Oral Lesion Excision
Medically reviewed by Drugs.com. Last updated on Aug 4, 2025.
AMBULATORY CARE:
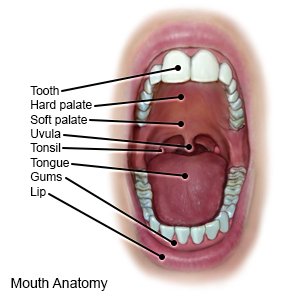
An oral lesion excision
is surgery to remove a sore, ulcer, or patch (lesion) from inside your mouth. This includes the inner lip or cheek lining, gums, tongue, and floor and roof of the mouth. Removal may be the only treatment needed for the lesion, or may be part of your treatment plan.
 |
How to prepare for surgery:
- Your surgeon will tell you how to prepare. He or she may tell you not to eat or drink anything after midnight on the day before surgery. Arrange to have someone drive you home after you are discharged.
- Tell your surgeon about all medicines you currently take. He or she will tell you if you need to stop any medicine for surgery, and when to stop. He or she will tell you which medicines to take or not take on the day of surgery.
- Tell your surgeon about all your allergies, including antibiotics or anesthesia.
What will happen during surgery:
- You may be given general anesthesia to keep you asleep and free from pain during surgery. You may instead be given local anesthesia to numb the surgery area. You will be awake with local anesthesia, but you should not feel pain.
- Your surgeon may use a knife or laser to cut the lesion away. He or she will remove tissue that looks healthy from around and under the lesion. This helps make sure that as much of the lesion as possible is removed. Your surgeon may have the lesion tested to find out if it is benign (not cancer) or malignant (cancer).
- The area where the lesion was removed may need to be closed with stitches. This depends on where it was and how large an area was removed. Medicine may be put on the area to control bleeding. Gauze bandages may be packed over the area to keep it clean and prevent more bleeding.
What to expect after surgery:
- You may have some bleeding, redness, or swelling near the surgery area. These are expected and should get better within a day or two.
- You may have trouble opening your mouth fully for a few days after surgery.
Risks of an oral lesion excision:
You may bleed more than expected or develop an infection. Depending on where the lesion is, removal may cause nerve damage. Your surgeon may not be able to remove all of the unhealthy tissue. Even with surgery, you may develop another oral lesion. Cancer cells may still spread or come back. You may have scarring from where the skin tissue was removed.
Call your local emergency number (911 in the US) if:
- You have trouble breathing.
Related medications
Seek care immediately if:
- You are bleeding more than you were told to expect, even when you apply pressure.
- You have trouble swallowing.
- You have sudden numbness in your face.
- You have severe pain.
- You cannot move part of your face.
Call your dentist or oral surgeon if:
- You have a fever.
- You have increased swelling, redness, or bleeding.
- You have pain that does not go away, or is not helped by pain medicines.
- You have yellow or green drainage coming out of the surgery area.
- You have trouble opening your mouth or chewing.
- You have questions or concerns about your condition or care.
Medicines:
You may need any of the following:
- Antibiotics help treat or prevent an infection caused by bacteria.
- Acetaminophen decreases pain and fever. It is available without a doctor's order. Ask how much to take and how often to take it. Follow directions. Read the labels of all other medicines you are using to see if they also contain acetaminophen, or ask your doctor or pharmacist. Acetaminophen can cause liver damage if not taken correctly.
- Prescription pain medicine may be given. Ask your healthcare provider how to take this medicine safely. Some prescription pain medicines contain acetaminophen. Do not take other medicines that contain acetaminophen without talking to your healthcare provider. Too much acetaminophen may cause liver damage. Prescription pain medicine may cause constipation. Ask your healthcare provider how to prevent or treat constipation.
- Take your medicine as directed. Contact your healthcare provider if you think your medicine is not helping or if you have side effects. Tell your provider if you are allergic to any medicine. Keep a list of the medicines, vitamins, and herbs you take. Include the amounts, and when and why you take them. Bring the list or the pill bottles to follow-up visits. Carry your medicine list with you in case of an emergency.
Self-care for the first 24 hours after surgery:
- Rest as needed after surgery. Your healthcare provider will tell you when it okay to drive and return to your daily activities. Your provider may tell you to sleep with your head and upper body elevated to keep the swelling down. You may want to use a pillow or two. Do not prop a young child's head up with pillows. A pillow might fall onto a child's face, and he or she may not be able to move it off. Ask your child's provider about how to elevate a young child's head safely.
- Keep any gauze in place as directed. This helps to control bleeding.
- Do not rinse your mouth for 24 hours, or as directed.
- Eat only soft foods and liquids for 24 hours. This helps control pain.
- Apply ice over the surgery area for 15 to 20 minutes every hour, or as directed. Ice helps with pain and swelling. Use an ice pack, or put crushed ice in a plastic bag. Cover it with a towel before you apply it to your skin. Do not apply heat for at least 24 hours after surgery. Heat will make the swelling worse.
Self-care starting 24 hours after surgery:
- Rinse your mouth gently with warm water. Your healthcare provider may want you rinse with warm salt water. Add ½ teaspoon of salt to 1 cup of warm water to make the salt water. Rinse your mouth gently 4 times each day, or as often as directed. Your provider will tell you how many days to do this.
- Apply heat over the surgery area for 15 minutes every hour, or as directed. Heat helps increase blood circulation and lowers swelling.
Manage or prevent oral lesions:
- Go to regular dental visits. Your dentist will check for and may need to fix problems with your teeth. He or she will also do routine oral cancer screenings. Have your teeth checked and cleaned 2 times each year, or as often as directed.
- Brush and floss your teeth safely. Ask when it is safe to begin brushing and flossing after surgery. Gently brush your teeth with a soft toothbrush. Brush and floss each day as often as directed after the surgery area heals. Do not use an alcohol-based mouth rinse.
- Protect your mouth if you wear braces. Some kinds of braces can irritate your gums, tongue, and inner cheeks. Use dental wax to cover any parts that poke or scrape your mouth. Talk to your dentist or orthodontist if you think the braces need to be adjusted.
- Care for your mouth if you wear dentures. It is still important to clean your gums and mouth if you wear dentures. Be extra careful when you put in or remove dentures. Try to prevent any injuries to your gums that could lead to sores or infection. Soak your dentures in denture solution at night to keep them free from bacteria.
- Do not use tobacco products. Tobacco products increase the risk for oral cancer. Ask your healthcare provider for information if you currently use tobacco products and need help to quit. E-cigarettes or smokeless tobacco still contain nicotine. Talk to your healthcare provider before you use these products.
- Do not drink alcohol. Alcohol increases the risk for mouth cancer. Alcohol can also irritate the surgery area.
- Be careful with foods and drinks that can irritate your mouth. Examples include citrus fruits (such as orange juice), and hard, salty, or crunchy foods. These can irritate your surgery area or cause new lesions. A dietitian may help to plan the best meals and snacks for you.
Follow up with your dentist or oral surgeon as directed:
You may need to return to have your stitches removed. You may need to come back for results if the lesion was sent to a lab for tests. If tests show the lesion was pre-cancer, you will need to come in over time to have it checked. You may be referred to a specialist for more tests or treatment. Write down your questions so you remember to ask them during your visits.
© Copyright Merative 2025 Information is for End User's use only and may not be sold, redistributed or otherwise used for commercial purposes.
The above information is an educational aid only. It is not intended as medical advice for individual conditions or treatments. Talk to your doctor, nurse or pharmacist before following any medical regimen to see if it is safe and effective for you.
Further information
Always consult your healthcare provider to ensure the information displayed on this page applies to your personal circumstances.
