Robot Assisted Laparoscopic Prostatectomy
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
What you need to know about robot-assisted laparoscopic prostatectomy (RALP):
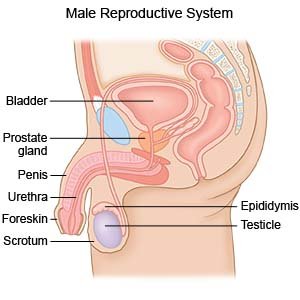
RALP is surgery to remove your prostate gland through small incisions in your abdomen. RALP is done with a machine that is controlled by your surgeon. The machine has mechanical arms that use small tools to remove your prostate.
 |
How to prepare for RALP:
- Your surgeon will tell you how to prepare. Tell him or her about any other surgeries or cancer treatments you had. Tell him or her if you have had bleeding problems.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine before surgery, and when to stop.
- Tell your surgeon about any allergies you have. Include allergic reactions to medicine, antibiotics, or anesthesia. You may need to take antibiotic medicine to help prevent an infection caused by bacteria. You may get antibiotic medicine before and after your surgery.
- Arrange to have someone drive you home after surgery and stay with you for 24 hours.
- You may need to have tests done before surgery, such as blood tests or a chest x-ray.
- You may have to stop eating solid food for up to 2 days before your surgery. You can drink water, broth, apple juice, or lemon-lime soft drinks. You may also suck on ice chips or eat gelatin. You may be given medicine to drink or an enema to clean out your bowel.
What will happen during RALP:
- A urinary catheter will be put into your bladder to drain your urine. The robotic arms place a laparoscope and other tools inside your abdomen through small cuts. A laparoscope is a long, thin tube with a light and camera on the end. A gas called carbon dioxide is pumped into your abdomen to inflate it. This gives your surgeon room so he or she can see your prostate better.
- Your surgeon will use the camera to see inside your abdomen. He or she will guide the robotic arms to remove the prostate. The prostate will be removed through one of the small incisions in your abdomen. Lymph nodes may also be removed. Your surgeon will use the robotic arms to stitch your incisions closed.
What to expect after RALP:
- Drains (thin rubber tubes) may be used to drain fluid from around your incision. The drains will be taken out when the surgery area stops draining.
- A Foley catheter is a thin tube inserted through your urethra and moved into your bladder. The catheter is used to drain urine into a bag. Healthcare providers will remove the catheter when you no longer need it.
Risks of RALP:
- You may bleed more than expected or get an infection. Your bladder, ureters (tubes that drain urine from your body), intestines, or rectum could be damaged during surgery. After RALP, you may have problems urinating or having bowel movements. You may need more surgery to treat urination problems. You may not be able to have an erection after surgery. Your stitches may come apart. You may have a hernia or develop an abscess (deep infection).
- You may get a blood clot in your arm or leg. The clot may travel to your heart or brain and cause life-threatening problems, such as a heart attack or stroke. Even with surgery, cancer may come back.
Call your local emergency number (911 in the US) for any of the following:
- You have chest pain when you take a deep breath or cough. You cough up blood.
- You suddenly feel lightheaded and short of breath.
Related medications
Call your surgeon or uro-oncologist if:
- Your arm or leg feels warm, tender, and painful. It may look swollen and red.
- You have more blood in your urine than you were told to expect, or you pass a blood clot.
- You have an upset stomach or are vomiting.
- You have painful swelling in your abdomen that does not go away.
- You have a fever.
- Your pain is getting worse, even with medicine.
- You have an incision that is red, swollen, or has pus coming from it.
- You are urinating less than usual.
- You have trouble urinating or having a bowel movement.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Antibiotics prevent or fight an infection caused by bacteria.
- Blood thinners help prevent blood clots. Clots can cause strokes, heart attacks, and death. Many types of blood thinners are available. Your healthcare provider will give you specific instructions for the type you are given. The following are general safety guidelines to follow while you are taking a blood thinner:
- Watch for bleeding and bruising. Watch for bleeding from your gums or nose. Watch for blood in your urine and bowel movements. Use a soft washcloth on your skin, and a soft toothbrush to brush your teeth. This can keep your skin and gums from bleeding. If you shave, use an electric shaver. Do not play contact sports.
- Tell your dentist and other healthcare providers that you take a blood thinner. Wear a bracelet or necklace that says you take this medicine.
- Do not start or stop any other medicines or supplements unless your healthcare provider tells you to. Many medicines and supplements cannot be used with blood thinners.
- Take your blood thinner exactly as prescribed by your healthcare provider. Do not skip a dose or take less than prescribed. Tell your provider right away if you forget to take your blood thinner, or if you take too much.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Surgery area care:
Follow your surgeon's directions on how to care for the area. Ask when you can start showering or bathing. You may need to keep the area covered so it does not get wet.
Foley catheter care:
Keep the bag below your waist. If the bag is too high, urine will flow back into your bladder. This can cause an infection. Do not pull on the catheter. This may cause pain and bleeding, and the catheter may come out. Do not let the catheter tubing kink or twist. A kink or twist will block the flow of urine.
Bladder control:
After surgery, you may leak urine and have trouble controlling when you urinate. The following can help decrease or manage urine leakage:
- Do not have caffeine. Caffeine can cause problems with bladder control and increase your need to urinate.
- Limit liquids. Drink smaller amounts of liquid throughout the day. Do not drink before bedtime. Ask if you should decrease the amount of liquid you drink each day. This may help you control your bladder.
- Wear a pad or adult diapers, if needed. These may help to absorb leaking urine and decrease odor.
- Do pelvic floor muscle exercises. Pelvic floor muscle exercises, also called Kegels, may help improve your bladder control. These exercises are done by tightening and relaxing your pelvic muscles. Ask how to do pelvic floor muscle exercises, and how often to do them.
Self-care:
- Rest as needed. You may feel like resting more after surgery. Slowly start to do more each day.
- Ask when it is okay to return to your normal daily activities. You may need to wait 4 to 6 weeks after surgery. Your healthcare provider will tell you about the activities you should avoid after your surgery. These may include driving while you are taking pain medicines or until your catheter is removed. You may also be given a weight restriction on lifting objects.
- Walk when your healthcare provider says more activity is okay. Walking is an important activity to help with your recovery after surgery. Walking is a good way to improve your overall health and help you recover sooner. It also helps keep your blood flowing and reduces the risk of blood clots. Other types of exercise can also be an important part of your recovery. Ask about the exercises that are safe for you.
- Ask when it is okay to start having sex again. You may have trouble having an erection. Your erections may return with time. Medicines and mechanical aids may help. Talk to your healthcare provider about these options.
Follow up with your surgeon or uro-oncologist in 1 week or as directed:
You will need your urinary catheter removed. Tests will show if any cancer remains in your body after surgery. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
