Uterine Artery Embolization for Fibroids
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about uterine artery embolization (UAE) for fibroids:
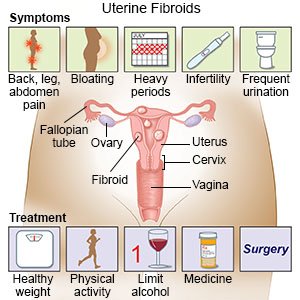
UAE is a procedure to make fibroids smaller. Embolization means creating a clot, or block, in a blood vessel. Your healthcare provider will block an artery that supplies blood to the fibroid. The fibroid will not be gone but it will get smaller. This may decrease symptoms fibroids can cause. This procedure may also be called uterine fibroid embolization.
 |
How to prepare for the procedure:
- Your provider will tell you how to prepare for this procedure. Your provider may tell you not to eat or drink anything after midnight before your procedure. Arrange to have someone drive you home and stay with you after your procedure.
- Give your provider a list of your medicines, including any herbs or supplements. Your provider will tell you if you need to stop any medicine for your procedure, and when to stop. Your provider will tell you which medicines to take or not take on the day of your procedure. Tell your provider about any allergies you have, including to medicines or anesthesia.
- Tell your provider if you know or think you are pregnant. This procedure cannot be done while you are pregnant.
- Tell your provider if you have an intrauterine device (IUD). Your IUD may need to be removed before your procedure.
- You may need blood tests, urine tests, or an MRI. These tests will help your provider plan for your procedure. You may be given contrast liquid to help your uterus show up better in the pictures. Tell the healthcare provider if you have ever had an allergic reaction to contrast liquid. Do not enter the MRI room with anything metal. Metal can cause serious injury. Tell the healthcare provider if you have any metal in or on your body.
What will happen during the procedure:
- You may be given medicine to help you relax. You may instead be given general anesthesia to keep you asleep. A local anesthetic is given in your wrist or groin where a small incision will be made. With local anesthesia, you may still feel pressure or pushing, but you should not feel pain.
- Your provider will insert a small catheter (thin tube) into an artery near your wrist or groin. The catheter is slowly moved into the uterine artery. Your provider may use an x-ray with contrast liquid to help guide the catheter to the uterine artery. You may feel warm as the contrast liquid is put into the catheter.
- Your provider will put embolization liquid into the uterine artery. This liquid blocks blood flow to the fibroid. Your provider may be able to treat more than one fibroid during this procedure. Your provider will then remove the catheter. Your provider will cover the incision with a bandage and apply pressure to the area. This will help stop bleeding and keep the area from getting infected. The incision may be small and close on its own.
What to expect after the procedure:
You will be taken to a recovery room until you are fully awake. Healthcare providers will monitor you closely for any problems. You may have to lie in one position for a certain amount of time. Do not get up until healthcare providers say it is okay. You may be able to go home when your pain is controlled, or you may need to spend the night in the hospital. You may have bleeding or discharge from your vagina for up to 1 month.
Risks of UAE for fibroids:
- You may bleed more than expected or develop an infection. Your arteries may be damaged from the catheter, or you may develop a blood clot. Your kidneys may be damaged from the contrast liquid. Your uterus may be damaged, and it may need to be removed. You may develop an abscess (pocket of pus) in your uterus. You may develop a urinary tract infection (UTI) or have trouble urinating. Your symptoms may not go away. The fibroid may grow back. A fibroid may detach from your uterus. You may need another procedure to remove all the pieces of the fibroid.
- Your risk for a caesarian section (C-section) or miscarriage will increase if you get pregnant. You may bleed heavily after you deliver a baby. If you are older than 45, embolization may cause menopause to start. Your ovarian arteries may need to be blocked. Your ovaries may not work after this. You may have trouble getting pregnant. Your monthly periods may stop.
Seek care immediately if:
- You have a fever along with pain and nausea lasting longer than 3 days.
- You have increasing abdominal pain or pressure.
- You have heavy vaginal bleeding that soaks 1 pad in 1 hour for 2 hours in a row.
- You cannot urinate, or you urinate very little.
- You have foul-smelling vaginal discharge.
- You have a fever higher than 100.4°F (38°C).
- You have signs of an infection at the incision area, such as redness or swelling.
Related medications
Call your doctor or gynecologist if:
- You have pain or vaginal discharge that continues for longer than 1 month.
- You bleed more than usual during your monthly periods.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Nausea medicine may help calm your stomach and prevent vomiting.
- NSAIDs help decrease swelling and pain or fever. This medicine is available with or without a doctor's order. NSAIDs can cause stomach bleeding or kidney problems in certain people. If you take blood thinner medicine, always ask your healthcare provider if NSAIDs are safe for you. Always read the medicine label and follow directions.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
Watch for symptoms of postembolization syndrome:
This syndrome is common after an embolization procedure. It usually starts within 72 hours of the procedure and may last a few days. Common symptoms are fever, pain, and nausea. You should be able to manage your symptoms at home. Acetaminophen or an NSAID, such as ibuprofen, can decrease a fever and pain. Eat small meals with bland foods and take medicine as directed, to help decrease your nausea. Drink liquids as directed by your provider.
Care for your incision area as directed:
Carefully wash around the area with soap and water. Gently dry the area and put on new, clean bandages as directed. Change your bandages when they get wet or dirty. If you have strips of medical tape, let them fall off on their own. Look for signs of infection, such as redness or swelling.
Self-care:
- Rest as needed. Rest and sleep will help your body heal. You may be more tired than usual for 7 to 10 days. It will take a few months for the fibroid to break down.
- Follow your healthcare provider's instructions for activity. Your provider will tell you when you can return to your normal activities and start driving. This is usually in 1 to 3 weeks.
- Do not have sex, use tampons, douche, or take a bath until your provider says it is okay. Do not go in pools or hot tubs for as long as directed. These may cause an infection in your uterus. It is okay to shower after the procedure.
- Check your vaginal discharge for changes. Look for any change in the color, amount, or smell. Foul-smelling discharge may mean you have an infection or a fibroid has detached from your uterus. You will need immediate treatment if this happens.
Follow up with your doctor or gynecologist as directed:
You will need regular MRIs to check that your uterus and fibroid are getting smaller. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
