blood sugar levels that are caused by type 2 diabetes. Normally, after you eat, your pancreas releases insulin to help your body store excess sugar for later use. This process occurs during normal digestion of food. In type 2 diabetes, your body does not work properly to store the excess sugar and the sugar remains in your bloodstream. Having high blood sugar can lead to serious health problems in the future. Proper diet is the first step in managing type 2 diabetes but often medicines are needed to help your body. Miglitol is a medicine that slows the digestion of sugars so your body has time to store extra sugar. Sometimes another medicine called sulfonylurea can be used in combination with miglitol to help your body store more sugar.
This medicine is available only with your doctor's prescription.
Before using Glyset
In deciding to use a medicine, the risks of taking the medicine must be weighed against the good it will do. This is a decision you and your doctor will make. For this medicine, the following should be considered:
Allergies
Tell your doctor if you have ever had any unusual or allergic reaction to this medicine or any other medicines. Also tell your health care professional if you have any other types of allergies, such as to foods, dyes, preservatives, or animals. For non-prescription products, read the label or package ingredients carefully.
Pediatric
Studies on this medicine have been done only in adult patients, and there is no specific information comparing use of miglitol in children with use in other age groups.
Geriatric
This medicine has been tested and has not been shown to cause different side effects or problems in older people than it does in younger adults.
Breast Feeding
There are no adequate studies in women for determining infant risk when using this medication during breastfeeding. Weigh the potential benefits against the potential risks before taking this medication while breastfeeding.
Interactions with Medicines
Although certain medicines should not be used together at all, in other cases two different medicines may be used together even if an interaction might occur. In these cases, your doctor may want to change the dose, or other precautions may be necessary. When you are taking this medicine, it is especially important that your healthcare professional know if you are taking any of the medicines listed below. The following interactions have been selected on the basis of their potential significance and are not necessarily all-inclusive.
Using this medicine with any of the following medicines is usually not recommended, but may be required in some cases. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Abiraterone Acetate
- Chloroquine
- Chlorothiazide
- Chlorthalidone
- Ciprofloxacin
- Delafloxacin
- Enoxacin
- Furosemide
- Gatifloxacin
- Gemifloxacin
- Grepafloxacin
- Hydrochlorothiazide
- Hydroflumethiazide
- Hydroxychloroquine
- Indapamide
- Insulin
- Insulin Aspart, Recombinant
- Insulin Bovine
- Insulin Degludec
- Insulin Detemir
- Insulin Glargine, Recombinant
- Insulin Glulisine
- Insulin Lispro, Recombinant
- Lanreotide
- Levofloxacin
- Lomefloxacin
- Metolazone
- Moxifloxacin
- Norfloxacin
- Octreotide
- Ofloxacin
- Pasireotide
- Polythiazide
- Pramlintide
- Somatrogon-ghla
- Sparfloxacin
- Thioctic Acid
- Triamterene
- Trovafloxacin
Using this medicine with any of the following medicines may cause an increased risk of certain side effects, but using both drugs may be the best treatment for you. If both medicines are prescribed together, your doctor may change the dose or how often you use one or both of the medicines.
- Acebutolol
- Atenolol
- Betaxolol
- Bisoprolol
- Bitter Melon
- Carteolol
- Carvedilol
- Celiprolol
- Digoxin
- Esmolol
- Glucomannan
- Guar Gum
- Labetalol
- Levobunolol
- Metipranolol
- Metoprolol
- Nadolol
- Nebivolol
- Oxprenolol
- Penbutolol
- Pindolol
- Practolol
- Propranolol
- Psyllium
- Sotalol
- Timolol
Interactions with Food/Tobacco/Alcohol
Certain medicines should not be used at or around the time of eating food or eating certain types of food since interactions may occur. Using alcohol or tobacco with certain medicines may also cause interactions to occur. Discuss with your healthcare professional the use of your medicine with food, alcohol, or tobacco.
Other Medical Problems
The presence of other medical problems may affect the use of this medicine. Make sure you tell your doctor if you have any other medical problems, especially:
- Digestion problems or
- Inflammatory bowel disease or
- Intestinal blockage or
- Other intestinal problems—Miglitol should not be used
- Kidney disease—Higher levels of miglitol may result and a smaller dose may be needed
Proper use of Glyset
Follow carefully the special meal plan you doctor gave you. This is the most important part of controlling your condition, and is necessary if the medicine is to work properly. Also, exercise regularly and test for sugar in your blood or urine as directed.
For this medicine to work properly it should be taken with the first bite of each main meal.
Dosing
The dose of this medicine will be different for different patients. Follow your doctor's orders or the directions on the label. The following information includes only the average doses of this medicine. If your dose is different, do not change it unless your doctor tells you to do so.
The amount of medicine that you take depends on the strength of the medicine. Also, the number of doses you take each day, the time allowed between doses, and the length of time you take the medicine depend on the medical problem for which you are using the medicine.
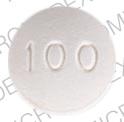
- For oral dosage form (tablets):
- For type 2 diabetes:
- Adults—At first the dose is 25 milligrams (mg) three times a day, at the start (with the first bite) of each main meal. After four to eight weeks, your doctor may increase your dose to 50 mg three times a day. Then, after an additional twelve weeks, if necessary, your doctor may increase your dose to 100 mg three times a day.
- Children—Use and dose must be determined by your doctor.
- For type 2 diabetes:
Missed Dose
If you miss a dose of this medicine, skip the missed dose and go back to your regular dosing schedule. Do not double doses.
Storage
Store the medicine in a closed container at room temperature, away from heat, moisture, and direct light. Keep from freezing.
Keep out of the reach of children.
Do not keep outdated medicine or medicine no longer needed.
Ask your healthcare professional how you should dispose of any medicine you do not use.
Precautions while using Glyset
Your doctor will want to check your progress at regular visits, especially during the first few weeks that you take this medicine.
It is very important to follow carefully any instructions from your health care team about:
- Alcohol—Drinking alcohol may cause severe low blood sugar. Discuss this with your health care team.
- Other medicines—Do not take other medicines during the time you are taking miglitol unless they have been discussed with your doctor. This especially includes nonprescription medicines such as aspirin, and medicines for appetite control, asthma, colds, cough, hay fever, or sinus problems.
- Counseling—Other family members need to learn how to prevent side effects or help with side effects if they occur. Also, patients with diabetes may need special counseling about diabetes medicine dosing changes that might occur because of lifestyle changes, such as changes in exercise and diet. Furthermore, counseling on contraception and pregnancy may be needed because of the problems that can occur in patients with diabetes during pregnancy.
- Travel—Keep a recent prescription and your medical history with you. Be prepared for an emergency as you would normally. Make allowances for changing time zones and keep your meal times as close as possible to your usual meal times.
In case of emergency—There may be a time when you need emergency help for a problem caused by your diabetes. You need to be prepared for these emergencies. It is a good idea to wear a medical identification (ID) bracelet or neck chain at all times. Also, carry an ID card in your wallet or purse that says that you have diabetes and a list of all your medicines.
Symptoms of hypoglycemia (low blood sugar) include anxiety; behavior change similar to being drunk; blurred vision; cold sweats; confusion; cool, pale skin; difficulty in thinking; drowsiness; excessive hunger; fast heartbeat; headache (continuing); nausea; nervousness; nightmares; restless sleep; shakiness; slurred speech; or unusual tiredness or weakness.
Miglitol does not cause low blood sugar. However, it can occur if you delay or miss a meal or snack, drink alcohol, exercise more than usual, cannot eat because of nausea or vomiting, or take miglitol with another type of diabetes medicine. Symptoms of low blood sugar must be treated before they lead to unconsciousness (passing out). Different people feel different symptoms of low blood sugar. It is important that you learn which symptoms of low blood sugar you usually have so that you can treat it quickly.
If symptoms of low blood sugar occur, eat glucose tablets or gel or honey, or drink fruit juice to relieve the symptoms. Table sugar (sucrose) or regular (nondiet) soft drinks will not work. Also, check your blood for low blood sugar. Glucagon is used in emergency situations when severe symptoms such as seizures (convulsions) or unconsciousness occur. Have a glucagon kit available, along with a syringe or needle, and know how to use it. Members of your household also should know how to use it.
Symptoms of hyperglycemia (high blood sugar) include blurred vision; drowsiness; dry mouth; flushed, dry skin; fruit-like breath odor; increased urination; ketones in urine; loss of appetite; stomachache, nausea, or vomiting; tiredness; troubled breathing (rapid and deep); unconsciousness; or unusual thirst.
High blood sugar may occur if you do not exercise as much as usual, have a fever or infection, do not take enough or skip a dose of your diabetes medicine, or overeat or do not follow your meal plan.
If symptoms of high blood sugar occur, check your blood sugar level and then call your health care professional for instructions.
Side Effects of Glyset
Some side effects may occur that usually do not need medical attention. These side effects may go away during treatment as your body adjusts to the medicine. Also, your health care professional may be able to tell you about ways to prevent or reduce some of these side effects. Check with your health care professional if any of the following side effects continue or are bothersome or if you have any questions about them:
More common
- Bloated full feeling
- excess air or gas in stomach or intestines
- increase in bowel movements
- loose stools
- passing gas
- soft stools
- stomach or abdomen pain
Less common
- Skin rash
Other side effects not listed may also occur in some patients. If you notice any other effects, check with your healthcare professional.
Call your doctor for medical advice about side effects. You may report side effects to the FDA at 1-800-FDA-1088.
Related/similar drugs
Commonly used brand name(s)
In the U.S.
- Glyset
Available Dosage Forms:
- Tablet
Therapeutic Class: Hypoglycemic
Pharmacologic Class: Alpha-Glucosidase Inhibitor
More about Glyset (miglitol)
- Check interactions
- Compare alternatives
- Drug images
- Side effects
- Dosage information
- During pregnancy
- Generic availability
- Drug class: alpha-glucosidase inhibitors
- Breastfeeding
Patient resources
Professional resources
Related treatment guides
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.